Abstract
Purpose
To determine the value of early exome sequencing (eES) relative to the current typical care (TC) in the diagnosis of newborns with suspected severe mitochondrial disorders (MitD).
Methods
We used a decision tree–Markov hybrid to model neonatal intensive care unit (NICU)–related outcomes and costs, lifetime costs and quality-adjusted life-years among patients with MitD. Probabilities, costs, and utilities were populated using published literature, expert opinion, and the Pediatric Health Information System database. Incremental cost-effectiveness ratios (ICER) and net monetary benefits (NMB) were calculated from lifetime costs and quality-adjusted life-years for singleton and trio eES, and TC. Robustness was assessed using univariate and probabilistic sensitivity analyses (PSA). Scenario analyses were also conducted.
Results
Findings indicate trio eES is a cost-minimizing and cost-effective alternative to current TC. Diagnostic probabilities and NICU length-of-stay were the most sensitive model parameters. Base case analysis demonstrates trio eES has the highest incremental NMB, and PSA demonstrates trio eES had the highest likelihood of being cost-effective at a willingness-to-pay (WTP) of $200,000 relative to TC, singleton eES, and no ES.
Conclusion
Trio and singleton eES are cost-effective and cost-minimizing alternatives to current TC in diagnosing newborns suspected of having a severe MitD.
Similar content being viewed by others
INTRODUCTION
In the United States, serious but treatable inherited metabolic diseases are detected through state-mandated newborn screening protocols.1 However, mitochondrial disorders (MitD) may not be captured. When a diagnosis is undetermined, newborns undergo a diagnostic odyssey involving multiple tests.2 During this period, quick diagnosis is critical for patient stabilization or palliative care. Diagnosis turnaround time and accuracy also have implications for inpatient health-care resource utilization due to resource-intensive medical management. Infants with severe MitD are often admitted to the neonatal intensive care unit (NICU), incurring significant daily costs as their illness remains undiagnosed.
MitD refers to a spectrum of genetic disorders that occurs in a variety of patients, ranging from immediate onset in newborns, to later onset in adults.3 Newborns with suspected MitD tend to have a worse prognosis and shorter life expectancy than those diagnosed later in life, often presenting with a combination of symptoms ranging from seizures to cardiomyopathies and persistent metabolic disturbances.4,5 However, the hallmark of MitD, left untreated, is steady progression and increased involvement of multiple organ systems.5 Due to clinical and genetic heterogeneity, MitD clinical presentation can overlap with other diseases, leading to longer NICU length-of-stay and complicating diagnosis.4,5 Rapid diagnosis in this context is critical for making informed treatment decisions.
Currently, the MitD typical care (TC) diagnostic pathway varies depending on care setting, but often begins with clinical observation.6 Initial evaluation is followed by biochemical blood and urine screens, laboratory tests, and imaging studies such as an electrocardiogram or echocardiogram.6 Genetic studies with less resolution than exome or genome sequencing, such as microarray testing and karyotyping, are also common.7 Historically, this may then be followed by liver or muscle biopsies, which can cost upward of $5,500.7 These workups can extend the length-of-stay in the NICU by several days, adding to diagnostic uncertainty, which can lead to significant family anxiety and emotional burden, without changing medical management. Exome sequencing (ES) may offer a valuable way to quickly diagnose these patients, despite costing upward of US$5,000 to $7,000, by diagnosing patients earlier and more efficiently.8,9
Due to its precision and quick turnaround time potential, ES inclusion, both trio and singleton, earlier in the care pathway represents a decision problem for neonatologists and geneticists. Earlier diagnosis may impact inpatient care, provide more accurate and timely family counseling, facilitate palliative care decisions, or reduce futile and sometimes invasive operations for severely affected neonates (Appendix Note 1). Currently, genetic testing reimbursement is dependent on payer and hospital dynamics, limiting current sequencing applications. Evidence demonstrating earlier diagnosis value by singleton or trio early exome sequencing (eES) is necessary to convince decision makers to reimburse this diagnostic.
Several single-institution studies have found hospital cost savings tied to earlier introduction of ES as a diagnostic approach.9,10,11 While these studies provide useful data on the cost borne by hospitals, they lack key information on the societal and health-care sector benefit associated with earlier diagnoses. These studies highlight the need for a robust cost-effectiveness analysis of ES for severe inherited disorders to assess the economic value of earlier genetic testing in newborns. As a case study for understanding the clinical economics of ES, our analysis models eES relative to TC.
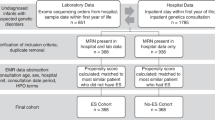
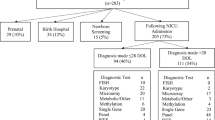
The four comparators explored here are (1) trio eES, (2) singleton eES, (3) trio TC, and (4) singleton TC (Fig. 1). TC is defined as the typical diagnostic workup for a newborn suspected of having a severe MitD, with either trio or singleton ES used as a last-line diagnostic. Singleton eES is defined as first-line ES of the newborn, leading to discharge in the event of a positive diagnosis. Trio eES is identical to singleton; however, the newborn’s parents are also tested. In the event of no diagnosis through eES, TC is the last-line diagnostic.
A decision tree is displayed here until the discharge node, where a three-state Markov model is used to model longer-term, postneonatal intensive care unit (NICU) outcomes for these patients. Nodes represent the culmination of patient care through that point. Patients that expire during their NICU stay are followed until the discharge node. No sequencing was evaluated during scenario analyses and resembles the typical care (TC) comparator arm without last-line exome sequencing.
Researchers, clinicians, payers, and decision makers are tasked with determining when to incorporate ES into the diagnostic pathway.9,12,13,14 The goal of this analysis is to address this problem through a comprehensive assessment of neonatal MitD diagnosis. Here, we present a cost-effectiveness model from both the societal and health-care sector perspectives, analyzing the value of eES relative to the current TC in diagnosing neonates suspected of having a severe MitD.
MATERIALS AND METHODS
Model structure
To model the decision problem facing clinicians presented with a critically ill newborn suspected of having a MitD, we analyzed economic and clinical outcomes associated with MitD using a hybrid decision tree and Markov model (Fig. 1, Appendix Note 2). We did not include MitD patients older than one month, as they often experience a different diagnostic odyssey and decision problem.15 We chose a model time horizon of 25 years, reflecting the maximum reported life expectancy for newborns suspected of having a severe MitD.16 All outcomes and costs were discounted at a rate of 3% per year. Cost–consequence and budget impact analyses were conducted from the health-care sector perspective. Cost–utility analysis was conducted from the societal perspective (Appendix Note 3).17
Each comparator was evaluated relative to singleton TC. Due to clinical heterogeneity of MitD, TC may vary depending on the care setting, with literature and guidelines suggesting dozens of tests.4,18 When faced with multiple, seemingly disparate disorders spanning from multiple organ system failure to developmental delay, clinicians need to be well-equipped to diagnose the varying symptoms of MitD, thus TC in this context is all-encompassing.4,5
The main differentiator between both forms of eES and TC is the length-of-stay in the NICU and the proportion of patients successfully diagnosed per arm. Since earlier diagnosis can either facilitate end-of-life care or medical management without a major improvement in outcomes relative to later diagnosis, we expect the life expectancy to be similar across all arms. In this model, we assume that a provider solely used ES as their genetic diagnostic.
Costs
Due to MitD patient clinical heterogeneity, little current research has been published on NICU resource utilization by neonates with severe MitD. However, the Pediatric Health Information System (PHIS) database provides clinical and resource utilization data for all pediatric patients admitted to more than 45 major children’s hospitals throughout the United States.19 PHIS data and sensitivity analyses capture the breadth of NICU stays in terms of length and cost (Appendix Note 4).
Inpatient stay indirect costs in the NICU are calculated as unpaid caregiver time dedicated to MitD patient care beyond that for a healthy newborn. These values were calculated using expert opinion and published literature associated with transportation and caregiver waiting time during care episodes.20 Indirect costs post-NICU discharge are calculated likewise, but are centered around home care (Table 1, Appendix Table 1, Appendix Table 2, Appendix Note 5).
Published data and literature are limited regarding long-term costs and quality of life associated with severe MitD. One hallmark of MitD symptomatology is the presence of severe neurodevelopmental deficits that lead to clinical manifestations sometimes labeled as cerebral palsy (CP).4 CP and MitD are also both chronic conditions with birth/early childhood onset and no known curative options. We used CP as a proxy for long-term costs for newborns with severe MitD, under the assumption that postdischarge costs associated with CP are like those of MitD. The direct costs associated with CP are calculated from published literature, per year of life (Table 1, Appendix Table 2).21,22,23,24
All costs are adjusted to 2019 US dollars, and foreign costs adjusted using medical goods purchasing power parity (Appendix Table 3).25
Utilities
For this model, only two health states have associated utilities: within the NICU and post-NICU. Newborns lack the ability to report health states, thus quality-of-life metrics, from the patient perspective, remain unpublished for this population. Published utility values from the parent perspective of a child in the ICU were used as a proxy for the utility of a severe MitD newborn in a level III/IV NICU. Utility values published were based on standard gamble responses (Table 1, Appendix Table 4).26 For post-NICU modeling, published utilities generated from a standard gamble response were also used (Table 1, Appendix Table 4).
Probabilities and length-of-stay
Diagnostic probability either through singleton eES, trio eES, or TC was calculated using published literature and expert opinion (Table 1). We calculated the true positive diagnostic probability as the median of several probabilities published in the current literature on the use of ES in diagnosing MitD. With continued innovations, we believe this value may be a conservative estimate of the true positive diagnostic capability for neonatal MitD. In this model, we assumed that (1) the sum of each diagnostic probability is equal to one, (2) false positives are rare during genetic sequencing based on published literature, and (3) true negative diagnoses are more common than false negative (Table 1). Values populating these parameters were validated with experts in genetic medicine and neonatology to confirm validity (See Appendix Note 6).
Each arm’s NICU length-of-stay was determined using published literature and the PHIS database. Values used to populate this model were then corroborated with expert opinion.
Transition probabilities from the NICU to discharge or death were calculated per diagnostic arm (true/false positive, true/false negative) using PHIS data, expert opinion, published literature, and assumptions where data were unavailable (Table 1). The inclusion of each possible outcome allows the model to more accurately reflect the true diagnostic capability and clinical realities of each approach and to capture the benefit of including an innovative diagnostic within TC. Likelihood of death in the NICU was calculated as 1 minus the probability of discharge. Due to the severity associated with inherited neonatal onset MitD, we assumed patients with either false positive or true negative diagnoses for MitD, indicating the patient likely had a non-MitD metabolic disorder, had a higher likelihood of surviving the NICU than patients with either a true positive or false negative diagnosis. Survival likelihood contingent on true/false positive, true false/negative drives duration in each health state.
These transition assumptions were tested using sensitivity analyses to determine robustness of findings. Since severe MitD requires significant medical management, it was assumed that patients with a false negative diagnosis were less likely to survive the NICU. After discharge from the NICU, transition probabilities from alive to death were calculated using published literature and assumptions that false positive MitD patients were likely healthier than true positive ones, and false negative patients likely much sicker than true positive (Table 1). Post-NICU Markov stages occur in yearly cycles. Probabilities of death per cycle were consistent each year (Table 1). These values were validated using expert opinion and literature (Appendix Notes 6, 7).
Patient palliative care in this model is assumed to be like current care before patient death. Due to clinical heterogeneity and the target patient population, health state utilities and cost during a palliative care state are difficult to quantify but are conservatively assumed to be like current care.
Outcomes
The primary outcomes for the analysis were the incremental cost-effectiveness ratio (ICER) and incremental net monetary benefits (iNMBs). ICERs were calculated using formula (1):
INMB is calculated as the difference in NMB between singleton eES or trio eES, and TC, using formulas (2) and (3). NMB was calculated at willingness-to-pay (WTP) thresholds of $50,000 and $200,000 per quality-adjusted life-year (QALY). $50,000 was selected as a similar proxy to the UK’s National Health Service decision-making threshold, and $200,000 was selected as an approximation of three times gross domestic product per capita, which can be used as a US proxy for WTP for one year of perfect health.27,28
All outcomes were calculated as QALYs using formula (4), and all costs were aggregated direct and indirect costs (Appendix Note 8).
Secondary outcomes included cost–consequences and budget impact analyses, calculated from the health-care sector perspective. This analysis consisted of total correct diagnoses (true positive and true negative), total NICU survival, total NICU cost per patient, cost per correct diagnosis, cost per NICU survival, and differences of secondary outcomes relative to singleton TC.
Sensitivity analyses
TC varies widely depending on the care setting. Sensitivity analyses allow us to test our model, such that multiple care settings can be considered. Univariate sensitivity testing was conducted using a ±20% range from the base case value to see which parameters had the largest effect on the ICER and iNMB. Probabilistic sensitivity analysis explored uncertainty surrounding mean parameter values by varying parameter estimates using a 2,500 trial Monte Carlo simulation.29 Within each trial, parameter values were randomly drawn from relevant probability distributions. Cost parameters were given a gamma distribution, utilities a beta distribution, length-of-stay values a log normal distribution, and transition probabilities a beta distribution.30 Where dispersion values were required, standard deviation was used. To demonstrate the proportion of simulations that favored singleton eES, trio eES over singleton, or trio TC at willingness-to pay (WTP) thresholds of $0 to $1,000,000 per QALY, a cost-effectiveness acceptability curve (CEAC) was generated. A CEAC summarizes the decision uncertainty in the cost-effectiveness analysis by showing the probability that each intervention is cost-effective over a range of different WTP thresholds per QALY.29
Expected value of perfect information (EVPI) was calculated to determine the theoretical value of removing parameter uncertainty from this model and can be interpreted as the decision maker’s WTP for perfect information regarding all factors that may impact the preferred treatment choice.31 Using results from our PSA, EVPI was calculated as the max net benefit regardless of intervention, minus the dominant intervention expected benefit. EVPI was calculated at similar WTP thresholds as NMBs.
Scenario analyses
Multiple scenario analyses were conducted to further assess ES value relative to current typical care. A fifth comparator, “No ES,” was added to compare singleton and trio eES and TC relative to no sequencing. This arm consisted of TC diagnostics only. NMBs and CEACs were generated using this fifth arm to contextualize when no sequencing may be valuable.
An additional hypothetical treatment scenario was constructed to measure how key findings might change with the introduction of a curative therapy (see Appendix Note 9). Hypothetical treatment scenario assumptions consisted of (1) patients’ treatment with a true or false positive diagnosis, (2) life extended with a US population norm health utility, and (3) all other model parameters held constant (see Appendix Note 9). Added life expectancy was varied from 1 to 15 years. Each comparator arm’s iNMBs were calculated relative to singleton ES TC and for a range of potential annual orphan medication costs with $193,324 as an upper bound limit.32
RESULTS
Cost–utility
In the base case scenario, total, nondiscounted expected life-years per patient is 2.10 years for singleton and trio eES arms, 2.03 years for the TC arm under the singleton scenario, and 2.12 years under the trio ES TC arm, consistent with life expectancies seen in patients with severe MitD observed in real world settings.5,16 Total discounted costs for the singleton eES arm is $288,308 and $330,249 for the TC arm (Table 2). Discounted costs for trio eES and the trio TC arm is $282,281 and $334,170, respectively. Total discounted expected QALYs for each arm is approximately 1.1 (Table 2). These values imply that singleton and trio eES dominate current TC practices for diagnosing patients with severe MitD because they provide equivalent QALYs at a lower cost. iNMB of singleton eES compared to singleton TC at a WTP of $200,000 and $50,000 were also calculated to be $45,387 and $42,802, respectively (Table 2). We observed iNMBs of $49,826 and $48,432 at WTPs of $200,000 and $50,000 among trio eES relative to singleton TC.
Budget impact and cost–consequence analyses
MitD patient NICU outcomes, predischarge, are better for patients in the eES singleton and trio arms. More patients are correctly diagnosed and more survive the NICU relative to singleton TC (Table 2). Total NICU cost per patient, cost per correct diagnosis, and cost per NICU survivor as observed from the health-care perspective are less costly for both eES arms relative to both TC arms. Trio eES has the lowest total NICU cost difference relative to singleton TC, lowest cost per correct diagnosis, and lowest cost per NICU survivor compared to each of the other arms at -$49,849, -$112,394, and -$95,158 respectively (Table 2). These analyses are primarily driven by more correct diagnoses, greater NICU survival, and lower costs for eES arms relative to TC arms. Earlier diagnosis by singleton and trio eES contributes to shorter NICU length-of-stay and thus fewer health care–associated expenses.
One-way and probabilistic sensitivity analyses
The parameters with largest effects on ICER and iNMB at the $200,000 and $50,000 WTP thresholds were the likelihoods of true positive diagnoses in both arms (TC and eES), length-of-stay in the NICU regardless of true/false positive/negative diagnostic rates, discharge or death likelihood following an initial unconfirmed diagnosis, and unconfirmed diagnosis likelihood following either eES or TC (Fig. 2). Key results were robust to univariate sensitivity analysis.
Unless otherwise indicated, all key parameters being adjusted are days spent in neonatal intensive care unit (NICU) per branch due to either true positive, true negative, false positive, or false negative per comparator arm. Red line indicates an incremental net monetary benefit (iNMB) of $0. Dx diagnosis. Full tornado diagrams can be found in Appendix Fig. 1.
Probabilistic sensitivity analysis confirms base case results at each WTP from US$0 to $1,000,000. At a $0 WTP, trio eES is the most cost-effective comparator in 58% of simulations. However, singleton eES becomes the best option as WTP threshold increases beyond $500,000. Figure 3 and Appendix Fig. 2 exhibit Monte Carlo simulations projected to a cost-effectiveness plane and the cost-effectiveness acceptability curve.
Probabilistic sensitivity analyses were completed using 2,500 Monte Carlo simulations with varying distributions depending on the parameter. The probability of each comparator being the most cost-effective is displayed here across a range of willingness-to-pay (WTP) thresholds. Trio early exome sequencing (eES) is consistently the most cost-effective across all accepted WTP thresholds <$450,000 per quality-adjusted life-year (QALY). TC typical care, but singleton eES takes over at approximately $500,000.
Finally, EVPI was calculated according to our PSA results to determine the theoretical amount a decision maker would be willing to pay for perfect information on diagnostic outcome for three of our comparators relative to singleton TC. Singleton eES has an EVPI of $85,496 and $86,458 at a WTP of $50,000 and $200,000, trio eES has an EVPI of $69,207 and $63,107 respectively, and trio TC has an EVPI of $97,042 and $91,134, relative to singleton TC.
Scenario analyses
Relative to singleton TC, no ES was more costly, although with a positive iNMB of $6,778 and $1,135 at WTP thresholds of $200,000 and $50,000, relative to singleton TC. Total NICU cost, cost per correct diagnosis, and cost per NICU survival were also less than singleton TC (Appendix Table 5). No ES has a slightly lower probability of being a cost-effective alternative at a varying WTP threshold than singleton eES, and a higher probability of being cost-effective relative to singleton and trio TC (Fig. 3).
Under the hypothetical curative orphan drug threshold analysis, no ES has the largest iNMB relative to singleton TC, under the base conditions that expected life expectancy due to therapy increases (Appendix Figure 3a). However, as total orphan treatment cost decreases (Appendix Figure 3b–f), eES yields the greatest iNMB.
DISCUSSION
ES is an expensive genetic diagnostic with clinical promise for diagnosing newborns with rare diseases.14 This analysis evaluated the economic value of eES for the diagnosis of neonates with severe MitD. By robustly analyzing this patient population and intervention from the societal perspective, eES is shown to have a positive iNMB relative to TC, while also dominating the current TC by reducing a major driver of ill newborn costs, i.e., NICU length-of-stay. Given the results presented here, one could assume that for other genetic diseases that are difficult to diagnose through current clinical means, eES represents a cost-effective and cost-minimizing way to quickly diagnose and optimally manage patients with severe disorders. Furthermore, the breadth of identifiable illnesses through ES suggests the analyses here are conservative since other illnesses may be diagnosed in these newborns at nearly zero marginal costs. This is particularly true if parents consent to testing of the 59 genes on the American College of Medical Genetics and Genomics–established list of incidental findings.30 These include BRCA1/2, other cancer genes, cardiomyopathy genes, and more.
There are several limitations to this analysis that may be explored through threshold and scenario analyses. eES and length-of-stay costs have a large effect on this model. Establishing an appropriate neonatal cost-effectiveness threshold can help inform clinicians on the timeliness of incorporating eES into the care continuum. Other threshold analyses should also be completed regarding the likelihood of true positive and true negative diagnoses. As ES accuracy and testing precision improves, the value of eES should also improve.
Although useful, PHIS has limitations. Since severe MitDs are rare and deadly, newborns in community hospitals may die prior to diagnosis. Since PHIS data are derived solely from children’s hospitals, similar patients from community hospitals are excluded, potentially underestimating MitD morbidity and mortality, which may bias the observed effect of implementing a novel diagnostic in the patient care continuum (Appendix Note 4).
Like other decision-analytic models, this analysis had additional limitations that may bias or impact these results. MitD is rare and often underdiagnosed. Data pertaining to longer-term outcomes and health-care resource allocation are scarce. CP was used as a proxy for generating costs and health state utilities to populate this model. Although similar, CP is a different illness than MitD, and both have different hurdles pertaining to cost and health states. Given the lower life expectancy of severe MitD patients relative to those of CP, results here may be an overestimate with the inclusion of costs seen in infants with CP, but not in infants with MitD.
Most available evidence regarding diagnostic likelihood and longer-term outcomes of patients with MitD is confined to single-institution studies at major academic hospitals. Patients seen at those centers likely have different outcomes and costs than those seen at smaller institutions, so the inclusion of such data may create bias. Finally, MitD is notoriously clinically and economically heterogeneous. Thus, the base case explored here may not represent the extreme clinical spectrum or diagnostic pathways for neonates with severe MitD.
This paper highlights that interventions leading to earlier diagnoses for MitD neonates are cost-effective and cost-minimizing. Through earlier diagnosis, parents can be counseled earlier, reducing family-associated emotional burden; earlier treatment can potentially stabilize the patient; or palliative care for severe cases can be implemented earlier. Although this paper demonstrates the clinical and economic value of eES as a diagnostic for newborns with severe metabolic disorders, the findings also highlight research areas important for improving neonatal care of patients with metabolic disorders. Further, EVPIs calculated here indicate that decision makers stand to gain upwards of $90,000 per MitD patient, if the uncertain parameters are studied further.
Scenario analyses demonstrate potential limitations of ES as a MitD diagnostic. Due to eES cost and diagnostic accuracy, eES is best served as an early diagnostic. Used as a last resort, early diagnosis benefit, such as earlier patient discharge and shorter NICU length-of-stay, are not observed in the modeled population, suggesting in some cases, no exome sequencing is as beneficial as late exome sequencing (Fig. 3). This finding underscores the importance of including eES as a first-line diagnostic, especially as diagnostic efficiency improves.
Threshold analyses demonstrate an interesting dynamic in this model. As total post-NICU cost increases, no sequencing incurs the largest iNMB. However, that decreases as total post-NICU cost decreases, and eES starts to incur the largest iNMB. Although this analysis is limited with fixed parameters, these findings demonstrate the importance of later life costs in determining the value of early-life diagnostics. This highlights the need for future discussions to address cost of patient treatment after stabilization as well as rethinking some neonatal care value metrics.
When evaluating eES from the societal perspective for a genetic disorder, there are other scenarios worth considering. For example, the newborn diagnostic odyssey can lead to a substantial caregiver and parent quality-of-life burden.33 Future analyses might also consider the advent of curative cellular therapies. Capturing the impact of curative therapies will also underscore the potential benefit of exploring innovative diagnostics.
As an expensive yet innovative diagnostic, convincing payers and public agencies to reimburse eES has been difficult. By modeling the clinical, health status, and cost associated with a severe neonatal MitD, we have demonstrated the value of earlier inclusion of ES in the diagnostic process. In addition to reducing the emotional toll on families awaiting diagnosis, these findings can be informative for clinicians and decision makers while we continue to search for a curative therapy for this devastating group of diseases.
Data availability
This model is available upon request by contacting the corresponding author.
Code availability
This model is available upon request by contacting the corresponding author.
References
Nelson, H. D., Bougatsos, C. & Nygren, P. Universal newborn hearing screening: systematic review to update the 2001 US Preventive Services Task Force Recommendation. Pediatrics. 122, e266–e276, https://doi.org/10.1542/peds.2007-1422 (2008).
Basel, D. & McCarrier, J. Ending a diagnostic odyssey: family education, counseling, and response to eventual diagnosis. Pediatr. Clin. 64, 265–272, https://doi.org/10.1016/j.pcl.2016.08.017 (2017).
Schaefer, A. M., Taylor, R. W., Turnbull, D. M. & Chinnery, P. F. The epidemiology of mitochondrial disorders—past, present and future. Biochim. Biophys. Acta. 1659, 115–120, https://doi.org/10.1016/j.bbabio.2004.09.005 (2004).
Honzik, T. et al. Neonatal onset of mitochondrial disorders in 129 patients: clinical and laboratory characteristics and a new approach to diagnosis. J. Inherit. Metab. Dis. 35, 749–759, https://doi.org/10.1007/s10545-011-9440-3 (2012).
Scaglia, F. Clinical spectrum, morbidity, and mortality in 113 pediatric patients with mitochondrial disease. Pediatrics. 114, 925–931, https://doi.org/10.1542/peds.2004-0718 (2004).
Gropman, A. L. Diagnosis and treatment of childhood mitochondrial diseases. Curr. Neurol. Neurosci. Rep. 1, 185–194, https://doi.org/10.1007/s11910-001-0015-9 (2001).
Rahman, S. & Poulton, J. Diagnosis of mitochondrial DNA depletion syndromes. Arch. Dis. Child. 94, 3–5, https://doi.org/10.1136/adc.2008.147983 (2009).
Dragojlovic, N. et al. The cost and diagnostic yield of exome sequencing for children with suspected genetic disorders: a benchmarking study. Genet. Med. 20, 1013–1021, https://doi.org/10.1038/gim.2017.226 (2018).
Schwarze, K., Buchanan, J., Taylor, J. C. & Wordsworth, S. Are whole-exome and whole-genome sequencing approaches cost-effective? A systematic review of the literature. Genet. Med. 20, 1122, https://doi.org/10.1038/gim.2017.247 (2018).
Smith, L. D., Willig, L. K. & Kingsmore, S. F. Whole-exome sequencing and whole-genome sequencing in critically ill neonates suspected to have single-gene disorders. Cold Spring Harb. Perspect. Med. 6, a023168, https://doi.org/10.1101/cshperspect.a023168 (2016).
Stark, Z. et al. Prospective comparison of the cost-effectiveness of clinical whole-exome sequencing with that of usual care overwhelmingly supports early use and reimbursement. Genet. Med. 19, 867–874, https://doi.org/10.1038/gim.2016.221 (2017).
Lionel, A. C. et al. Improved diagnostic yield compared with targeted gene sequencing panels suggests a role for whole-genome sequencing as a first-tier genetic test. Genet. Med. 20, 435–443, https://doi.org/10.1038/gim.2017.119 (2018).
Meng, L. et al. Use of exome sequencing for infants in intensive care units: ascertainment of severe single-gene disorders and effect on medical management. JAMA Pediatr. 171, e173438–e173438, https://doi.org/10.1001/jamapediatrics.2017.3438 (2017).
Dervan, A. P., Deverka, P. A., Trosman, J. R., Weldon, C. B., Douglas, M. P. & Phillips, K. A. Payer decision making for next-generation sequencing–based genetic tests: insights from cell-free DNA prenatal screening. Genet. Med. 19, 559–567, https://doi.org/10.1038/gim.2016.145 (2017).
Munnich, A. & Rustin, P. Clinical spectrum and diagnosis of mitochondrial disorders. Am. J. Med. Genet. 106, 4–17, https://doi.org/10.1002/ajmg.1391 (2001).
Debray, F.-G. et al. Long-term outcome and clinical spectrum of 73 pediatric patients with mitochondrial diseases. Pediatrics. 119, 722–733, https://doi.org/10.1542/peds.2006-1866 (2007).
Neumann, P. & Kamal-Bahl, S. Should value frameworks take a “societal perspective”? Health Affairs Blog. https://www.healthaffairs.org/do/10.1377/hblog20170906.061833/full/ (2021).
Paiva Coelho, M., Martins, E. & Vilarinho, L. Diagnosis, management, and follow-up of mitochondrial disorders in childhood: a personalized medicine in the new era of genome sequence. Eur. J. Pediatr. 178, 21–32, https://doi.org/10.1007/s00431-018-3292-x (2019).
PHIS. https://www.childrenshospitals.org/phis (2019).
Pew Research Center. How far Americans live from the closest hospital differs by community type. https://www.pewresearch.org/fact-tank/2018/12/12/how-far-americans-live-from-the-closest-hospital-differs-by-community-type/ (2018).
Ganz, M. L. The lifetime distribution of the incremental societal costs of autism. Arch. Pediatr. Adolesc. Med. 161, 343–349, https://doi.org/10.1001/archpedi.161.4.343 (2007).
McCormack, S. E. et al. Hospitalizations for mitochondrial disease across the lifespan in the US Mol. Genet. Metab. 121, 119–126, https://doi.org/10.1016/j.ymgme.2017.04.007 (2017).
Kruse, M., Michelsen, S. I., Flachs, E. M., Brønnum‐Hansen, H., Madsen, M. & Uldall, P. Lifetime costs of cerebral palsy. Dev. Med. Child. Neurol. 51, 622–628, https://doi.org/10.1111/j.1469-8749.2008.03190.x (2009).
Tonmukayakul, U. et al. Systematic review of the economic impact of cerebral palsy. Res. Dev. Disabil. 80, 93–101, https://doi.org/10.1016/j.ridd.2018.06.012 (2018).
Ramsey, S. et al. Good research practices for cost-effectiveness analysis alongside clinical trials: the ISPOR RCT-CEA Task Force Report. Value Health. 8, 521–533, https://doi.org/10.1111/j.1524-4733.2005.00045.x (2005).
Carroll, A. E. & Downs, S. M. Improving decision analyses: parent preferences (utility values) for pediatric health outcomes. J. Pediatr. 155, 21–25.e5, https://doi.org/10.1016/j.jpeds.2009.01.040 (2009).
Gold, M., Siegel, J., Russell, L. & Weinstein, M. Cost-Effectiveness in Health and Medicine. (Oxford University Press, Oxford, 1996).
Neumann, P., Sanders, G., Russell, L., Siegel, J. & Ganiats, T. Cost-Effectiveness in Health and Medicine. 2nd edn. (Oxford University Press, Oxford, 2017).
Neumann, P. J. et al. Future directions for cost-effectiveness analyses in health and medicine. Med. Decis. Making 38, 767–777, https://doi.org/10.1177/0272989X18798833 (2018).
Green, R. C. et al. ACMG recommendations for reporting of incidental findings in clinical exome and genome sequencing. Genet. Med. 15, 565–574, https://doi.org/10.1038/gim.2013.73 (2013).
York Health Economics Consortium. Expected value of perfect information (EVPI). https://yhec.co.uk/glossary/expected-value-of-perfect-information-evpi/ (2016).
AHIP. The rise of orphan drugs. https://www.ahip.org/the-rise-of-orphan-drugs/ (2019).
Carmichael, N., Tsipis, J., Windmueller, G., Mandel, L. & Estrella, E. “Is it going to hurt?”: the impact of the diagnostic odyssey on children and their families. J. Genet. Couns. 24, 325–335, https://doi.org/10.1007/s10897-014-9773-9 (2015).
NW 1615 L. St, Suite 800Washington, Inquiries D 20036USA202-419-4300 | M-857-8562 | F-419-4372 | M. How far Americans live from the closest hospital differs by community type. Pew Research Center. Published March 2, 2020. Accessed March 2, 2020. https://www.pewresearch.org/fact-tank/2018/12/12/how-far-americans-live-from-the-closest-hospital-differs-by-community-type/
Honeycutt, A. A. et al. Economic costs of mental retardation, cerebral palsy, hearing loss, and vision impairment. Using Survey Data to Study Disability: Results from the National Health Survey on Disability (Research in Social Science and Disability) 3, https://doi.org/10.1016/S1479-3547(03)03011-2 (2003).
Petrou, S. & Kupek, E. Estimating preference-based health utilities index mark 3 utility scores for childhood conditions in England and Scotland. Med. Decis. Making. 29, 291–303, https://doi.org/10.1177/0272989X08327398 (2009).
Hong, S. et al. Clinical utility in infants with suspected monogenic conditions through next-generation sequencing. Mol. Genet. Genomic Med. 7, e684, https://doi.org/10.1002/mgg3.684 (2019).
Bodian, D. L. et al. Utility of whole-genome sequencing for detection of newborn screening disorders in a population cohort of 1,696 neonates. Genet. Med. 18, 221–230, https://doi.org/10.1038/gim.2015.111 (2016).
Soden, S. E. et al. Effectiveness of exome and genome sequencing guided by acuity of illness for diagnosis of neurodevelopmental disorders. Sci. Transl. Med. 6, 265ra168–265ra168, https://doi.org/10.1126/scitranslmed.3010076 (2014).
Goel, H., Lusher, A. & Boneh, A. Pediatric mortality due to inborn errors of metabolism in Victoria, Australia: a population-based study. JAMA. 304, 1070–1072, https://doi.org/10.1001/jama.2010.1259 (2010).
Author information
Authors and Affiliations
Contributions
Conceptualization: S.A.C., C.L.G., L.Y., and L.M.R. Data curation: S.A.C. and C.L.G. Formal analysis: S.A.C. Investigation: S.A.C., C.L.G., L.Y., L.M.R., J.W.H. Methodology: S.A.C., C.L.G., and J.W.H. Project administration: S.A.C. and C.L.G. Supervision: C.L.G., L.Y., L.M.R., and J.W.H. Visualization: S.A.C. Writing—original draft: S.A.C. and C.L.G. Writing—review & editing: S.A.C., C.L.G., L.Y., L.M.R., and J.W.H.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Crawford, S.A., Gong, C.L., Yieh, L. et al. Diagnosing newborns with suspected mitochondrial disorders: an economic evaluation comparing early exome sequencing to current typical care. Genet Med 23, 1854–1863 (2021). https://doi.org/10.1038/s41436-021-01210-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-021-01210-0