Abstract
Purpose
Cancer genetics clinics have seen increasing demand, challenging genetic counselors (GCs) to increase efficiency and prompting some clinics to implement genetic counseling assistants (GCAs). To evaluate the impact of GCAs on Geisinger’s cancer genetics clinic, we tracked GC time utilization, new patient volume, and clinic cost per patient before and after implementing a GCA program.
Methods
GCs used time-tracking software while completing preappointment activities. Electronic health records were reviewed for appointment length and number of patients per week. Internal salary data for GCs and GCAs were used to calculate clinic costs per patient.
Results
Time spent by GCs completing each preappointment activity (21.8 vs. 15.1 minutes) and appointment length (51.6 vs. 44.5 minutes) significantly decreased after GCA program implementation (p values < 0.001). New patients per week per GC significantly increased (7.9 vs. 11.4, p < 0.001). Weekly clinic cost per patient significantly decreased ($233 vs. $176, p = 0.03).
Conclusion
Implementing a GCA program increased GC efficiency in preappointment activities and clinic appointments, increased patient volume, and decreased clinic cost per patient. Such a program can improve access to GC services and assist GCs in focusing on the direct patient care for which they are specially trained.
Similar content being viewed by others
INTRODUCTION
Genetic counselors who practice in cancer genetics have been under increasing pressure to improve the efficiency of their clinic operations as referrals have steadily increased. Multiple reasons for this increase have been noted, including the “Angelina Jolie effect” (i.e., increased visibility of hereditary cancer risk after the actress's public disclosure of her BRCA1 carrier status and subsequent management choices);1,2 the expanding scope of National Comprehensive Cancer Network (NCCN) guidelines for cancer genetic counseling and consideration of genetic testing (e.g., the recent addition of metastatic prostate cancer diagnoses as a criterion for considering testing);3 availability of treatment regimens targeted to germline status (e.g., PARP inhibitors in the context of BRCA1/2 variants and PDL1 checkpoint inhibitors in the context of mismatch repair deficient tumors);4,5,6 and an expanding number of laboratories offering genetic testing, thus decreasing cost and increasing access.7,8
With this increasing demand for cancer genetics services, Hoskovec et al. expressed concern that there may be a genetic counselor (GC) workforce shortage and access issues in some areas of the country, and projected that the number of GCs in direct patient care will not satisfy the demand for GC services until as late as 2030.9 Given that the majority of GC time is spent completing patient-related activities outside of direct care, there is a significant opportunity to improve efficiencies of these tasks and potentially increase patient access.10 While it remains important to increase the genetic counseling workforce, it is essential to explore alternative service delivery models to increase efficiency and support GCs in providing direct patient care at the top of their scope of practice.
To address the increasing demand for cancer genetics services, some clinics have used genetic counseling assistants (GCAs) or similarly specialized clinical support staff.11,12 GCAs have been reported to take part in clinical support activities such as assisting with administrative tasks and contacting patients to collect information or disclose negative results.11,13 Unlike other administrative support staff, GCAs are specifically trained to take on roles that were previously completed by genetic counselors. These positions aim to increase the amount of time GCs spend on direct patient care, with the intent of improving patient access to GC services.
In one cancer genetics clinic’s analysis of GCA utilization, average weekly patient volume increased by 58.5% post-GCA utilization with a ratio of one GCA to three GCs.11 Internal and external GCs surveyed for the study reported that utilization of GCAs resulted in perceived increased efficiency.11 Although GCAs may assist GCs in spending less time on administrative tasks and more time in direct patient care,10 little research has evaluated how GCAs specifically impact time GCs spend on various clinic-related tasks.
Geisinger’s cancer genetics clinic saw a steady increase in referrals of just over 20% per year from 2014 to 2018. To address this increasing demand, GCAs were incorporated into the clinic in early 2016. We sought to evaluate the impact of the GCA program by measuring the following variables pre- and post-GCA implementation: (1) time spent by GCs in preappointment activities, (2) length of GC appointments, (3) patients per week per GC full-time equivalent (FTE), and (4) estimated clinic cost per patient per week. Since GCAs completed some preappointment activities previously performed by GCs at a lower salary than GCs, we hypothesized that implementing the GCA program would be associated with increased GC efficiency preappointment, decreased appointment length, increased patient volume per GC, and decreased weekly clinic cost per patient.
MATERIALS AND METHODS
Setting: Geisinger’s Cancer Genetics Risk Assessment Clinic
Geisinger is an integrated rural health-care system serving the central, south central, and northeastern regions of Pennsylvania and southern New Jersey. GCs within the cancer genetics clinic divide their time between clinic and research projects. Funding support for the GC’s clinic time is provided by the hematology/oncology department, with a total of 1.5 FTEs of GC clinic time throughout the study. The effort of each GC ranged from 0.2 to 0.6 FTEs. For example, at the time of the study, one GC had 0.2 FTE, meaning one day per week of dedicated cancer clinic time, and another GC had 0.4 FTE, meaning two days a week of dedicated clinic time. All GCs are certified by the American Board of Genetic Counseling, have Pennsylvania state GC licensure, and are credentialed by Geisinger. At the time of the study, GCs at Geisinger were not billing for their services.
The Genetic Counseling Intervention Reporting Standards are used here as a framework to describe Geisinger’s cancer genetics clinic operations.14 The indication for referral to the clinic is typically a personal and/or family history of cancer suggestive of a hereditary predisposition. Referrals can be made by internal or external providers, or individuals can self-refer. Services are provided across the Geisinger system, at hospital- and clinic-based locations. In-person GC consultations are typically completed prior to genetic testing and take 30 to 70 minutes. Risk assessment includes a three-generation family history, detailed personal history, review of pathology and tumor studies, and use of risk models such as MMRpro or BRCAPRO as appropriate.15,16 NCCN guidelines inform decisions on whether and what genetic testing will be offered. Genetic counseling follows published recommendations for cancer genetic counseling and includes information about the risk assessment, discussion of genetic testing options, and psychosocial support.17,18 Results are most often disclosed over the phone, with the option to return for an in-person appointment for individuals who are identified to carry a pathogenic/likely pathogenic variant. After results disclosure, GCs assist in coordinating referrals to clinics for surveillance as indicated (e.g., high-risk breast clinic for someone with negative genetic testing and a family history of breast cancer).
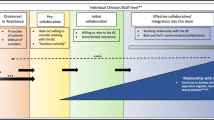
Importantly, the overall genetic counseling process described above did not change with the addition of GCAs. Rather, specific activities were shifted from GCs to GCAs. This shift also changed the timing of family history taking from in-session with a GC to presession with a GCA. Figure 1a shows the overall workflow of the GCs in the pre-GCA time period.
(a) Pre–genetic counseling assistant (GCA) workflow. (b) Post-GCA workflow. GC time in preappointment activities directly tracked by GCs, GC time in direct care as documented in the electronic health record (EHR). Preappointment tasks started by or completed by a GCA in post-GCA workflow are highlighted. Postappointment time not reported as there were no changes to this workflow. *Three-generation pedigree moved from direct care with GC to preappointment with GCA. GINA Genetic Information Nondiscrimination Act of 2008.
Setting: Geisinger GCA program
As with the GCs, Geisinger GCAs divide their time between clinic and research projects and GCA clinic time is funded by the hematology/oncology department. GCAs at Geisinger are required to have a bachelor’s degree and strong interpersonal and organizational skills. An interest in graduate training in genetic counseling or related health career is preferred. GCA training is completed using written standard operating procedures, authored initially by Geisinger GCs and regularly updated by GCAs, as well as by observing GCs and GCAs completing specific tasks (e.g., taking a family history or completing chart review). Typically, GCAs independently perform preappointment tasks after three weeks of onboarding and training. Training of GCAs is completed by GCs and GCAs directly involved in the clinic, and this time is supported by clinic funding.
During the study time period, GCAs supported the clinic by assisting GCs in completing tasks related to upcoming appointments. Figure 1b summarizes GC and GCA tasks related to clinic workflow in the post-GCA time period. Preappointment activities completed by GCAs included general case preparation, such as records review, insurance authorization, test kit preparation, and documentation of a three-generation pedigree, and cancer screening history. GCAs were additionally tasked with supporting overall clinic functioning by GCAs reviewing incoming referrals to determine whether individuals needed to be seen on an urgent basis, such as for treatment or surgical management decisions, scheduling appointments, and making confirmation calls for upcoming appointments. Additionally, questions from providers (such as whether a referral is indicated) or patients (such as cost of testing or location of appointment) were answered by GCAs via a general phone line and secure electronic messages through the patient portal within the electronic health record (EHR) or secure emails using the institutional email system.
GCAs did not complete any tasks during GC appointments or at the time of result disclosure, nor did they assist GCs in any postappointment tasks such as summary letters or referral coordination.
Data collection: GC time tracking
Time tracking was completed before and after implementation of the GCA program. The first time period serves as the baseline, during which there was no GCA clinic support. The second tracking period represents fully implemented GCA preappointment support.
GCs developed a detailed fishbone diagram (Fig. 1a) of all clinic-related tasks and grouped these tasks, by consensus, into the broad categories of preappointment, direct care, postappointment, or ancillary activities. In developing the GCA program, GCs identified tasks they deemed appropriate for GCAs to complete or initiate, most of which were related to preparing for upcoming appointments. One activity, taking a three-generation pedigree, shifted from in-session with the GC to preappointment with the GCA. We report on the GC time tracked for preappointment activities and the length of the GC session as these are the areas where tasks were supported by the GCAs. We do not report on postappointment activities since this workflow did not change with the implementation of GCA clinic support.
GCs used Toggl (www.toggl.com),19 a web-based time-tracking application, to manually track time by clicking a start button when beginning a specific preappointment activity and a stop button at completion of the activity. GCs who were involved in time tracking in the pre-GCA period trained the GCs who were new to the clinic on the Toggl application for consistency in time tracking between GCs and across time periods.
This activity-centric method of time tracking allows for review of total time GCs spent preparing for clinics and the amount of time spent on each preappointment activity. To illustrate with an example from the post-GCA time period: if a 47-year-old woman was referred for a personal history of breast cancer diagnosed at age 43, she would be first triaged by the GCA to the next available appointment. The GC would quickly review that triage decision and would agree with the outcome of scheduling for the next available appointment. Closer to the time of the appointment, the GCA would complete a more detailed chart review, gathering information about the relevant pathology, treatment, and any family history noted in the chart. The GCA would also contact the patient and gather a detailed three-generation pedigree, with targeted questions related to the history of breast cancer (e.g., any ovarian cancer in the family history? Ashkenazi Jewish ancestry?). Finally, the GCA would start the genetic testing requisition form, inputting information such as the patient’s name, age, date of birth, and insurance details. The GC would review the pedigree and pathology reports gathered by the GCA and complete the testing requisition form as part of their clinic preparation, tracking the preappointment tasks individually. The time taken by the GC to complete each preappointment activity of (1) reviewing the referral, (2) reviewing the history and pedigree, and (3) completing the genetic test requisition form was tracked in the Toggl application as a unique preappointment task. Of note, these activities are not connected back to this individual patient, and tasks related to a single patient may be separated from each other by several weeks. The measure of each preappointment activity captures the completion of individual activities, whereas the total time in preappointment activities captures the time spent per week completing all preappointment activities.
Data collection: appointment length, patient volume, and clinic cost
Appointment duration was determined by EHR chart review for visit length as documented by the GC in the chart note at the time of the visit. EHR data were used to capture the number of new patient appointments. Clinic costs were estimated based on internal GC and GCA salary information at the post-GCA time period.
Statistical analysis
For each GC, time tracked in preappointment activities was aggregated by week. Weekly minutes were standardized between GCs by dividing the weekly time tracked by the GC’s dedicated clinic FTE, providing a consistent basis for making inferences across the pre-GCA and post-GCA time periods. The time spent by GCs in completing each preappointment activity was positively skewed. Thus, we applied a log transformation, which yielded an approximately normal distribution of minutes per activity. Weekly clinic volume was calculated for each GC by dividing the number of appointments they completed by their dedicated clinic FTE, thereby standardizing volume between GCs to allow for comparisons. Consequently, formal analyses of clinic volume are based on the number of patients each GC would have seen if they had 1.0 FTE in clinic, not on the actual number of patients seen in the clinic. To analyze the effect of GCA implementation on GC time and patient volume, we used multilevel regression models comparing the pre-GCA and post-GCA periods (i.e., time period was a fixed-effect predictor). We included a random intercept for GC to account for individual differences among counselors in time and patient volume. Relative to conventional regression methods within a general linear modeling framework, which assume that the observations are independent, multilevel models allowed for statistical dependency due to repeated assessments of each counselor.20 The multilevel models reported here assume that the relationship between predictors and the outcome is linear, that the variance of the residuals is homogeneous between timepoints, that residuals are normally distributed, and that random effects follow a normal distribution. We verified that these assumptions held in our data by visual inspection, as well as through application of a variant of Levene’s test for equal residual variance.21 As noted above, time spent by GCs in preappointment activities was positively skewed, yielding a non-normal distribution of residuals. However, log transformation of this variable normalized the distribution and satisfied all modeling assumptions.
We note that the small number of GCs in the analysis is relatively low for multilevel approaches.22 Thus, we also recomputed all of our statistics using a linear model that treated each GC uniquely as a fixed-effect predictor. This avoids the parametric assumption on the distribution of counselor-specific means, while nevertheless accounting for dependency in the data due to GC effects.
To estimate clinic cost per patient, weekly new patient clinic volume was divided by the average clinic salary rate. For the pre-GCA period, new patient volume was divided by average GC salary rate, whereas in the post-GCA period, we normalized by the average GC and GCA salary rate. To minimize effects of expected changes in salaries over time, the average GC salary rate at the post-GCA time period was used for all GC cost estimates. During both periods, there was a week that had very low volume due to GC absence from clinic for vacation or conference travel. These weeks were dropped from the cost analysis. The Wilcoxon rank sum test was used to compare the average weekly clinic cost per patient between the pre-GCA and post-GCA time periods. To test the impact of dropping low volume weeks from the analysis, a sensitivity analysis was performed. GC average volume was used to impute weekly patient volume for individual GCs absent due to vacation or conference attendance. The Wilcoxon rank sum test was again used to compare weekly clinic cost per patient.
All analyses were performed using R (version 3.5.1);23 multilevel models were run using the lme4 package with restricted maximum likelihood estimation.24 All code used for analyses is available from the corresponding author upon request.
RESULTS
GCA program implementation
Time tracking took place during two periods: in November–December 2015 (9 weeks; pre-GCA) and April–May 2017 (9 weeks; post-GCA). GC staffing remained consistent at 1.5 FTE through both time-tracking periods, although individual GCs differed between time periods. There were four GCs in each time period, two of whom were in both periods. In the post-GCA time period there was 1.3 FTE of GCA effort split between three GCAs. All GCAs had been onboarded and trained in cancer clinic-related tasks at least 5 months prior to the start of the post-GCA period. During the pre-GCA period, the clinic saw 75 new patients in 9 weeks; in the post-GCA period, 129 new patients were seen in 9 weeks.
Time utilization, patient volume, and clinic costs
As summarized in Table 1, the mean total time spent by GCs per week per FTE in preappointment activities was not significantly different between timepoints (380.8 vs. 456.7 minutes, p = 0.48). The mean time spent by GCs each time they completed a preappointment activity, however, was significantly lower in the post-GCA compared with the pre-GCA time period (21.8 vs. 15.2 minutes, p < 0.001; see Fig. 2). There was a significant decrease in average appointment length between pre- and post-GCA time periods (51.6 vs. 44.5 minutes, p < 0.001). Average total patients seen per week per GC FTE significantly increased from 7.9 patients pre-GCA to 11.4 patients post-GCA (p < 0.001). None of our results changed qualitatively in the alternative linear model approach, suggesting that our findings are robust to different modeling assumptions (additional details available from the corresponding author upon request). Estimated weekly clinic cost per patient significantly decreased between the time periods ($233 vs. $176, p = 0.03). The alternative analysis of the imputed clinic volume did not change these results.
DISCUSSION
Our results show that GCs spent significantly less time completing each preappointment activity and average appointment length was significantly shorter at the post-GCA timepoint with a concomitant decrease in weekly clinic cost per patient. This is the first study to demonstrate the impact of GCAs on GC time utilization and clinic cost in a cancer genetics clinic and supports prior studies demonstrating that incorporation of GCAs can lead to increased patient volume per GC FTE.11,13 By shifting specific preappointment tasks to GCAs, GCs increased their efficiency in preparing for upcoming appointments and decreased appointment length in clinic. The time saved in clinic by shorter appointments allowed for additional patients to be scheduled per clinic day, and GCs were able to prepare for a greater number of upcoming appointments without any additional dedicated clinic time because they were more efficiently completing the preappointment activities. The time-tracking data add quantitative evidence to previous qualitative reports that GCA employment resulted in perceived streamlined clinic processes and identify which specific tasks are responsible for the improved efficiency.11
There was a significant decrease in the estimated clinic cost per patient per week after implementation of the GCA program. Since this was evaluated by holding the GC cost stable, it suggests that the decrease in clinic cost per patient was related to the addition of the GCA clinic support. Given the challenges for billing and reimbursement of genetic counseling services, improving the cost structure borne by the service line is paramount. In clinics where GCs bill for services, the increased patient volume has potential to increase revenue and offset the increased personnel costs of adding GCA support staff.
This study is a pre–post evaluation of a program implemented in a real-world clinical practice. While this design is a major strength for its generalizability, there is also the possibility of organizational and personnel changes influencing the study results that cannot be accounted for in the analysis. Over the 18 months it took to implement a fully functional GCA program, Geisinger Health Plan changed their criteria to no longer require prior authorization for genetic testing for breast cancer risk when individuals met NCCN guidelines for BRCA1/2 testing (preauthorization requirements did not change for other cancer predisposition syndromes such as Lynch syndrome). As nearly one-third of patients were covered by this insurance plan, there was likely an overall administrative time savings associated with no longer needing to secure testing coverage for these patients. Importantly, the prior authorization process for this payer was a straightforward form letter; the time savings of not completing this letter was deemed modest and unlikely to significantly impact our results. One of the four GCs (0.4 FTE) was a recent graduate during the pre-GCA assessment period, but by the post-GCA assessment period she was experienced, which would be expected to improve efficiency, potentially impacting the attribution to GCA implementation, although this could not be quantified. Finally, the study relies on each GC tracking their time consistently and documenting appointment length accurately in the EHR. It is possible that there were errors made in the precision of the time tracking. While recognizing the potential confounding variables, we do not think these other factors could entirely account for the magnitude of the measured changes.
Regarding the cost analysis, clinic cost per patient was estimated using the weekly aggregated number of new patients and is not a direct reflection of how much time was spent on each patient. Additionally, we did not include ancillary costs (e.g., space, phones, computers) required to support the additional GCA staff members. However, we expect that these items would have a minimal impact on the final estimated cost per patient when spread over the number of patients in the study.
Our study focused on the time spent by GCs preappointment and in clinic since the GCAs supported preappointment activities. However, this does not capture all time spent by GCs on clinic-related tasks or all tasks in which GCAs could be used to offset GC effort. Future studies could investigate the impact of GCA support in postappointment activities, such as calling out negative results. Furthermore, evaluation of GCA programs in other GC practice settings, such as pediatrics, prenatal, laboratory, and research, would add important perspectives on the value of GCA programs in different clinical contexts. Alternative measures of patient access, including time to appointment, should also be considered, along with measures of quality of care and cost-effectiveness. Finally, it is vital to consider research related to the experience that patients, GCs, and GCAs have with clinic operations that incorporate GCAs.
As the demand on the GC workforce continues to grow, it is paramount to identify opportunities to improve patient access to GC services while preserving the essential value of the GC encounter. Our data on GC time utilization, clinic volume, and clinic cost suggest that GCAs could be a valuable addition to cancer genetics clinics, increasing the volume of patients for whom GCs are able to provide services at a significantly lower cost per patient without increasing GC FTE.
References
Evans DG, Barwell J, Eccles DM, et al. The Angelina Jolie effect: how high celebrity profile can have a major impact on provision of cancer related services. Breast Cancer Res. 2014;16:442.
Freedman R, Mountain H, Karina D, Schofield L. A retrospective exploration of the impact of the ‘Angelina Jolie Effect’ on the single state-wide familial cancer program in Perth, Western Australia. J Genet Couns. 2017;26:521–562.
National Comprehensive Cancer Network. Clinical practice guidelines in oncology. Genetic/familial high risk assessment: breast and ovarian. Version 3.2019. January 18, 2019. NCCN.org. https://www.nccn.org/professionals/physician_gls/pdf/genetics_bop.pdf.
Markman M. Poly (ADP-ribose) polymerase inhibitors in the management of ovarian cancer. Women’s Health (Lond). 2018;14:1745505717750694.
Keung MYT, Wu Y, Vadgama JV. PARP inhibitors as a therapeutic agent for homologous recombination deficiency in breast cancers. J. Clin Med. 2019;8:435.
Le DG, Uram JN, Wang H, et al. PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med. 2015;372:2509–2520.
Kesselheim AS, Cook-Deegan RM, Winickoff DE, Mello MM. Gene patenting—the Supreme Court finally speaks. N Engl J Med. 2013;369:869–875.
Genetic Testing Registry. https://www.ncbi.nlm.nih.gov/gtr/. Accessed May 2019.
Hoskovec JM, Bennett RL, Carey ME, et al. Projecting the supply and demand for certified genetic counselors: a workforce study. J Genet Couns. 2018;27:16–120.
Attard CA, Carmany EP, Trepanier AM. Genetic counselor workflow study: the times are they a-changin’? J Genet Couns. 2019;28:130–40.
Pirzadeh-Miller S, Robinson LS, Read P, Ross TS. Genetic counseling assistants: an integral piece of the evolving genetic counseling service delivery model. J Genet Couns. 2016;26:716–727.
Cohen SA, Nixon DM. A collaborative approach to cancer risk assessment services using genetic counselor extenders in a multi-system community hospital. Breast Cancer Res Treat. 2016;159:527–534.
Heydrich C, Stickevers S. The genetic counseling assistant: Dana-Farber’s experience in establishing a new role. Presented at: 35th Annual Education Conference of the National Society of Genetic Counselors; September 28–October 1, 2016; Seattle, WA.
Hooker GW, Babu D, Myers MF, Zierhut H, McAllister M. Standards for the reporting of Genetic Counseling Interventions in Research and Other Studies (GCIRS): an NSGC Task Force report. J Genet Couns. 2017;26:355–360.
Berry DA, Iversen ES, Gudbjartsson DF, et al. BRCAPRO validation, sensitivity of genetic testing of BRCA1/BRCA2, and prevalence of other breast cancer susceptibility genes. J Clin Oncol. 2002;20:2701–2712.
Chen S, Wang W, Lee S, et al. Prediction of germline mutations and cancer risk in the Lynch syndrome. JAMA. 2006;296:1479–1487.
Riley BD, Culver JO, Skrzynia C, et al. Essential elements of genetic cancer risk assessment, counseling, and testing: updated recommendations of the National Society of Genetic Counselors. J Genet Couns. 2012;21:151–161.
Robson ME, Bradbury AR, Arun B, et al. American Society of Clinical Oncology policy statement update: genetic and genomic testing for cancer susceptibility. J Clin Oncol. 2015;33:3660–3667.
Toggl time tracking software. Toggle.com. Wilmington, DE, USA: Toggl Inc; Accessed November–December 2015 and March–April 2017.
Hox JJ, Moerbeek M, van de Schoot R. Multilevel analysis: techniques and applications. 2nd ed. New York: Routledge; 2010.
Fox J. Applied regression analysis and generalized linear models. 2nd ed. Thousand Oaks, CA: Sage Publications; 2008.
Maas CJM, Hox JJ. Sufficient sample sizes for multilevel modeling. Methodology. 2005;1:86–92.
R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2018. https://www.R-project.org/.
Bates D, Maechler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67:1–48.
Acknowledgements
Special thanks to our genetic counseling colleague, Audrey Fan, for her efforts to begin and evaluate the GCA program at Geisinger. The authors also acknowledge the funding support of Geisinger Research and Hematology/Oncology departments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
M.R. is a stockholder of Helix, LLC. The other authors declare no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hallquist, M.L.G., Tricou, E.P., Hallquist, M.N. et al. Positive impact of genetic counseling assistants on genetic counseling efficiency, patient volume, and cost in a cancer genetics clinic. Genet Med 22, 1348–1354 (2020). https://doi.org/10.1038/s41436-020-0797-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-020-0797-2
Keywords
This article is cited by
-
A qualitative exploration of interprofessional collaborative practice between genetic counselors and mental health providers
Journal of Community Genetics (2023)
-
An overview of genetic services delivery for hereditary breast cancer
Breast Cancer Research and Treatment (2022)