Abstract
Purpose
Guidelines by professional organizations for assessing variant pathogenicity include the recommendation to utilize biologically relevant transcripts; however, there is variability in transcript selection by laboratories.
Methods
We describe three patients whose genomic results were incorrect, because alternative transcripts and tissue expression patterns were not considered by the commercial laboratories.
Results
In individual 1, a pathogenic coding variant in a brain-expressed isoform of CKDL5 was missed twice on sequencing, because the variant was intronic in the transcripts considered in analysis. In individual 2, a microdeletion affecting KMT2C was not reported on microarray, since deletions of proximal exons in this gene are seen in healthy individuals; however, this individual had a more distal deletion involving the brain-expressed KMT2C isoform, giving her a diagnosis of Kleefstra syndrome. Individual 3 was reported to have a pathogenic variant in exon 10 of OFD1 on exome, but had no typical features of the OFD1-related disorders. Since exon 10 is spliced from the more biologically relevant transcripts of OFD1, it was determined that he did not have an OFD1 disorder.
Conclusion
These examples illustrate the importance of considering alternative transcripts as a potential confounder when genetic results are negative or discordant with the phenotype.
Similar content being viewed by others
INTRODUCTION
Genomic sequencing (exome/genome/targeted gene sequencing) and allied techniques such as chromosomal microarray (CMA) are widely used for the diagnosis of genetic diseases and while these have revolutionized genomic medicine, determining variant pathogenicity remains a challenge in diagnostic decision-making. The American College of Medical Genetics and Genomics/Association for Molecular Pathology (ACMG/AMP) standards and guidelines for the interpretation of sequence variants have stated that in addition to the reference transcript (i.e., canonical), alternate clinically relevant transcripts (e.g with additional exons, or expressed in a tissue of interest) should be evaluated in assessing variant pathogenicity.1 For analysis of copy-number variants (CNVs) on CMA alternate transcripts are less likely to be a confounding factor, but the interpretation of CNVs can be influenced by tissue-specific transcript expression, a fact that is seldom discussed in the existing literature.
The importance of alternate transcripts in interpreting genetic testing is underscored by the finding that ~95% of multiexon genes undergo alternative splicing, with an average of seven transcripts per gene; furthermore, these can be differentially expressed across tissues and developmental timespans.2,3 Interpretation of genomic variation may thus differ according to transcript selection and tissue expression.4 Several transcript databases are available for variant annotation, including GENCODE (https://www.gencodegenes.org/), RefSeq (https://www.ncbi.nlm.nih.gov/refseq/), Ensembl (https://www.ensembl.org), and Consensus Coding Sequencing (CCDS; https://www.ncbi.nlm.nih.gov/projects/CCDS). Each laboratory selects its own reference transcript and as a result, there is great variability in the transcripts utilized by sequencing laboratories.5
Highlighting the impact of this variability in transcript selection, an annotation comparison of 80 million genome sequencing (GS) variants using two different transcript sets (RefSeq and Ensembl) produced agreement in annotation in only 44% of putative loss-of-function (LoF) variants.6 Another study demonstrated that for 292 genes included on three neonatal epilepsy panels, only one transcript was considered by the commercial laboratories for 96% of the genes, although 30% of these genes had alternative coding regions expressed in fetal/neonatal brain tissue.5 Four missed pathogenic variants were found when variants were reannotated as LoF in alternate transcripts.5 The opposite could also occur, with a putative pathogenic variant being reannotated as not disease-associated, in the context of alternative isoforms. Thus, errors in considering alternative transcripts can result in both missed and incorrect diagnoses.
Here we present three individuals, in whom genomic results were either negative or discordant with the clinical phenotype, and subsequent evaluation of alternate transcripts and their expression in the tissues of interest provided diagnostic clarity.
MATERIALS AND METHODS
All evaluations were performed as part of the National Institutes of Health (NIH) Undiagnosed Diseases Network (UDN) (https://undiagnosed.hms.harvard.edu/) under an institutional review board (IRB)-approved protocol (National Human Genome Research Institute [NHGRI] 15-HG-0130), and informed consent was obtained from all subjects. Further consent for photographs to be used in a publication was provided for individual 2 (Supplementary Material). Trio exome sequencing (ES) had previously been performed at a commercial lab for all three individuals, and FASTQ files were requested and reanalyzed in the UDN as described previously.7 Trio GS was performed for individuals 1 and 2 through the UDN.8 Review of the literature, transcript databases, and CMA data was conducted for variant reannotation. Clinically relevant results were confirmed by an orthogonal method before communication to the individuals/parents.
RESULTS
Individual 1 is a 3-year, 4-month-old Caucasian male, with refractory infantile spasms, atonic seizures, developmental regression with onset of seizures, and current skills of a 9–12 month old (details in Supplementary Material). The family history was unremarkable. Pre-UDN testing included a normal CMA, normal comprehensive epilepsy panel (which included CDKL5), and nondiagnostic trio ES. The latter two tests had been performed through the same commercial laboratory.
Reanalysis of the ES data in the UDN was nondiagnostic, but GS revealed a novel de novo hemizygous CDKL5 c.2842C>T; p.(Arg948*) variant (NM_001323289.1) in exon 17, interpreted as pathogenic by the UDN laboratory. The alternative NM_001323289.1 isoform chosen by this laboratory for analysis is more biologically relevant than the canonical transcript, because it is the most abundant isoform expressed within the central nervous system.9 The patient’s clinical phenotype was consistent with CDKL5-associated epileptic encephalopathy (MIM 300672). Since LoF is the disease mechanism for this disorder we evaluated why this variant had not been reported previously on the epilepsy panel, ES, or the UDN reanalysis of exome data.
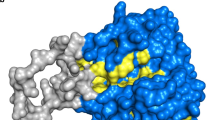
CDKL5 has multiple isoforms due to alternative splicing, three of which are included in the National Center for Biotechnology Information (NCBI) RefSeq Database (Fig. 1a). The commercial laboratory had used the canonical (longest) transcript NM_003159 for ES analysis in October 2016 (and for the prior epilepsy panel in 2015), and this variant had not been reported because it appeared in an intronic region just past exon 18. However, in the alternative RefSeq transcript NM_001323289.1 that was considered by the UDN genomic sequencing laboratory, this variant is within a coding region designated as exon 17. This exon extends further in the 3’ direction in this transcript, into what is an intronic region in the canonical transcript. The variant identified in individual 1 is located in this “extra” region of exon 17, indicated by the red arrow in Fig. 1a. In ClinVar there are two other individuals with different pathogenic variants within this “extra” region of exon 17 (these variants have been previously reported10,11), and there are no LoF variants within this region in gnomAD (https://gnomad.broadinstitute.org). Interestingly, the research-based pipeline used for UDN exome reanalysis also did not report the variant as the corresponding Ensembl transcript had not yet been added to the annotation build used.
Black boxes represent predicted coding sequence, smaller black boxes represent untranslated regions (UTRs), and black lines represent intronic sequences with arrowheads indicating the direction of transcription. Exons are labeled. a The three CDKL5 RefSeq transcripts NM_003159.2 (canonical), NM_001037343, and NM_001323289.1 are shown. The variant identified in individual 1 is designated with a red arrow. Pathogenic variants in this “extra” region of exon 17 previously reported by Bodian et al.11 and Archer et al.10 are designated with black arrows. The thick gray arrow indicates the region beyond codon 938 (NM_003159.2 only) for which Diebold et al.12 urges caution against overassigning pathogenicity. b The KMT2C RefSeq transcript NM_170606.3 (Ensembl transcript ENST00000262189) and seven additional protein coding Ensembl transcripts are shown. Deletions (red bars) and duplications (blue bars) in the Database of Genomic Variants (DGV) are shown at the top of the figure. At the bottom, the p.(Lys564*) pathogenic variant reported by Koemans et al.13 is represented by a red arrow. The 127-kb deletion identified in individual 2 and the 203-kb deletion previously reported by Koemans et al.13 are represented by horizontal red bars. c The three OFD1 RefSeq transcripts NM_001330209.1, NM_001330210.1, and NM_003611.2 (canonical) are shown. The variant identified in individual 3 is designated with a red arrow. The other three predicted loss-of-function (LoF) variants seen in gnomAD are labeled with black arrows, along with frequency and gender in which they were identified.
The alternative transcript NM_001323289.1 was added to the NCBI RefSeq database in April 2016, but had not yet been added to the commercial laboratory’s annotation pipeline at the time of this individual’s epilepsy panel and ES analyses (personal communication with commercial laboratory). The commercial laboratory listed two other reasons for this variant not being reported: (1) the presence of structural errors in the hg19 genome assembly making it difficult to accurately assess variants in this region, and (2) prior literature indicating that truncating variants in CDKL5 past amino acid 938 in the canonical transcript are not given “very strong” pathogenic designation.12 However, the latter reason is irrelevant for the variant identified in individual 1, as amino acid 938 in the canonical transcript is further downstream. Therefore, we asserted that this de novo CDKL5 variant is pathogenic and clinically relevant because it is a LoF coding variant in the brain-expressed transcript.
Individual 2, a 6-year, 2-month-old Caucasian female had developmental delays, borderline intelligence, macrocephaly, mild dysmorphic features, and a paternal family history of intellectual disability (details in Supplementary Material). A pre-UDN CMA had revealed a 142-kb deletion of uncertain significance on chromosome 7q31.1 in 2013, interpreted as a risk factor for autism, Tourette syndrome, and attention deficit–hyperactivity disorder (ADHD) with reduced penetrance. Pre-UDN commercial trio ES and a reanalysis were nondiagnostic.
On GS through the UDN, an interstitial deletion of ~135 kb in 7q36.1 involving exons 8 through 55 of KMT2C (NM_170606.3) was reported. KMT2C haploinsufficiency causes Kleefstra syndrome type 2 (MIM 617768), and there was clinical overlap between this disease entity and features described in individual 2. The deletion was inherited from her father who had similar clinical characteristics. The cytogenetics lab had not reported it on initial microarray in March 2013 but upon request they re-evaluated the data and confirmed the interstitial deletion arr[hg19] 7q36.1(151,839,151-151,965,981)×1, estimating it to be approximately 127 kb in size. The reason for the cytogenetics laboratory not reporting this deletion previously was that the size was below their threshold of 300 kb and additionally deletions within KMT2C are found in healthy individuals in the Database of Genomic Variants (DGV, http://dgv.tcag.ca/dgv/app/home). However, upon further scrutiny, it is evident that these are restricted to the 5’ region (exons 2–6) of the gene (Fig. 1b). In contrast, the deletion identified in individual 2 and her father includes exons 8 through 55, extending into the 3’ region of the NM_170606.3 transcript. Deletions overlapping the exons deleted in our individual have been associated with Kleefstra syndrome 2, including a deletion of exons 2–43 and a stop gain variant in exon 12 that resulted in a truncated protein (Fig. 1b).13
We examined tissue-specific differences in expression of the isoforms of KMT2C. While NCBI RefSeq lists only one transcript for KMT2C (NM_170606.3, which corresponds to ENST00000262189.11), there are multiple splice variants in Ensembl and two (ENST00000424877.5 and ENST00000360104.7) are most highly expressed in the brain according to the GTEx database (V8). These shorter brain-expressed transcripts do not include the proximal exons that are deleted in healthy individuals, but do contain the more distal exons deleted in our individual, as well as those previously reported as pathogenic.13 With this information, the clinical laboratory agreed that the deletion in our individual and her father is likely pathogenic (personal communication) and she was given a diagnosis of Kleefstra syndrome 2.
Individual 3, an 8-year, 5-month-old African American male, had autistic features and mild developmental delays (details in Supplementary Material). On pre-UDN commercial trio ES, a novel maternally inherited pathogenic variant (c.967delA, p.[Ser323Alafs*2]) in exon 10 of X-linked OFD1 (MIM 300170) had been reported (NM_003611.2). Further evaluations were performed for specific features of an OFD1-related disorder (MIM 30084, MIM 311200, MIM 300209), but he was found to have normal cognition and no oral, digital, facial, renal, or brain abnormalities. The mother’s clinical evaluation and kidney ultrasound were normal. Since the laboratory’s report of a pathogenic variant in OFD1 was discordant with the individual’s phenotype, we examined this variant further, including the transcript that had been selected for annotation and tissue-specific expression.
The canonical transcript NM_003611.2 (ENST00000340096.11) of OFD1 is used most widely for variant annotation by commercial laboratories (personal communication). However, there are two additional NCBI RefSeq transcripts including NM_001330209.1 and NM_001330210.1 (Fig. 1c). The NM_001330209.1 transcript undergoes alternative splicing for exon 10, thus encoding a protein that lacks the corresponding 40 amino acids encoded by this exon.14 To our knowledge this transcript is not used by commercial labs in their pipelines (personal communication with four commercial labs).
We then interrogated control and disease databases to determine if there were differences in variants reported in exon 10 compared with the other exons of OFD1. In gnomAD there are nine high-confidence OFD1 LoF variants in the canonical transcript NM_003611.2. Four of these are located within exon 10 (two frameshift variants including the variant identified in individual 3, one nonsense variant, and one splice acceptor variant), and two of these four are seen in the hemizygous state (Fig. 1c). Furthermore, these two hemizygous variants are seen in a total of 15 male individuals in gnomAD. Presumably none of these individuals have OFD1-related disorders since individuals with severe pediatric disease are excluded from this database.
In the Human Gene Mutation Database (HGMD, http://www.hgmd.cf.ac.uk/ac/index.php) there are 40 LoF variants reported in OFD1, but none are in exon 10. However, in ClinVar there are four pathogenic or likely pathogenic variants reported in exon 10 with gender not specified. Two of these are among the frameshift variants reported in gnomAD, one of which is the variant also identified in individual 3 reported here. The other two variants are nonsense, of which one is reportedly associated with clinical features of an OFD syndrome, and the other without clinical details provided. We contacted three other commercial labs to determine if they had reported pathogenic/likely pathogenic variants in exon 10 of OFD1, and only one had—this was a female patient with a frameshift variant with clinical features including bifid tongue, ankyloglossia, alveolar ridging, and clinodactyly (personal communication with lab). Attempts to contact the referring provider for further details were unsuccessful. We also contacted an OFD research team with a large cohort, who reported that they had no pathogenic/likely pathogenic variants in exon 10 of OFD1 in their cohort (personal communication).
Interestingly, another male individual in our clinic was found to have a de novo frameshift variant (c.1007dupA p.[Ser337Glufs*3]) in exon 10 of OFD1 (NM_003611.2), reported as pathogenic on ES by a commercial laboratory. This patient had severe epilepsy, but like individual 3 he had no other findings suggestive of OFD1-associated disorders and upon further examination, there were six male individuals in gnomAD with the exact variant. His unaffected brother was found to have the OFD1 variant as well. He was subsequently found to have a likely pathogenic variant in ATP1A3 that was consistent with the phenotype.
There do not appear to be clear tissue-specific differences among OFD1 isoforms (https://www.gtexportal.org). However, our findings of LoF variants in exon 10 in healthy individuals, and a general lack of LoF variants in exon 10 in affected individuals, and the fact that exon 10 is spliced out in an alternative transcript, suggest that all putative damaging variants in exon 10 of OFD1 may not cause disease.
DISCUSSION
Negative results from genetic tests may be due to pathogenic variants being overlooked; less frequently variants may be declared pathogenic erroneously, resulting in a misdiagnosis.11 Many factors may account for such erroneous results, and here we describe three individuals in which molecular diagnoses were missed, or erroneously assigned, because alternative transcripts and their tissue-specific expression patterns were not considered in variant annotation.
A major factor that leads to inconsistencies in how transcripts are applied between laboratories is that there is no single, standardized transcript database utilized, although the ACMG/AMP guidelines for variant interpretation emphasize the importance of understanding the transcript architecture of genes and information about alternative splicing of genes.1 In individual 1 an exonic nonsense CDKL5 variant had been overlooked by the commercial lab because this variant was inferred as being within a noncoding region of the canonical transcript used for annotation, although the sequencing software had identified the variant. Interestingly, another individual with epileptic encephalopathy has recently been reported with a pathogenic variant within this same region of CDKL5, and similar cases with pathogenic variants being overlooked because they are in the noncoding region of the canonical transcript have been reported in SCN8A and MITF.11,15,16 Additionally, for individual 1, the guidelines used by the commercial lab for not reporting variants in the distal 3’-end of the canonical transcript were erroneously applied to the alternative isoform; the CDKL5 variant in individual 1 was in the longer exon 17 within the alternative transcript NM_001323289.1 and not distal to amino acid 938 in the canonical transcript (since pathogenicity of variants distal to this is thought to be unlikely12). Thus, for genes with multiple isoforms it is critical for sequencing laboratories to consider regions in which alternative splicing can occur as well as tissue expression of the various transcripts when variants are prioritized and assessed for pathogenicity.
Similarly, the frameshift OFD1 variant in individual 3 was reported as pathogenic because LoF variants throughout OFD1 are known to cause a spectrum of OFD1-related disorders. However, the laboratory did not take into account the presence of an alternative transcript NM_001330209.1 in which exon 10 is spliced out. Although we do not have tissue-specific expression differences among the transcripts, the presence of 15 presumably healthy male individuals in gnomAD with hemizygous OFD1 nonsense variants supports the notion that the transcript containing this exon may not be highly expressed in biologically relevant tissues. Two of the four variants reported as pathogenic or likely pathogenic in ClinVar have also been found in presumably healthy individuals in gnomAD (one in a female, and the second in six males). It is unclear whether the two other individuals reported in ClinVar have an OFD1-related disorder or another condition with overlapping features. However, clearly most individuals with putative LOF variants in exon 10 of the canonical OFD1 transcript do not have an OFD1 disorder. Individual 3 and the individual from our clinical cohort (both with OFD1 variants reported as pathogenic) reinforce the fact that not all LoF variants in a gene wherein LoF is the mechanism of disease are indeed associated with disease. Databases such as ClinVar can have erroneous data for disease associations, and when there is remarkable phenotypic discordance with the genetic results there must be a reexamination of the pathogenicity of the variants (including alternative transcripts) by the clinicians and the laboratory to avoid conferring erroneous diagnoses.17 Incorporation of next-generation phenotyping data may provide a more objective determination of whether the phenotype is consistent with the associated disease.18
When genes known to have multiple transcripts are strong candidates in the differential diagnosis, incorporating tissue-specific and temporal expression data using resources such as GTEx may help identify transcripts that are most biologically relevant.5,16 For individual 1, the canonical transcript NM_003159.2 is mostly expressed in the fetal brain and adult testes, while the alternative transcript NM_001323289.1 is the most abundant isoform expressed in the central nervous system.9 Pertinent to individual 2, the shorter alternative transcripts (that include the distal exons that were deleted in her) are the isoforms most highly expressed in the brain. The original CMA report did not consider the tissue-specific expression of the isoforms of KMT2C or location of individual 2’s deletion in relation to the other small deletions in DGV in the context of alternative transcripts, resulting in an erroneous interpretation that the deleted exons were of uncertain significance. Brain expression data from the GTEx database (V8) was helpful in this case, since the phenotype of individual 2 and her father was primarily neurologic. In both of these cases, the canonical transcript was not the most biologically relevant isoform, underscoring the importance of laboratories considering tissue-specific expression data in variant interpretation. Differential expression patterns of isoforms by tissue system continue to be updated, and continued curation of transcripts is important for accurately annotating variants.16,19,20
Reanalysis of ES or GS data is a powerful tool and should also include evaluation of alternative transcripts.5 Considering alternate transcripts allows for the selection of the most biologically relevant transcript based on tissue expression, analysis of exons that may be spliced from the canonical transcript, and detection of variants that may be intronic in the canonical transcript but protein coding in the alternate transcript. Individuals 1 and 2 had negative initial testing (panel, ES, or CMA) and then received molecular diagnoses with GS, utilizing updated variant annotation and information about transcript expression. This emphasizes the importance of allowing adequate time to elapse before further genetic testing or reanalysis of prior data so that new information may be included. Similarly, utilizing a different laboratory may overcome limitations specific to an analytic pipeline or reporting protocol.7 Our experience with individual 2 highlights the importance of applying a similar reanalysis process to existing CMA data, considering whether genes have multiple transcripts along with transcript-specific expression data when interpreting CMA results.
Finally, these cases illustrate the complexities of having multiple public databases using different languages to describe gene information that is similar but not always identical. The CCDS project is a step toward consistently annotating coding regions of human genes, but this is an imperfect process and these cases illustrate that the CCDS transcript is not always the most biologically relevant. It would be helpful for the genomics community to develop a single resource for describing all known isoforms for each gene and their biological relevance. The Clinical Genome Resource (https://clinicalgenome.org/) curation teams have made strides toward determining the significance of variation for specific genes,21 and including relevant transcript and/or expression data as part of this process would be beneficial to the genetics community.
We understand that our approach to resolving missed diagnoses and misdiagnoses may not be generalizable to all clinic workflows, since it involves resources that may not be readily available, such as reanalysis of sequencing data by an in-house bioinformatician. In addition, our approach involved testing of family members and frequent communication with the sequencing or cytogenetics laboratory directors, which may be challenging in many clinical settings, due to time constraints. However, we wish to highlight the need for clinicians to carefully consider CMA and ES or GS results, or the lack thereof, in situations where there is phenotypic mismatch and understand that these results may change over time, with our understanding of transcript expression and alternative splicing. The three examples in our study highlight how the choice of selecting only the reference/canonical transcript in variant annotation can lead to both the failure to detect pathogenic variants as well as false attribution of pathogenicity to variants in exons that are not biologically relevant.
References
Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–424.
Pan Q, Shai O, Lee LJ, Frey BJ, Blencowe BJ. Deep surveying of alternative splicing complexity in the human transcriptome by high-throughput sequencing. Nat Genet. 2008;40:1413–1415.
Baralle FE, Giudice J. Alternative splicing as a regulator of development and tissue identity. Nat Rev Mol Cell Biol. 2017;18:437–451.
Zimmermann MT. The importance of biologic knowledge and gene expression context for genomic data interpretation. Front Genet. 2018;9:670.
Bodian DL, Kothiyal P, Hauser NS. Pitfalls of clinical exome and gene panel testing: alternative transcripts. Genet Med. 2019;21:1240–1245.
McCarthy DJ, Humburg P, Kanapin A, et al. Choice of transcripts and software has a large effect on variant annotation. Genome Med. 2014;6:26.
Shashi V, Schoch K, Spillmann R, et al. A comprehensive iterative approach is highly effective in diagnosing individuals who are exome negative. Genet Med. 2019;21:161–172.
DePristo MA, Banks E, Poplin R, et al. A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nat Genet. 2011;43:491–498.
Hector RD, Dando O, Landsberger N, et al. Characterisation of CDKL5 Transcript Isoforms in human and mouse. PLoS One. 2016;11:e0157758.
Archer HL, Evans J, Edwards S, et al. CDKL5 mutations cause infantile spasms, early onset seizures, and severe mental retardation in female patients. J Med Genet. 2006;43:729–734.
Bodian DL, Schreiber Schreiber, Vilboux T, Khromykh A, Hauser NS. Mutation in an alternative transcript of CDKL5 in a boy with early-onset seizures. Cold Spring Harb Mol Case Stud. 2018;4:a002360.
Diebold B, Delepine C, Gataullina S, Delahaye A, Nectoux J, Bienvenu T. Mutations in the C-terminus of CDKL5: proceed with caution. Eur J Hum Genet. 2014;22:270–272.
Koemans TS, Kleefstra T, Chubak MC, et al. Functional convergence of histone methyltransferases EHMT1 and KMT2C involved in intellectual disability and autism spectrum disorder. PLoS Genet. 2017;13:e1006864.
Coene KL, Roepman R, Doherty D, et al. OFD1 is mutated in X-linked Joubert syndrome and interacts with LCA5-encoded lebercilin. Am J Hum Genet. 2009;85:465–481.
Epilepsy Genetics Initiative. De novo variants in the alternative exon 5 of SCN8A cause epileptic encephalopathy. Genet Med. 2018;20:275–281.
DiStefano MT, Hemphill SE, Cushman BJ, et al. Curating clinically relevant transcripts for the interpretation of sequence variants. J Mol Diagn. 2018;20:789–801.
Shashi V, McConkie-Rosell A, Schoch K, et al. Practical considerations in the clinical application of whole-exome sequencing. Clin Genet. 2016;89:173–181.
van der Donk R, Jansen S, Schuurs-Hoeijmakers JHM, et al. Next-generation phenotyping using computer vision algorithms in rare genomic neurodevelopmental disorders. Genet Med. 2019;21:1719–1725.
Mele M, Ferreira PG, Reverter F, et al. Human genomics. The human transcriptome across tissues and individuals. Science. 2015;348:660–665.
GTEx Consortium. Human genomics. The Genotype-Tissue Expression (GTEx) pilot analysis: multitissue gene regulation in humans. Science. 2015;348:648–660.
DiStefano MT, Hemphill SE, Oza AM, et al. ClinGen expert clinical validity curation of 164 hearing loss gene-disease pairs. Genet Med. 2019;21:2239–2247.
Acknowledgements
We thank the families who participated in this study. Research reported in this paper was supported by the NIH Common Fund, through the Office of Strategic Coordination/Office of the NIH Director under award number U01HG007672. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The Undiagnosed Diseases Network members are Maria T. Acosta, Margaret Adam, David R. Adams, Pankaj B. Agrawal, Mercedes E. Alejandro, Justin Alvey, Laura Amendola, Ashley Andrews, Euan A. Ashley, Mahshid S. Azamian, Carlos A. Bacino, Guney Bademci, Eva Baker, Ashok Balasubramanyam, Dustin Baldridge, Jim Bale, Michael Bamshad, Deborah Barbouth, Gabriel F. Batzli, Pinar Bayrak-Toydemir, Anita Beck, Alan H. Beggs, Edward Behrens, Gill Bejerano, Jimmy Bennet, Beverly Berg-Rood, Raphael Bernier, Jonathan A. Bernstein, Gerard T. Berry, Anna Bican, Stephanie Bivona, Elizabeth Blue, John Bohnsack, Carsten Bonnenmann, Devon Bonner, Lorenzo Botto, Brenna Boyd, Lauren C. Briere, Elly Brokamp, Gabrielle Brown, Elizabeth A. Burke, Lindsay C. Burrage, Manish J. Butte, Peter Byers, William E. Byrd, John Carey, Olveen Carrasquillo, Ta Chen Peter Chang, Sirisak Chanprasert, Hsiao-Tuan Chao, Gary D. Clark, Terra R. Coakley, Laurel A. Cobban, Joy D. Cogan, F. Sessions Cole, Heather A. Colley, Cynthia M. Cooper, Heidi Cope, William J. Craigen, Andrew B. Crouse, Michael Cunningham, Precilla D'Souza, Hongzheng Dai, Surendra Dasari, Mariska Davids, Jyoti G. Dayal, Matthew Deardorff, Esteban C. Dell'Angelica, Shweta U. Dhar, Katrina Dipple, Daniel Doherty, Naghmeh Dorrani, Emilie D. Douine, David D. Draper, Laura Duncan, Dawn Earl, David J. Eckstein, Lisa T. Emrick, Christine M. Eng, Cecilia Esteves, Tyra Estwick, Marni Falk, Liliana Fernandez, Carlos Ferreira, Elizabeth L. Fieg, Paul G. Fisher, Brent L.Fogel, Irman Forghani, Laure Fresard, William A. Gahl, Ian Glass, Rena A. Godfrey, Katie Golden-Grant, Alica M. Goldman, David B. Goldstein, Alana Grajewski, Catherine A. Groden, Andrea L. Gropman, Irma Gutierrez, Sihoun Hahn, Rizwan Hamid, Neil A. Hanchard, Kelly Hassey, Nichole Hayes, Frances High, Anne Hing, Fuki M. Hisama, Ingrid A. Holm, Jason Hom, Martha Horike-Pyne, Alden Huang, Yong Huang, Rosario Isasi, Fariha Jamal, Gail P. Jarvik, Jeffrey Jarvik, Suman Jayadev, Jean M. Johnston, Lefkothea Karaviti, Emily G. Kelley, Jennifer Kennedy, Dana Kiley, Isaac S. Kohane, Jennefer N. Kohler, Deborah Krakow, Donna M. Krasnewich, Elijah Kravets, Susan Korrick, Mary Koziura, Joel B. Krier, Seema R. Lalani, Byron Lam, Christina Lam, Brendan C. Lanpher, Ian R. Lanza, C. Christopher Lau, Kimberly LeBlanc, Brendan H. Lee, Hane Lee, Roy Levitt, Richard A. Lewis, Sharyn A. Lincoln, Pengfei Liu, Xue Zhong Liu, Nicola Longo, Sandra K. Loo, Joseph Loscalzo, Richard L. Maas, Ellen F. Macnamara, Calum A. MacRae, Valerie V. Maduro, Marta M. Majcherska, May Christine V. Malicdan, Laura A. Mamounas, Teri A. Manolio, Rong Mao, Kenneth Maravilla, Thomas C. Markello, Ronit Marom, Gabor Marth, Beth A. Martin, Martin G. Martin, Julian A. Martínez-Agosto, Shruti Marwaha, Jacob McCauley, Allyn McConkie-Rosell, Colleen E. McCormack, Alexa T. McCray, Elisabeth McGee, Heather Mefford, J. Lawrence Merritt, Matthew Might, Ghayda Mirzaa, Eva Morava-Kozicz, Paolo M. Moretti, Marie Morimoto, John J. Mulvihill, David R. Murdock, Mariko Nakano-Okuno, Avi Nath, Stan F. Nelson, John H. Newman, Sarah K. Nicholas, Deborah Nickerson, Donna Novacic, Devin Oglesbee, James P. Orengo, Laura Pace, Stephen Pak, J. Carl Pallais, Christina G.S. Palmer, Jeanette C. Papp, Neil H. Parker, John A. Phillips III, Jennifer E. Posey, Lorraine Potocki, Barbara N. Pusey, Aaron Quinlan, Wendy Raskind, Archana N. Raja, Genecee Renteria, Chloe M. Reuter, Lynette Rives, Amy K. Robertson, Lance H. Rodan, Jill A. Rosenfeld, Natalie Rosenwasser, Robb K. Rowley, Maura Ruzhnikov, Ralph Sacco, Jacinda B. Sampson, Susan L. Samson, Mario Saporta, C. Ron Scott, Judy Schaechter, Timothy Schedl, Kelly Schoch, Daryl A. Scott, Prashant Sharma, Vandana Shashi, Jimann Shin, Rebecca Signer, Catherine H. Sillari, Edwin K. Silverman, Janet S. Sinsheimer, Kathy Sisco, Edward C. Smith, Kevin S. Smith, Emily Solem, Lilianna Solnica-Krezel, Rebecca C. Spillmann, Joan M. Stoler, Nicholas Stong, Jennifer A. Sullivan, Kathleen Sullivan, Angela Sun, Shirley Sutton, David A. Sweetser, Virginia Sybert, Holly K. Tabor, Cecelia P. Tamburro, Queenie K.-G. Tan, Mustafa Tekin, Fred Telischi, Willa Thorson, Cynthia J. Tifft, Camilo Toro, Alyssa A. Tran, Brianna M. Tucker, Tiina K. Urv, Adeline Vanderver, Matt Velinder, Dave Viskochil, Tiphanie P. Vogel, Colleen E. Wahl, Stephanie Wallace, Nicole M. Walley, Chris A. Walsh, Melissa Walker, Jennifer Wambach, Jijun Wan, Lee-kai Wang, Michael F. Wangler, Patricia A. Ward, Daniel Wegner, Mark Wener, Tara Wenger, Katherine Wesseling Perry, Monte Westerfield, Matthew T. Wheeler, Jordan Whitlock, Lynne A. Wolfe, Jeremy D. Woods, Shinya Yamamoto, John Yang, Guoyun Yu, Diane B. Zastrow, Chunli Zhao, Stephan Zuchner.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosure
The authors declare no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Schoch, K., Tan, Q.KG., Stong, N. et al. Alternative transcripts in variant interpretation: the potential for missed diagnoses and misdiagnoses. Genet Med 22, 1269–1275 (2020). https://doi.org/10.1038/s41436-020-0781-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-020-0781-x
Keywords
This article is cited by
-
The status of the human gene catalogue
Nature (2023)
-
From tuberculosis bedside to bench: UBE2B splicing as a potential biomarker and its regulatory mechanism
Signal Transduction and Targeted Therapy (2023)
-
Implementing precision oncology for sarcoma patients: the CCCLMUmolecular tumor board experience
Journal of Cancer Research and Clinical Oncology (2023)