Abstract
Purpose
Individuals with mosaic pathogenic variants in the FBN1 gene are mainly described in the course of familial screening. In the literature, almost all these mosaic individuals are asymptomatic. In this study, we report the experience of our team on more than 5,000 Marfan syndrome (MFS) probands.
Methods
Next-generation sequencing (NGS) capture technology allowed us to identify five cases of MFS probands who harbored a mosaic pathogenic variant in the FBN1 gene.
Results
These five sporadic mosaic probands displayed classical features usually seen in Marfan syndrome. Combined with the results of the literature, these rare findings concerned both single-nucleotide variants and copy-number variations.
Conclusion
This underestimated finding should not be overlooked in the molecular diagnosis of MFS patients and warrants an adaptation of the parameters used in bioinformatics analyses. The five present cases of symptomatic MFS probands harboring a mosaic FBN1 pathogenic variant reinforce the fact that apparently asymptomatic mosaic parents should have a complete clinical examination and a regular cardiovascular follow-up. We advise that individuals with a typical MFS for whom no single-nucleotide pathogenic variant or exon deletion/duplication was identified should be tested by NGS capture panel with an adapted variant calling analysis.
Similar content being viewed by others
INTRODUCTION
Marfan syndrome (MIM 154700, MFS) is a hereditary connective tissue disorder with an estimated incidence of 1 in 5,000 individuals. In this disease, many systems are affected with great phenotypic variability and life-threatening complications, such as the cardiovascular system, with thoracic aortic aneurysms and dissections; ocular system, with ectopia lentis; and skeletal system, with recognizable features such as scoliosis, long bone overgrowth, arachnodactyly, and pectus deformity. The clinical diagnosis is based on the revised Ghent nosology.1 Heterozygous pathogenic variants in the FBN1 gene, encoding fibrillin-1, an extracellular matrix protein, are found in the majority of patients with MFS (1,850 different pathogenic variants described in the UMD-FBN1 database2 (http://www.umd.be/FBN1/). A clear family history is apparent in the majority of MFS probands, whereas the disease arises de novo in about 25% of the cases.
Mosaicism defines an individual who has developed from a single fertilized egg and has two or more populations of cells with distinct genotypes, due to postzygotic de novo variants.3 A variant can occur in a somatic cell and be contained in only a few tissues (somatic mosaicism), it can occur in a germline cell (germline/gonadal mosaicism), or it can occur in an early precursor cell giving a mixed somatic and germline mosaicism (gonosomal mosaicism).4 A transmission of the variation to descendants is possible if the mosaic is present in a germ cell, which is the case in germline and gonosomal mosaicism. The most obvious example of somatic mosaicism is cancer, but mosaicism has also been described extensively in autosomal dominant diseases. The phenomenon was initially highlighted through the observation of localized or segmental forms of cutaneous diseases, such as neurofibromatosis type 1.5 Another example is Proteus syndrome, which is caused by somatic mosaicism for a pathogenic variant presumed lethal in the nonmosaic state.6,7
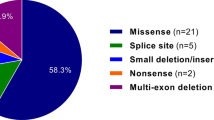
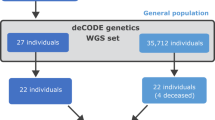
Mosaicism was long suspected to exist in MFS because of the high rate of sporadic cases.8 Our team performs systematic diagnostic study of the FBN1 gene in patients suspected for MFS since the early 1990s. More than 5,000 MFS-suspected probands have been tested for molecular diagnosis, either by Sanger sequencing or by next-generation sequencing (NGS) capture panel, and 1,961 were shown to harbor at least one heterozygous pathogenic variant in the FBN1 gene.9 Among these MFS patients with a pathogenic variant in the FBN1 gene, a family history was documented in 65%, while among the remaining apparently sporadic cases, a de novo occurrence could be confirmed in 258 cases, representing 13% of all the patients (Fig. 1). Moreover, a parental mosaicism was found in 23 cases, notably the first case of both somatic and gonosomal mosaicism reported in MFS.10 At the clinical level, all 23 cases were asymptomatic. In the literature, only two cases of symptomatic MFS patients exhibit a FBN1 mosaic pathogenic variant.11,12 The past 20 years have completely altered the diagnosis of MFS and related disorders, first through the availability of capillary Sanger sequencers followed by that of the NGS technologies.13 With the latter applied to a capture panel, we discovered five cases of mosaicism in five probands for whom the diagnosis of MFS had already been ascertained at the clinical level. This study reports on these unusual and underestimated molecular events that should be routinely looked for.
MATERIALS AND METHODS
Patients
All the patients included were followed either by the Centre National Maladies Rares—Syndrome de Marfan et apparentés, the French National Reference Centre in Paris, or by an affiliated regional Center of Expertise. Clinical diagnosis was established according to the revised Ghent nosology.1 Patients were examined by several physicians: cardiologists, ophthalmologists, geneticists, rheumatologists, or pediatricians (depending on their age) with specific evaluation of clinical features included in MFS. Systematic slit-lamp examination, cardiac ultrasonography and radiological investigations were also performed. Aortic diameter was evaluated at the root and at the tubular portion of the ascending aorta at end diastole. Aortic aneurysm was defined as a measure above mean + 2 standard deviations (Z score >2) as described by Campens et al.14 Dural ectasia was looked for by imaging. Systemic score was calculated as described in the revised Ghent nosology.1 Between 1996 and 2020, blood samples were obtained for more than 5,000 consecutive unselected probands referred nationwide to our laboratory for molecular diagnosis of suspected MFS.
DNA amplification and variant detection
Genomic DNA was isolated from peripheral blood leukocytes with a DNA Blood 4K kit (Perkin Elmer®) on Chemagicstar (Hamilton®) according to the manufacturer’s instructions. Originally, the FBN1 gene was systematically screened in patients suspected of MFS by bidirectional Sanger sequencing as previously reported.9 Since 2014, the FBN1 gene has been screened on MiSeq (Illumina®) by NGS (on more than 3,000 patients) using MARFAN MASTR Assay (Multiplicom®) or a custom capture array (NimbleGen, Roche®) designed to capture FBN1 gene (NM_000138.4; genome build hg19) and 27 other genes already known to be associated with Marfan syndrome and related diseases (total size of the target: 132 kb). Variant calling is performed through CLC Genomics Workbench v10.1.1 (Qiagen® Bioinformatics). Once a single-nucleotide or a small insertion/deletion pathogenic variant is found in this way, it is systematically confirmed by bidirectional Sanger sequencing of the altered exon. When the pathogenic variant alters the regional restriction map, the presence of the variation is also checked by polymerase chain reaction (PCR)/digestion using the appropriate restriction enzyme. When possible, familial segregation of pathogenic variants is investigated. Description of sequence variants is performed according to Human Genome Variation Society nomenclature.15 In brief, complementary DNA (cDNA) numbering with +1 corresponds to the A of ATG, the translation initiation codon in the reference sequence (FBN1: NM_000138.4). Exon numbering is historically made considering that exon 1 carries the initiation codon.
Copy-number variation (CNV) analysis
Before the routine use of the NimbleGen custom capture array, CNVs in the FBN1 gene were searched for with multiplex ligation-dependent probe amplification (MLPA, MRC-Holland®) on 53 of the 65 exons of FBN1 using a ABI-3130XL analyzer, and analyzed using Coffalyser.Net (MRC-Holland®). For patients screened using the NimbleGen custom capture array, CNV analysis was based on a comparison of normalized coverage depths for each amplicon to those of a group of 24 patients from the same experiment (CNV ratio). All CNVs were confirmed by quantitative PCR using specific PCR primers and SYBR™ Green Master Mix (Applied Biosystem®) on an ABI 7500 Fast and analyzed with the 7500 Fast Real-Time PCR System software (Applied Biosystem®). Quantification was normalized using the expression of the two housekeeping genes (PBGD and RB1).
Long-range PCR
A 7-kb fragment comprising FBN1 exons 44 to 50 was amplified using an Expand® High Fidelity PCR System (Sigma-Aldrich®) on a PeqSTAR® thermal cycler (UNO96G), with the following program: initial denaturation: 2 minutes at 94 °C; 10 cycles (denaturation: 10 seconds at 94 °C, annealing: 30 seconds at 60 °C, elongation: 15 min at 68 °C); 25 cycles (denaturation: 15 seconds at 94 °C, annealing: 30 seconds at 60 °C, elongation: 15 minutes + 20 seconds at 68 °C); final elongation: 7 minutes at 68 °C. Multiple amplification primers were designed in introns 44 and 49, and sequentially used to amplify shorter and shorter fragments. The shortest amplified fragment was then sequenced and analyzed using Seqscape® (Applied Biosystem®) to identify breakpoints in these introns.
RESULTS
Molecular aspects
Of 5,000 MFS suspected patients, 1,961 probands were shown to harbor at least one heterozygous pathogenic variant in the FBN1 gene.9 Approximately half of these were identified by NGS capture panel routinely performed since 2014. This last technology allowed the identification of five mosaic pathogenic variants in the FBN1 gene in five different probands. In these five cases, the entire FBN1 gene was covered with a minimum depth of 90 reads (mean depth: 422, 453, 478, 235, and 927 respectively for patients 1 to 5). In four cases (patients 1 to 4), four different single-nucleotide variants were identified with abnormally low allelic fraction (26%, 18%, 20%, and 24% respectively). The presence of these mosaic variants was confirmed using targeted Sanger sequencing, and PCR followed by enzymatic restriction when appropriate (Fig. 2). The variant found in patient 1 (c.3037G>A–p.[Gly1013Arg]) affects a highly conserved glycine, consensus in the transforming growth factor-β binding protein domain 3, and has already been reported in ten probands in UMD-FBN1 database. Prediction tools were in favor of a pathogenic effect for this variation (UMD-Predictor®,16 PolyPhen-217). In patient 2, an intronic variant was detected in intron 25 (c.3208+2T>A). This variant affects the consensus donor splice site of intron 25 and is predicted to cause an abnormal splicing of the intron and a major impact at the protein level. The two mosaic variants identified in patients 3 and 4 affect a cysteine, in calcium-binding epidermal growth factor domains 12 and 19, respectively. These two pathogenic variants, already reported in UMD-FBN1 database, are known to affect proper disulfide bond formation and to disrupt domain conformation. In the case of patient 5, a mosaic deletion of exons 45 to 49 in the FBN1 gene was suspected during CNV analysis since CNV ratios were intermediate (ranging from 0.73 to 0.78) for these five exons (Fig. 3). Quantitative PCR confirmed a 75–80% relative quantity of exons 45, 47, and 49, compared with controls. Long-range PCR was performed to determine the deletion breakpoints and identified a 9,128-bp deletion (c.5546-750_6163 + 1205del). This deletion of five exons is predicted to lead to an in-frame deletion of 206 amino acids but this could not be verified by a transcript analysis.
(a) Scatter plot of copy-number variation (CNV) for the next-generation sequencing (NGS) capture panel (28 genes). (b) CNV ratio data from NGS for exons 42 to 52 in the FBN1 gene. (c) Relative quantification of exon 49 (samples from left to right: patient’s mother, patient blood sample 1, patient blood sample 2, heterozygous deletion control, negative controls 1, 2, and 3). Similar profiles were obtained for exons 45 and 47. (d) Schematic view of the deletion breakpoints in the FBN1 gene in this proband.
Clinical aspects
The five probands with a mosaic pathogenic variant described in this report were sporadic cases. None of them had children, and their unaffected parents did not carry the pathogenic variant when the samples were available. Four of five were diagnosed during infancy and displayed classical MFS features usually found in heterozygote patients, with ascending aortic dilatation and/or ectopia lentis, and a systemic score ranging from 6 to 9. The last one (patient 4) was diagnosed after an emergency surgery for type A aortic dissection at 48 years old; the clinical examination was incomplete for him. The detailed clinical features of these probands are summarized in Table 1, as well as with the clinical features of the two symptomatic mosaic patients from the literature.11,12
DISCUSSION
In the present study, we describe five MFS probands harboring mosaic FBN1 pathogenic variants. At the clinical level, these mosaic patients displayed typical MFS features with the involvement of the skeletal, cardiovascular, and/or ocular systems. These findings were unexpected since mosaicism is rare in patients with typical MFS in the literature, which almost exclusively reports asymptomatic mosaic parents in the context of familial studies. Indeed, our team reported the first case of paternal mosaicism with both somatic and gonadal mosaicism for a FBN1 gene variant.10 In sporadic cases of MFS, it is important to find out whether the variation occurred de novo or if it has been inherited, to properly assess the risk of recurrence for another child. In our experience and in the literature, individuals harboring mosaic pathogenic variants in the FBN1 gene are usually asymptomatic.2,18,19,20,21,22,23 As a precaution, a follow-up in cardiology is recommended for these patients. In the literature, mosaicism is a very rare event in MFS patients since only two reports mention symptomatic probands mosaic for a FBN1 pathogenic variant.11,12 The first case is a sporadic case of MFS diagnosed at a young age for whom a mosaic deletion of exons 13 to 49 was reported. The second report is a symptomatic proband’s mother who was shown to harbor the familial intronic variant as a mosaic.
The five present cases of symptomatic probands mosaic for pathogenic variants in the FBN1 gene reinforce the fact that caution is warranted in the clinical follow-up of parental mosaic individuals. Another interesting point is that somatic mosaicism could also sometimes explain the mild and incomplete form of the disease often seen in the patients referred to MFS clinics for diagnosis.
We have identified an uncommon phenomenon in the molecular diagnosis of MFS patients. Indeed, for some MFS patients, the causal molecular event may have been missed due to lack of knowledge and technical sensitivity. In the literature, the power of MLPA for the detection of mosaicism in blood samples has been shown to be low, since it could not detect duplication mosaics below 40% or deletion mosaics below 30%.24 MLPA is therefore not an effective method for the detection of low-grade mosaicisms and its wide use in the last decade could explain why no mosaics for major rearrangements were seen at the time. Interestingly, targeted Sanger sequencing allows detection of mosaic variants with far lower allele fractions, as low as 8% according to a recent study.25 However, the conditions in which this percentage was obtained are not applicable to routine screening by Sanger sequencing. In our experience, enzymatic restriction is more sensitive than Sanger sequencing and useful in targeted familial screening to accurately detect parental mosaicism. NGS appears to be the ideal method to detect mosaic variants, provided that background signal is low enough to be to detect mosaic variants. Therefore, each capture method using custom bioinformatics analyses should be adapted to properly query for this molecular phenomenon and should be combined with additional Sanger sequencing. The lowest allele fraction detected in this study was 18%; however, the minimal detectable allele fraction is expected to be lower with an adapted bioinformatics analysis. Of note, we were able to detect a 4% minor allele fraction at another locus in the context of parental mosaicism (unpublished data). Furthermore, parental samples are tested using NGS technology in our laboratory to accurately detect parental mosaicism, as also suggested by Brewer et al.25 This is particularly warranted to properly evaluate the risk of recurrence that another child will be heterozygous for the familial FBN1 pathogenic variant.
In our experience acquired from mosaic parents, the rate of heterozygous cells was identical in buccal swab and blood sample. Unfortunately, we were not able to test any other tissue from the five MFS patients with a FBN1 mosaic pathogenic variant, but we can assume that in affected tissues, cardiovascular and ophthalmological tissues for instance, the rate of heterozygous cells might be higher. Further studies need to be done on other tissues to evaluate the presence of mosaic pathogenic variants in the FBN1 gene.
Taken together, the seven mosaic variants detailed in this study and in the literature are three missense variants, two variants with a predicted impact on splicing, and two deletions of several successive exons. Interestingly, three of the seven mosaic variants are located in the “neonatal region” corresponding to exons 24 to 32 of the FBN1 gene. This region has been associated with more severe phenotypes, including neonatal MFS.26 Moreover, the missense pathogenic variant identified in patient 1 was also found in five other probands in our laboratory and all of them displayed a severe form (infantile or neonatal) of the disease. Since patient 1 did not display a particularly severe form of the disease, it could be speculated that a mosaic state could influence the severity of the disease. Furthermore, we can hypothesize that the particularly deleterious consequences of these seven variants may explain why these mosaic patients are symptomatic.
Interestingly, combining the results from this report and from the literature, two mosaic patients of seven concerned a deletion of several exons in the FBN1 gene. This type of molecular event may be difficult to identify and the threshold for CNV analysis must be set keeping in mind the possibility of mosaicism.
These five pathogenic variants have been identified through NGS capture panel technology with a high mean depth on the entire FBN1 gene (>90 reads). We hypothesized that some cases of mosaicisms could have been missed while performing screening for FBN1 variants using Sanger sequencing before 2014. We advise that individuals with a typical MFS for whom no pathogenic single-nucleotide variant or exons deletion/duplication was identified should be tested by NGS capture panel with an adapted variant calling analysis.
Conclusion
Herein, we report five cases of symptomatic MFS patients with a mosaic FBN1 pathogenic variant, discovered in the course of molecular diagnosis thanks to NGS capture panel technology. This uncommon molecular event should not be overlooked and warrants adapting the parameters used in bioinformatics analyses. Retrospectively, it is highly probable that the phenomenon was indeed overlooked and mosaic variations have been missed in MFS probands. This has important consequences since these patients are now likely to be offered costly sequencing of their genome that, in fact, is not necessary. Finally, the five present cases of symptomatic patients with a mosaic FBN1 pathogenic variant underscores the need to perform complete clinical follow-up in apparently asymptomatic mosaic parents.
Data availability
The data are available upon request.
References
Loeys, B. L., Dietz, H. C. & Braverman, A. C. et al. The revised Ghent nosology for the Marfan syndrome. J. Med. Genet. 47, 476–485 (2010).
Collod-Béroud, G., Le Bourdelles, S. & Ades, L. et al. Update of the UMD-FBN1 mutation database and creation of an FBN1 polymorphism database. Hum. Mutat. 22, 199–208 (2003).
Biesecker, L. G. & Spinner, N. B. A genomic view of mosaicism and human disease. Nat. Rev. Genet. 14, 307–320 (2013).
Spinner, N. B. & Conlin, L. K. Mosaicism and clinical genetics. Am J. Med. Genet. C Semin. Med. Genet. 166C, 397–405 (2014).
García-Romero, M. T., Parkin, P. & Lara-Corrales, I. Mosaic neurofibromatosis type 1: a systematic review. Pediatr. Dermatol. 33, 9–17 (2016).
Biesecker, L. G. & Sapp, J. C. in GeneReviews (eds Adam, M. P., Ardinger, H. H. & Pagon, R. A. et al.). Proteus syndrome (University of Washington, Seattle, 1993). http://www.ncbi.nlm.nih.gov/books/NBK99495/
Lindhurst, M. J., Sapp, J. C. & Teer, J. K. et al. A mosaic activating mutation in AKT1 associated with the Proteus syndrome. N. Engl. J. Med. 365, 611–619 (2011).
Verstraeten, A., Alaerts, M., Van Laer, L. & Loeys, B. Marfan syndrome and related disorders: 25 years of gene discovery. Hum. Mutat. 37, 524–531 (2016).
Arnaud, P., Hanna, N. & Aubart, M. et al. Homozygous and compound heterozygous mutations in the FBN1 gene: unexpected findings in molecular diagnosis of Marfan syndrome. J. Med. Genet. 54, 100–103 (2017).
Collod-Béroud, G., Lackmy-Port-Lys, M. & Jondeau, G. et al. Demonstration of the recurrence of Marfan-like skeletal and cardiovascular manifestations due to germline mosaicism for an FBN1 mutation. Am. J. Hum. Genet. 65, 917–921 (1999).
Blyth, M., Foulds, N., Turner, C. & Bunyan, D. Severe Marfan syndrome due to FBN1 exon deletions. Am J. Med. Genet. A 146A, 1320–1324 (2008).
Rekondo, J., Robledo-Inarritu, M., Vado, Y., Pérez de Nanclares, G. & Arós, F. Marfan syndrome caused by somatic mosaicism in an FBN1 splicing mutation. Rev. Espanola Cardiol. Engl. Ed. 69, 520–521 (2016).
Arnaud, P., Hanna, N. & Benarroch, L. et al. Genetic diversity and pathogenic variants as possible predictors of severity in a French sample of nonsyndromic heritable thoracic aortic aneurysms and dissections (nshTAAD). Genet. Med. 21, 2015–2024 (2019).
Campens, L., Demulier, L. & De Groote, K. et al. Reference values for echocardiographic assessment of the diameter of the aortic root and ascending aorta spanning all age categories. Am. J. Cardiol. 114, 914–920 (2014).
den Dunnen, J. T., Dalgleish, R. & Maglott, D. R. et al. HGVS recommendations for the description of sequence variants: 2016 update. Hum. Mutat. 37, 564–569 (2016).
Salgado, D., Desvignes, J.-P. & Rai, G. et al. UMD-Predictor: a high-throughput sequencing compliant system for pathogenicity prediction of any human cDNA substitution. Hum. Mutat. 37, 439–446 (2016).
Adzhubei, I. A., Schmidt, S. & Peshkin, L. et al. A method and server for predicting damaging missense mutations. Nat. Methods 7, 248–249 (2010).
Montgomery, R. A., Geraghty, M. T. & Bull, E. et al. Multiple molecular mechanisms underlying subdiagnostic variants of Marfan syndrome. Am. J. Hum. Genet. 63, 1703–1711 (1998).
Rantamäki, T., Kaitila, I., Syvänen, A. C., Lukka, M. & Peltonen, L. Recurrence of Marfan syndrome as a result of parental germ-line mosaicism for an FBN1 mutation. Am. J. Hum. Genet. 64, 993–1001 (1999).
Tekin, M., Cengiz, F. B. & Ayberkin, E. et al. Familial neonatal Marfan syndrome due to parental mosaicism of a missense mutation in the FBN1 gene. Am J. Med. Genet. A 143A, 875–880 (2007).
Hilhorst-Hofstee, Y., Hamel, B. C. J. & Verheij, J. B. G. M. et al. The clinical spectrum of complete FBN1 allele deletions. Eur. J. Hum. Genet. 19, 247–252 (2011).
Sípek, A., Grodecká, L. & Baxová, A. et al. Novel FBN1 gene mutation and maternal germinal mosaicism as the cause of neonatal form of Marfan syndrome. Am J. Med. Genet. A 164A, 1559–1564 (2014).
Martínez-Quintana, E., Caballero-Sánchez, N., Rodríguez-González, F., Garay-Sánchez, P. & Tugores, A. Novel Marfan syndrome-associated mutation in the FBN1 gene caused by parental mosaicism and leading to abnormal limb patterning. Mol. Syndromol. 8, 148–154 (2017).
van Veghel-Plandsoen, M. M., Wouters, C. H., Kromosoeto, J. N. R., den Ridder-Klünnen, M. C., Halley, D. J. J. & van den Ouweland, A. M. W. Multiplex ligation-depending probe amplification is not suitable for detection of low-grade mosaicism. Eur. J. Hum. Genet. 19, 1009–1012 (2011).
Brewer, C. J., Gillespie, M. & Fierro, J. et al. The value of parental testing by next-generation sequencing includes the detection of germline mosaicism. J. Mol. Diagn. 22, 670–678 (2020).
Faivre, L., Collod-Beroud, G. & Loeys, B. L. et al. Effect of mutation type and location on clinical outcome in 1,013 probands with Marfan syndrome or related phenotypes and FBN1 mutations: an international study. Am. J. Hum. Genet. 81, 454–466 (2007).
Acknowledgements
Several authors of this publication are members of the European Reference Network for Rare Multisystemic Vascular Diseases (VASCERN) and French Rare Disease Network FAVA-Multi.
Author information
Authors and Affiliations
Contributions
Conceptualization: P.A., C.B., N.H. Data curation: P.A., H.M. Funding acquisition: C.L.G., G.J., C.B. Investigation: O.M., L.G., C.F., A.D.C., G.J. Methodology: P.A., C.L.G., C.B., N.H. Resources: C.B. Supervision: C.B., N.H. Writing—original draft: P.A., H.M., N.H. Writing—review and editing: P.A., N.H., C.B.
Corresponding authors
Ethics declarations
Ethics declaration
Informed consent was obtained for all patients in agreement with the requirements of French bioethics laws. Institutional review board [IRB] approval was obtained from Comité de Protection des Personnes number 11 008, 13 January 2011.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Arnaud, P., Morel, H., Milleron, O. et al. Unsuspected somatic mosaicism for FBN1 gene contributes to Marfan syndrome. Genet Med 23, 865–871 (2021). https://doi.org/10.1038/s41436-020-01078-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-020-01078-6
This article is cited by
-
Identification of two variants in PAX3 and FBN1 in a Chinese family with Waardenburg and Marfan syndrome via whole exome sequencing
Functional & Integrative Genomics (2023)
-
Marfan syndrome
Nature Reviews Disease Primers (2021)