Abstract
Purpose
Women who inherit a BRCA1 or BRCA2 pathogenic variant are at high risk of developing breast and ovarian cancer. Evidence for the effectiveness and cost-effectiveness of long-term management in clinical practice is lacking. The purpose of this study was to evaluate the real-world cost-effectiveness of BRCA carrier management within a structured clinical program.
Methods
Lifetime health outcomes and costs of clinical management for female unaffected BRCA carriers aged 20 were measured using a microsimulation model. For the intervention, women could attend a high-risk clinic, undergo risk-reducing surgery, and receive annual breast screening. Input data for the model was from a clinical database of 983 BRCA carriers. The comparator was no risk management. Outcomes were discounted at 5%.
Results
The incremental cost-effectiveness ratio for the program was $32,359 to $48,263 per quality-adjusted life-year (QALY). Limiting uptake of risk-reducing salpingo-oophorectomy to <50% of carriers decreased cost-effectiveness by $7000–8000 per QALY. Achieving perfect adherence to guidelines was less cost-effective for BRCA2 due to increased risk-reducing mastectomy costs with smaller incremental health benefit.
Conclusion
Long-term management of BRCA carriers within a structured clinical program is cost-effective. Suboptimal adherence to risk management guidelines can substantially affect outcomes and is an important consideration for future studies.
Similar content being viewed by others
INTRODUCTION
Women who carry a pathogenic variant in BRCA1/2 are estimated to have a cumulative breast cancer risk of 61–79% and cumulative ovarian cancer risk of 11–53% to age 80 years.1 Genetic testing for hereditary breast and ovarian cancer is increasingly being performed in mainstream settings, and there are growing discussions about the feasibility of population-based BRCA testing of cancer-unaffected individuals.2,3 There is still, however, a significant gap in evidence for patient outcomes in clinical practice after they are identified as high-risk.4
In women known to carry a germline pathogenic variant in BRCA1 or BRCA2, several risk management strategies are recognized individually as effective and cost-effective for mitigating their increased cancer risk, including risk-reducing bilateral salpingo-oophorectomy (RRBSO) for ovarian cancer prevention, risk-reducing bilateral or contralateral mastectomy for breast cancer prevention, and early detection through annual breast screening.5,6 Uptake of these cancer risk management strategies by BRCA carriers remains suboptimal.7 Whether a particular strategy is appropriate can vary significantly depending on a woman’s age, life stage, personal values, and family history.8 Recommendations are also subject to change as new evidence becomes available. Consequently, BRCA carriers likely need the individualized guidance of specialists experienced with hereditary cancer from multiple disciplines, often over many years. Although international guidelines for cancer risk management strategies are relatively consistent, there is still substantial variation when it comes to clinical programs for long-term care once a carrier is identified, both domestically and internationally. Prior evaluations of cancer risk management in BRCA carriers are often limited to single risk management strategies in isolation, assume perfect adherence to cancer risk management, or predominately rely on hypothetical data for patient behavior.9 The benefit of these strategies is contingent on carriers adhering to evidence-based guidelines; however, no evaluations consider changes in behavior over time, the clinical framework under which carriers are managed over the many years from their initial genetic testing, and the health-care resources this would require.
Economic evaluation and simulation modeling can assist in decision-making in the absence of long-term cohort data or randomized trials by using available data to estimate which interventions may be of the most value, both clinically and economically. The incremental cost-effectiveness ratio (ICER) is a common measure used for comparing alternative interventions. The ICER is calculated by dividing the difference in costs by the difference in effectiveness \(\left( {\frac{{C_2 \ - \ C_1}}{{E_2 \ - \ E_1}}} \right)\). Effectiveness is most often reported as quality-adjusted life-years (QALYs). QALYs are the number of years of life gained after adjusting for any reduction in quality of life.
The purpose of this study was to use real-world clinical data to determine the long-term effectiveness and cost-effectiveness of cancer risk management within a structured clinical program for known BRCA1 and BRCA2 carriers.
MATERIALS AND METHODS
This was a model-based study to estimate the lifetime health and cost outcomes for BRCA carriers followed through a structured clinical program in the setting of the Australian public health-care system. Under this system all medical procedures and appointments are publicly funded with no out of pocket medical costs for patients. The model specification is provided in Table S1. The model used clinical and costing data drawn from a tertiary hospital database of 983 BRCA carriers who underwent genetic testing between 1 January 1996 and 31 December 2015. Data were available for 491 BRCA carriers for a median follow-up time of 6.57 years, and 492 BRCA2 carriers for a median of 5.86 years. The study population has been described previously.10 The study was approved by the Peter MacCallum Cancer Centre institutional review board.
Women entered the simulation aged 20, with no history of cancer and no prior cancer risk management. The intervention included participation in a multidisciplinary high-risk clinic (MDC), RRBSO, bilateral risk-reducing mastectomy (BRRM), contralateral risk-reducing mastectomy (CRRM), mammography, and breast magnetic resonance imaging (MRI). Patient uptake and adherence to breast screening, risk-reducing surgery, and an MDC was based on prospective follow-up data for BRCA carriers post–genetic testing. There are very limited data on risk management behavior for BRCA carriers who are not participating in structured high-risk follow-up programs, therefore a “do-nothing” approach (the natural history) was chosen as the comparator for the base case. For the comparator arm, women were assumed not to undergo any preventive surgery, breast screening, or to attend medical appointments unless directly related to cancer treatment. As this study was comparing risk management strategies, interventions and costs related to identification of BRCA carriers and genetic testing were excluded.
Australia’s population-based breast cancer screening program (BreastScreen) was included as an alternative comparator in the sensitivity analysis using participation rates reported in the general Australian population. BreastScreen offers two-yearly mammograms from the age of 40 years, but specifically targets women aged 50–74 years.
Women were followed over a lifetime time horizon (to age 100) with annual cycles. Primary outcomes were life-years, QALYs, health-care costs, and the ICER. Costs and health outcomes were discounted 5% annually according to Australian guidelines.11
Computer simulation
This evaluation used a previously developed simulation model for BRCA carrier natural history and cancer risk management.10 It is a validated discrete-time patient-level model in Python that simulates the development of breast and ovarian cancer in BRCA1 and BRCA2 carriers, and the effect of different clinical management strategies on lifetime health outcomes and health-care costs. Input parameters were obtained from the literature, expert opinion, and individual patient data. Additional model details including a description of the cohort used for the patient data, and a list of modeling assumptions were described previously.10
Natural history model
Parameters and data sources for the natural history are provided in Table S2. Annual probabilities for cancer onset were calculated using published prospective cancer incidence rates.1 Breast and ovarian cancer pathology was dependent on a woman’s age, gene, and the mode of detection (symptomatic, screen-detected, or occult). Probabilities for breast cancer pathology (grade, tumor size, nodal status, metastasis, and hormone receptors) were obtained from individual patient data.10
Breast cancer mortality was from the Surveillance, Epidemiology, and End Results program and incorporated hormone receptors, grade, and stage at diagnosis.12 No difference in survival between BRCA-associated and sporadic breast cancer has been shown after accounting for these prognostic factors.13 Ovarian cancer mortality was age-, stage-, and gene-specific based on a prior meta-analysis.14 Recurrence and remission were not modeled. Mortality from other causes was from Australian life tables after removing deaths attributed to breast or ovarian cancer. The model was validated for cancer onset, pathology by gene and detection mode, and mortality.10
Intervention
The intervention, a familial cancer service (FCS), was a clinical program that included optional participation in an MDC and any combination of risk management strategies over a woman’s lifetime (Table S1). Clinical effectiveness estimates for breast screening and risk-reducing surgery were based on review of the literature and included prior meta-analyses (Table S3).
Clinical pathways were developed by following current practice at the Peter MacCallum Cancer Centre in Melbourne, Australia. Uptake of risk-reducing surgery, MDC attendance, and adherence to annual breast screening were from BRCA carrier follow-up data as detailed in a previous publication (Table S3).10 Carriers attending this clinic have access to specialists in genetics, oncology, psychiatry, breast and gynecological surgery, and genetic counselors with no out of pocket medical costs.
In the model, women could attend the MDC from the age of 25 until age 64. The MDC has been shown to improve adherence to annual breast imaging, and increase uptake of RRBSO.10 Breast MRI could be performed between ages 25 and 49 inclusive per Australian guidelines.8 Mammography could be performed between ages 25 and 74, but is only recommended from age 30. Women were assigned an age at which they underwent their first mammogram and breast MRI. The length of time between annual breast screens was updated stochastically every cycle on an individual basis depending on whether a woman was of child-bearing potential (aged < 40 years), and her prior MDC attendance (Table S3).10
Women were eligible to undergo BRRM between ages 25 and 55 years inclusive, and RRBSO from age 30 until age 65 (due to limited uptake data beyond this age). Uptake probabilities were gene- and age-specific. RRBSO uptake probabilities were higher if a woman developed breast cancer, or if she attended the MDC during the previous cycle (Table S3).10 For CRRM, a woman was most likely to have surgery in the same year as her first breast cancer diagnosis (66%) and remained eligible to undergo CRRM for up to 10 years.
Costs
Details for the costs and data sources can be found in Table S4. Costs were considered from the perspective of the public health-care system. Medical costs were included for cancer treatment, consultations, surgery, breast imaging, and diagnostic workup. Costs for medical services were obtained from the Federal Government Medicare Benefits Schedule. Drug costs were from the Pharmaceutical Benefits Scheme. Hospital costs were based on the Australian-Refined Diagnosis-Related Groups and the National Hospital Costs Data Collection, a collection of costing data from Australian public hospitals.
Risk-reducing surgery costs were from individual reimbursement claims for BRCA carriers from local hospital data for surgeries performed between 2013 and 2016 (51 RRBSO, 21 BRRM). Breast reconstruction costs were included in the model if a woman had a bilateral mastectomy (for prevention or treatment), and costed by whether an autologous or implant-based reconstruction was performed. Cancer treatment was stage-specific, and costed based on a combination of the above sources, and prior publications.15,16 Breast cancer treatment patterns according to stage at diagnosis were modeled on observations of 151 BRCA carriers diagnosed with breast cancer after genetic testing, and evidence-based guidelines.8 Women diagnosed with noninvasive ductal carcinoma in situ (DCIS) did not receive chemotherapy or radiation therapy. Probabilities for diagnostic follow-up procedures following abnormal breast screens were from local BRCA carrier data. All costs are presented in 2017 Australian Dollars (AUD$), and where necessary inflated using the World Bank Consumer Price Index.17
Health state utilities
Health state utility values (utilities) for estimation of QALYs are provided in Table S5. Age-specific utilities from the Australian population were assigned to women with no history of cancer or risk-reducing surgery.18 Utilities for risk-reducing surgery, breast cancer, and ovarian cancer were obtained from a review of the literature.16,19,20 A short-term disutility was applied for the cycle in which a woman underwent an RRBSO, in accordance with a time tradeoff study in BRCA carriers.20 There are no long-term data on health-related quality of life for high-risk women following this surgery, so it was assumed to have no long-term effect. No disutility was assumed for risk-reducing mastectomy and abnormal breast screen exams21 for the base case.
Sensitivity analysis
One-way and probabilistic sensitivity analyses (PSA) were used to investigate the effect of model parameter uncertainty. Inputs for costs, utilities, risk management behavior, effectiveness of surgery and screening, cancer risks, breast cancer sojourn time, and pathology were included (Tables S2–S5). For the one-way analysis parameters were varied by the 95% confidence interval where available, or by ±50%. Correlated values, such as stage-specific breast cancer utilities and costs, were sampled using the difference method.22
Outcomes were also evaluated after (1) adjusting age at entry (20–50 years of age) and the time horizon (80–100 years of age), (2) introducing an assumption of perfect adherence to all recommended risk management interventions, (3) reduced uptake of RRBSO or BRRM, and (4) excluding availability of an MDC. An additional scenario, Australia’s population-based breast cancer screening program (BreastScreen Australia) was tested as an alternative comparator instead of the natural history. Women could commence two-yearly mammogram through BreastScreen from age 40 or 50 years of age. Additional BreastScreen inputs are provided in Table S3.
The PSA was performed by running all scenarios for 5000 sampled parameter sets (sampling number determined by convergence). BreastScreen was also included in the PSA. Cost-effectiveness acceptability curves (CEACs) were generated using the net-benefit framework.23 CEACs summarize uncertainty by visualizing the probability an intervention is cost-effective at various willingness-to-pay (WTP) thresholds. The WTP is the maximum amount a decision-maker will pay for a gain of one unit of effectiveness. The PSA was run using discount rates of 0%, 3%, 5%, and 7%.
RESULTS
Base case cost-effectiveness analysis
Discounted and undiscounted outcomes are shown in Table 1. Compared with the natural history, the FCS intervention was both more costly and more effective. The FCS was cost-effective at a willingness-to-pay threshold of AUD$50,000 per QALY saved with an ICER of AUD$32,359 per QALY for BRCA1 and AUD$48,263 per QALY for BRCA2 carriers.
Sensitivity analysis
Detailed outcomes for the one-way and PSA are presented in the Supplementary Materials (Figs. S1–S4, Tables S6–S9).
Cost-effectiveness improved for women entering the model at an older age, except for BRCA2 carriers entering the model at age 25 (Tables S6, S7). Shortening the time horizon by 20 years (to age 80) only slightly raised cost-effectiveness estimates.
The ICER per QALY saved was most sensitive to the cost and risk reduction of BRRM for BRCA1 carriers (Fig. 1). Nevertheless, all discounted results for BRCA1 remained under a AUD$50,000 WTP threshold for the one-way analysis (range AUD$17,964 to AUD$46,744). BRCA2 outcomes were sensitive to breast cancer risk and BRRM cost parameters (range AUD$29,627 to AUD$84,473). The ICER was highly sensitive to the discount rate used for health outcomes (Table 1, Supplementary Fig. S3).
Introducing the population-based breast screening program as a comparator did not significantly alter the ICER (Table S8). An assumption of perfect adherence to risk management guidelines led to an FCS being more effective and more costly than when using actual adherence rates (Table 2). Lowering uptake rates for RRBSO (46–49% overall uptake) or BRRM (28% overall uptake) led to a decrease of 0.05–0.11 life-years and 0.05–0.10 QALYs compared with the base case (Table S9). Reduction in uptake of RRBSO had a greater impact on incremental cost-effectiveness, increasing the ICER per QALY to $40,000 for BRCA1 carriers and $55,500 for BRCA2 carriers.
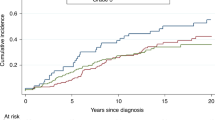
The PSA results are shown in Figs. 2, 3 and Supplementary Figs. S3, S4. For a WTP threshold of AUD$50,000 per QALY an FCS was cost-effective in 98.2% of BRCA1 simulations, but only 40.6% of BRCA2. Once the WTP reached AUD$100,000 per QALY, 99.5% of BRCA2 simulations were cost-effective.
The FCS intervention was the preferred strategy if the WTP threshold was at least AUD$29,000 per QALY for BRCA1 and AUD$57,000 per QALY for BRCA2. Results were slightly more favorable if quality of life was not considered, with a necessary WTP threshold of AUD$26,000 per LYG for BRCA1 and AUD$49,000 per LYG for BRCA2 (Supplementary Fig. S4). Removing the availability of an MDC in the PSA resulted in a service with lower costs, but it was also less effective, particularly for BRCA1 carriers (Fig. 3).
DISCUSSION
This study found long-term management through a structured multidisciplinary familial cancer service is clinically effective and cost-effective for BRCA1 and BRCA2 carriers. This is the first study that combines a BRCA-specific natural history disease model with clinical data to evaluate the long-term cost-effectiveness of BRCA carrier cancer risk management in a real-world clinical setting.
Empirical data on long-term outcomes for clinical management of BRCA carriers once their genetic status is known are mostly absent. Real-world uptake of risk management strategies is affected by many factors, including a woman’s personal history, preferences, her age and life stage, and is also heavily influenced by physicians’ recommendations.10,24 Perfect adherence to breast screening and preventive surgeries is frequently assumed in prior model-based evaluations of BRCA risk management.9 This can overestimate the clinical effectiveness of interventions, as well as underestimate the substantial cost of preventive options, and the resources required to maintain engagement with carriers over many years.
There are several strengths to the current study. We had access to a large clinical database of BRCA carriers followed prospectively from the time of genetic testing. A wide range of model inputs were able to be extracted relating to the natural history, patient behavior, and medical costs. The one-way sensitivity analysis found the cost of BRRM was one of the main drivers of cost-effectiveness. This is the first cost-effectiveness study in BRCA carriers to include the actual reported hospital costs for BRRM with breast reconstruction, which were up to AUD$25,000 higher than estimates used in prior economic evaluations.2,25 The estimates in this study included costs related to breast reconstruction, as well as readmission and corrective surgery due to short-term complications (both medical and cosmetic). Between 20% and 30% of women experience complications from BRRM within the first month of surgery,26 and up to 50% of women require further unexpected corrective surgery within two years.27 Studies that only include the cost of immediate surgery are therefore likely to overestimate the cost-effectiveness of this risk management strategy. By factoring in the higher cost for BRRM and the substantial recurring costs of ongoing follow-up, the cost-effectiveness results in the current study are perhaps less favorable than would be expected for this high-risk group. Health outcomes were highly sensitive to the discount rate. In jurisdictions where the recommended discount rate is lower, long-term management is more likely to be cost-effective for both BRCA1 and BRCA2 carriers.
A recent study of trends in risk management uptake reported substantial international variation in the uptake of different strategies, particularly for BRRM.7 Our model was based on data obtained from a comparatively well-resourced clinic, where high-risk individuals are contacted regularly for follow-up. Our adherence rates may therefore be higher than at other centers. When uptake of RRBSO was limited to less than 50% of BRCA carriers, the ICER increased by between $7000 and $8000 per QALY. Improving risk management adherence and management through a multidisciplinary high-risk management clinic for BRCA2 carriers was less likely to be cost-effective at lower WTP thresholds compared with BRCA1 carriers (Table 2, Fig. 3). This suggests our current model of care may need to be further optimized to be gene-specific. This aligns with emerging clinical data; differential breast screening intervals based on genotype have recently been proposed.28 It has also been suggested that BRRM may lead to a survival benefit in BRCA1 carriers but not BRCA2 due to differences in breast cancer–specific mortality; however, this analysis was based on short-term follow-up with few events.29,30 Improved risk stratification of BRCA2 carriers through adding a polygenic risk score (PRS) may help identify the women at highest risk,31 thereby enabling them to be actively targeted to prioritize early intervention. Stratifying these women will become increasingly important as the availability of genetic testing is widened, as current penetrance estimates are from clinic populations ascertained based on being high-risk and therefore may not be appropriate for BRCA carriers identified in the general population. The flexibility of the simulation model used in this study means it could be modified in future studies to potentially optimize BRCA carrier management in light of new discoveries, such as the PRS or new risk-reducing medications, in lieu of the long-term clinical data being available.
Limitations of the current study include uncertainty around cancer treatment costs, quality of life, and the unobservable aspects of BRCA-specific natural history for breast and ovarian cancer. Very little is known about risk management behavior and health-care provision for BRCA carriers in a community setting, including for women who may be seeing individual specialists for regular follow-up. For this reason, the natural history of disease was used as a comparator for the base case. It is unlikely that women who are aware of their BRCA status, but not seen through a familial cancer service, would not act at all to mitigate their increased risk, so this choice of comparator would likely overestimate the cost-effectiveness of the current program.
There are very few reports of the stage-specific costs of treating breast cancer.32 Hospital costs for chemotherapy alone have been reported to be AUD$15,000 per breast cancer patient, even exclusive of adverse events.33 We attempted to account for all breast cancer–related costs, and set a wide range for the sensitivity analysis to compensate for this. BRCA carrier status can also be used to guide cancer treatment, including the use of poly (ADP-ribose) polymerase (PARP) inhibitors, which prolong progression-free survival in BRCA-associated ovarian34 and metastatic breast cancer.35 The substantial cost of PARP inhibitors was included only for relapsed ovarian cancer in this study, and will need to be considered in future analyses as this treatment becomes increasingly available for both relapsed and newly diagnosed disease. Due to substantial differences between health-care systems the current findings may not be generalizable to other countries; country-specific health-care costs, utilities, and uptake rates may be added to apply the model to these different settings.
Caution must also be used when making decisions based on quality of life estimates.36 Health state utility values for risk management and breast and ovarian cancer vary widely depending on the population and valuation tool.19,37 Furthermore, the long-term quality of life for high-risk women following life-changing surgeries such as BRRM and RRBSO is unknown. In the short-term, BRCA carriers who undergo RRBSO while still premenopausal have similar overall quality of life to comparator groups one year after surgery.38 In the general population, premature surgical menopause has been associated with cognitive and sexual dysfunction, and increased cardiovascular morbidity,39 but how this translates to long-term quality of life and mortality this high-risk group is still under investigation.
In summary, a familial cancer service is a cost-effective approach for clinical management of women with germline pathogenic variants in BRCA1 and BRCA2. These women face a range of complex and life-changing decisions, often extending many years beyond the initial receipt of their genetic test results. A specialist multidisciplinary approach is likely necessary to maximize clinical outcomes in this group given their unique lifelong needs. This approach also provides indirect health benefits related to family relationships and psychosocial support, but these are difficult to include in an economic model. It is estimated that over 90% of BRCA carriers in the general population remain unidentified.40 Eligibility for genetic testing for cancer predisposing genetic variants is being increasingly widened, and population-based genetic testing may be available in the near future. Consequently, being able to evaluate and implement the most effective and cost-effective means of managing these individuals is increasingly vital for both their individual health outcomes as well as wider health service planning—decisions that need to be made in real-time and cannot wait for the decades of follow-up required to resolve them through prospective BRCA carrier cohort data.
Code availability
The code for the miBRovaCAre model used in this study is available from the corresponding author upon request.
References
Kuchenbaecker KB, Hopper JL, Barnes DR, et al. Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA. 2017;317:2402–2416.
Manchanda R, Patel S, Gordeev VS, et al. Cost-effectiveness of population-based BRCA1, BRCA2, RAD51C, RAD51D, BRIP1, PALB2 mutation testing in unselected general population women. J Natl Cancer Inst. 2018;110:714–725.
Zhang L, Bao Y, Riaz M, et al. Population genomic screening of all young adults in a health-care system: a cost-effectiveness analysis. Genet Med. 2019;21:1958–1968.
Moyer VA. Force USPST. Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer in women: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160:271–281.
Grann VR, Patel PR, Jacobson JS, et al. Comparative effectiveness of screening and prevention strategies among BRCA1/2-affected mutation carriers. Breast Cancer Res Treat. 2011;125:837–847.
Norman RP, Evans DG, Easton DF, Young KC. The cost-utility of magnetic resonance imaging for breast cancer in BRCA1 mutation carriers aged 30-49. Eur J Health Econ. 2007;8:137–144.
Metcalfe K, Eisen A, Senter L, et al. International trends in the uptake of cancer risk reduction strategies in women with a BRCA1 or BRCA2 mutation. Br J Cancer. 2019;121:15–21.
eviQ. Cancer treatments online, 2016. https://www.eviq.org.au/. Accessed 7 July 2016.
Petelin L, Trainer AH, Mitchell G, Liew D, James PA. Cost-effectiveness and comparative effectiveness of cancer risk management strategies in BRCA1/2 mutation carriers: a systematic review. Genet Med. 2018;20:1145–1156.
Petelin L, Hossack L, Mitchell G, Liew D, Trainer AH, James PA. A microsimulation model for evaluating the effectiveness of cancer risk management for BRCA pathogenic variant carriers: miBRovaCAre. Value Health. 2019;22:854–862.
Commonwealth Government of Australia. Guidelines for preparing submissions to the Pharmaceutical Benefits Advisory Committee [Version 5.0]. Department of Health, Canberra, Australia; 2016.
Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Incidence—SEER 18 regs research data (1992–2014): National Cancer Institute 2017. https://seer.cancer.gov/seerstat/ Accessed 24 August 2017.
Copson ER, Maishman TC, Tapper WJ, et al. Germline BRCA mutation and outcome in young-onset breast cancer (POSH): a prospective cohort study. Lancet Oncol. 2018;19:169–180.
Candido-dos-Reis FJ, Song H, Goode EL, et al. Germline mutation in BRCA1 or BRCA2 and ten-year survival for women diagnosed with epithelial ovarian cancer. Clin Cancer Res. 2015;21:652–657.
Verry H, Lord SJ, Martin A, et al. Effectiveness and cost-effectiveness of sentinel lymph node biopsy compared with axillary node dissection in patients with early-stage breast cancer: a decision model analysis. Br J Cancer. 2012;106:1045–1052.
Gordon LG, Scuffham PA, Beesley VL, et al. Medical costs and outcomes for Australian women with ovarian cancer: a patient-level analysis over 2.5 years. Int J Gynecol Cancer. 2010;20:757–765.
World Bank, World Development Indicators, 2018. https://databank.worldbank.org/source/world-development-indicators. Accessed 15 August 2018.
Richardson J, Iezzi A, Khan MA, Maxwell A. Validity and reliability of the Assessment of Quality of Life (AQoL)-8D multi-attribute utility instrument. Patient. 2014;7:85–96.
Peasgood T, Ward SE, Brazier J. Health-state utility values in breast cancer. Expert Rev Pharmacoecon Outcomes Res. 2010;10:553–566.
Grann VR, Patel P, Bharthuar A, et al. Breast cancer-related preferences among women with and without BRCA mutations. Breast Cancer Res Treat. 2010;119:177–184.
Rijnsburger AJ, Essink-Bot ML, van Dooren S, et al. Impact of screening for breast cancer in high-risk women on health-related quality of life. Br J Cancer. 2004;91:69–76.
Ren S, Minton J, Whyte S, Latimer NR, Stevenson M. A new approach for sampling ordered parameters in probabilistic sensitivity analysis. Pharmacoeconomics. 2018;36:341–347.
Briggs AH, Weinstein MC, Fenwick EA, et al. Model parameter estimation and uncertainty analysis: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force Working Group-6. Med Decis Making. 2012;32:722–732.
Buchanan AH, Voils CI, Schildkraut JM, et al. Adherence to recommended risk management among unaffected women with a BRCA mutation. J Genet Couns. 2017;26:79–92.
Tuffaha HW, Mitchell A, Ward RL, et al. Cost-effectiveness analysis of germ-line BRCA testing in women with breast cancer and cascade testing in family members of mutation carriers. Genet Med. 2018;20:985–994.
Moberg IO, Schou Bredal I, Schneider MR, Tonseth KA, Schlichting E. Complications, risk factors, and patients-reported outcomes after skin-sparing mastectomy followed by breast reconstruction in women with BRCA mutations. J Plast Surg Hand Surg. 2018;52:234–239.
van Verschuer VMT, Mureau MAM, Heemskerk-Gerritsen BAM, et al. Long-term outcomes of bilateral direct-to-implant breast reconstruction in women at high breast cancer risk. J Plast Surg Hand Surg. 2018;52:245–252.
Phi XA, Saadatmand S, De Bock GH, et al. Contribution of mammography to MRI screening in BRCA mutation carriers by BRCA status and age: individual patient data meta-analysis. Br J Cancer. 2016;114:631–637.
Heemskerk-Gerritsen BAM, Jager A, Koppert LB, et al. Survival after bilateral risk-reducing mastectomy in healthy BRCA1 and BRCA2 mutation carriers. Breast Cancer Res Treat. 2019;177:723–733.
Evans DG, Howell SJ, Howell A. Should unaffected female BRCA2 pathogenic variant carrriers be told there is little or no advantage from risk reducing mastectomy? Fam Cancer. 2019;18:377–379.
Kuchenbaecker KB, McGuffog L, Barrowdale D. et al. Evaluation of polygenic risk scores for breast and ovarian cancer risk prediction in BRCA1 and BRCA2 mutation carriers. J Natl Cancer Inst. 2017;109:djw302.
Sun L, Legood R, Dos-Santos-Silva I, Gaiha SM, Sadique Z. Global treatment costs of breast cancer by stage: a systematic review. PLoS ONE. 2018;13:e0207993.
Sakata S, Cronk M. The financial burden of using Oncotype Dx for patients with lymph node-negative and estrogen receptor-positive breast cancer in Australia. Asia Pac J Clin Oncol. 2014;10:94–95.
Moore K, Colombo N, Scambia G, et al. Maintenance olaparib in patients with newly diagnosed advanced ovarian cancer. N Engl J Med. 2018;379:2495–2505.
Robson M, Im SA, Senkus E, et al. Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N Engl J Med. 2017;377:523–533.
Neumann PJ, Cohen JT. QALYs in 2018—advantages and concerns. JAMA. 2018;319:2473–2474.
Bromley HL, Petrie D, Mann GB, Nickson C, Rea D, Roberts TE. Valuing the health states associated with breast cancer screening programmes: a systematic review of economic measures. Soc Sci Med. 2019;228:142–154.
Vermeulen RFM, Beurden MV, Korse CM, Kenter GG. Impact of risk-reducing salpingo-oophorectomy in premenopausal women. Climacteric. 2017;20:212–221.
Rocca WA, Bower JH, Maraganore DM, et al. Accelerated accumulation of multimorbidity after bilateral oophorectomy: a population-based cohort study. Mayo Clin Proc. 2016;91:1577–1589.
Manchanda R, Blyuss O, Gaba F, et al. Current detection rates and time-to-detection of all identifiable BRCA carriers in the Greater London population. J Med Genet. 2018;55:538–545.
Acknowledgements
We thank the Peter MacCallum Cancer Centre Core Research Computing Facility. This work was supported by the Cancer Council New South Wales (CCNSW) Strategic Research Partnership scheme (grant number SRP12–03); and through an Australian Government Research Training Program (RTP) Scholarship. Neither funder had a role in the design of the study; the collection, analysis, and interpretation of the data; or the decision to approve publication of the finished manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
L.P.’s salary has been funded by an Australia Government Research Training Program Scholarship, and by a Cancer Council New South Wales Strategic Research Partnership scheme (grant number SRP12–03). Neither funder had a role in the design of the study, the collection, analysis, and interpretation of the data, and the decision to approve publication of the final manuscript. Over the past 3 years, D.L. has participated in advisory boards and/or received honoraria from AbbVie, Astellas, AstraZeneca, Bristol-Myers Squibb, Novartis, Pfizer, Sanofi, and Shire for work unrelated to this study. He declares no conflict of interest specifically related to this study. Over the past 3 years, he has attended conferences of the American Heart Association, the European Society of Cardiology, and the Cardiac Society of Australian and New Zealand. L.H. has received compensation for participating in an advisory panel for Pfizer. The other authors declare no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Petelin, L., Hossack, L., Shanahan, M. et al. Cost-effectiveness of long-term clinical management of BRCA pathogenic variant carriers. Genet Med 22, 831–839 (2020). https://doi.org/10.1038/s41436-020-0751-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-020-0751-3
Keywords
This article is cited by
-
The Difference Method Approach for Sampling Order Constrained Parameters: An Improved Implementation and Important Limitations
PharmacoEconomics (2024)
-
“There should be one spot that you can go:” BRCA mutation carriers’ perspectives on cancer risk management and a hereditary cancer registry
Journal of Community Genetics (2023)
-
Longitudinal adherence to breast cancer surveillance following cancer genetic testing in an integrated health care system
Breast Cancer Research and Treatment (2023)