Abstract
Purpose
Previous studies have reported that prenatal exome sequencing (pES) can detect monogenic diseases in fetuses with congenital anomalies with diagnostic yields ranging from 6% to 81%, but there are few reports of its clinical utility.
Methods
We conducted a retrospective chart review of patients who had pES to determine whether results led to clinical management changes.
Results
Of 20 patients, 8 (40%) received a definitive diagnosis. Seven patients (35%) had medical management changes based on the pES results, including alterations to their delivery plan and neonatal management (such as use of targeted medications, subspecialty referrals, additional imaging and/or procedures). All patients who received a definitive diagnosis and one who received a likely pathogenic variant (n = 9; 45%) received specific counseling about recurrence risk and the medical/developmental prognosis for the baby. In five (25%) cases, the result facilitated a diagnosis in parents and/or siblings.
Conclusion
pES results can have significant impacts on clinical management, some of which would not be possible if testing is deferred until after birth. To maximize the clinical utility, pES should be prioritized in cases where multiple care options are available and the imaging findings alone are not sufficient to guide parental decision-making, or where postnatal testing will not be feasible.
Similar content being viewed by others
INTRODUCTION
Congenital anomalies and genetic conditions are noted in approximately 2–5% of pregnancies and are major causes of fetal demise and infant death.1,2 Chromosomal microarray is recommended to evaluate for chromosomal abnormalities in fetuses with congenital anomalies, but 60–70% of fetuses remain without a genetic diagnosis after microarray, which can complicate counseling, prenatal management, and parental decision-making.3,4
With the decreasing cost and turnaround time (TAT) of genomic testing methodologies, broad testing approaches such as exome sequencing (ES) are being used more frequently for prenatal diagnosis of monogenic disorders not detectable by microarray. Current professional society opinions support the use of prenatal ES (pES) in select cases of anomalies suggestive of a genetic disorder with the input of a clinical geneticist.3,5,6 Prior case series have reported highly variable diagnostic yields of pES from 6.2% to 89%, with most reporting yields of 20–40%.7,8,9,10,11,12,13,14,15,16,17,18,19,20
However, it remains to be determined whether this improved diagnostic yield is meaningful to the patient and family. The American College of Medical Genetics and Genomics defines the clinical utility of genetic testing as its “effects on diagnostic or therapeutic management, implications for prognosis, health and psychological benefits to patients and their relatives, and economic impact on health-care systems.”21 Most genetics providers believe that pES will have clinical utility.22,23,24,25 Previous studies of pES indicate that results can impact decision-making about continuation or termination, pre- or postnatal medical management, delivery planning, recurrence risk counseling, reproductive planning, and parental medical management.8,9,10,13,18,20,26
However, there are also risks and limitations of pES that must be considered. Since parents may choose to terminate their pregnancy based on the results, there is a potential for harm if results are ambiguous, unexpected, and/or misunderstood.25,27 As in postnatal ES, there is a risk of discovering incidental or secondary findings. The interpretation of variants detected on pES can be also challenging because the prenatal-onset phenotypes of many disorders are poorly characterized and the phenotype information about a fetus is often limited.19 Additionally, pES requires a rapid TAT if results are to be used for clinical management, which can be labor-intensive for both the clinical and laboratory teams. The cost of pES may pose a significant burden to patients because most US health-care insurance providers do not cover the cost of this test, citing a lack of evidence to support its clinical utility.28
Given the potential limitations, additional studies are needed to establish the clinical utility of pES to justify its use. Here, we examine the clinical utility of pES in a cohort of 20 patients seen at our institution for pregnancies affected by congenital anomalies.
MATERIALS AND METHODS
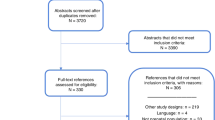
A retrospective chart review was conducted for patients evaluated in our fetal care center who had ES ordered during pregnancy or after a fetal demise or termination of pregnancy (TOP), which were all considered as pES for this study since the indications for testing were prenatally identified congenital anomalies. Our fetal care center is a tertiary referral center that evaluated approximately 1,100 patients from 2018 to 2019 (the timeframe where most of the patients included in this chart review were evaluated) for congenital anomalies and complications of multiple gestations. All patients underwent detailed prenatal phenotyping via ultrasound, fetal magnetic resonance imaging (MRI), and fetal echocardiogram, as well as evaluation by a multidisciplinary team including a clinical geneticist, genetic counselor, maternal fetal medicine specialist, neonatologist, and additional subspecialists as needed based on the fetal anomalies (e.g., fetal/pediatric surgeon, neurologist). Patients were considered eligible for pES if their fetus had congenital anomalies thought to be caused by an underlying genetic disorder but for which multigene panels were not felt to be suitable as determined by the clinical geneticist and genetic counselor. All patients underwent chromosomal microarray testing prior to or concurrently with pES. Some patients had additional testing, such as amniotic fluid viral studies, based on their indications. There were no gestational age restrictions for eligibility. Patients considering TOP, a comfort care approach, or full medical interventions were all eligible. Patients were eligible for this chart review if pES produced a result (i.e., no sample failure) and they were no longer pregnant at the time of chart review.
Fetal DNA was obtained via chorionic villus sampling, amniocentesis, or fetal tissue. Blood or saliva was collected from parents for duo or trio analysis. All patients received counseling about pES from a certified genetic counselor and provided written informed consent for the testing. ES was performed by CLIA-approved commercial or academic laboratories selected on a case-by-case basis based on patient-specific factors, such as gestational age, insurance considerations, and eligibility for a pES clinical trial. Variant interpretation and reporting were performed by individual laboratories per standard clinical practice.
Maternal and neonatal charts were reviewed to describe the prenatal phenotype, pregnancy and neonatal outcomes (when applicable), pES results, and clinical utility of the results. Clinical utility was defined as changes to prenatal management (e.g., decisions about prenatal surgical interventions, decision about pregnancy termination or perinatal palliative care), delivery management (e.g., change in location, mode, and/or timing of delivery), neonatal management (e.g., initiation of gene- or pathway-specific medication, subspecialist referrals), family planning (e.g., specific recurrence risk counseling, pursuit of preimplantation or prenatal genetic testing for future pregnancies), family medical care (e.g., diagnosis of a genetic disorder in parents and/or siblings), and other aspects of care (e.g., psychosocial interventions).
RESULTS
Cohort demographics
Twenty patients from March 2015 to October 2019 were identified who met the inclusion criteria (Table 1). One additional patient was excluded since exome was ordered based on the autopsy findings and was therefore not considered a prenatal exome. Most had pES in 2018 (n = 9) or 2019 (n = 9). Nineteen were completed as trios and one was a maternal/fetal duo as the father was unavailable.
Fourteen (70%) were ordered during an ongoing pregnancy, 3 (15%) after fetal demise, and 3 (15%) after TOP. The average gestational age for the pES order during an ongoing pregnancy was 28 4/7 weeks gestation. For the eight patients who received results during their pregnancy, the average TAT was 19.3 days and the average gestational age at the time of the result was 30 5/7 weeks. For the remaining 12 patients, the average TAT was 56.8 days.
pES results
Eight patients (40%) received a diagnostic result from pES (Table 1). Of these diagnoses, three (cases 1, 3, and 6) were autosomal recessive disorders and one (case 8) was an autosomal dominant disorder inherited from a previously undiagnosed mother. The remaining four were de novo autosomal dominant (cases 4, 5, and 7) and somatic mosaic (case 2) disorders. Seven additional patients (35%) received an inconclusive result due to variants of uncertain clinical significance. In two cases (cases 1 and 16), variants in novel genes were reported. Of the five patients who received negative pES results, two received postnatal diagnoses of nongenetic disorders (cases 16 and 18).
Clinical utility of pES results
Nine patients (45%) had clinical management changes made based on the pES result, including all eight who received a diagnosis and one who received an inconclusive result (Table 2).
Case 1
Multiple brain malformations, hydrops, small chest, hepatomegaly, decreased muscle mass, small kidneys, and oligohydramnios detected by ultrasound at 20 5/7 weeks gestation
pES detected compound heterozygous likely pathogenic variants in NMNAT2, a novel gene with no established human phenotype. The parents had previously decided on palliative care based on the poor prognosis associated with the imaging findings (Fig. 1a). Phenotypes reported in animal studies of NMNAT2 were consistent with the fetal anomalies. The clinical team believed this was likely the diagnosis for the fetus, which facilitated counseling about a recurrence risk of 25% and prompted the parents to pursue preimplantation genetic testing (PGT) resulting in a healthy child. They later had another pregnancy affected by similar anomalies and underwent targeted prenatal diagnostic testing that confirmed the same NMNAT2 variants in this fetus. Functional studies established that these variants impair NMNAT2 function and supported this gene’s association with fetal akinesia deformation sequence.29
(a) Case 1 at 26 3/7: severe hydrops fetalis, severe ventriculomegaly, abnormal brainstem morphology, cerebellar hypoplasia, and hepatomegaly. (b) Case 2 at 27 2/7: megalencephaly, frontal bossing, and thickened soft tissues of the chin. (c) Case 4 at 24 3/7: severely hypoplastic nose and micrognathia. (d) Case 6 at 24 4/7: significant scoliosis and slender limbs with deficient muscle mass. (e) Case 7 at 25 0/7: micrognathia, flattened facial profile, small and bell-shaped chest, pulmonary hypoplasia, shortened limbs, and generalized edema. (f) Case 9 at 30 4/7: severe micrognathia, small chest, and polyhydramnios.
Case 2
Megalencephaly, neuronal migration anomalies, enlarged globes, thickened chin soft tissue, and ambiguous genitalia detected by ultrasound at 23 2/7 weeks gestation
pES detected a pathogenic variant in AKT1 consistent with a diagnosis of Proteus syndrome (OMIM 176920). Based on the grave prognosis of Proteus syndrome in the context of the fetal anomalies (Fig. 1b), the parents enrolled in perinatal palliative care. At 35 weeks gestation, the fetal head circumference was greater than 2 standard deviations above the mean. Due to concerns that continued overgrowth of the head was likely and could result in maternal morbidity during delivery, her delivery timing was changed from 37 to 35 weeks gestation to reduce the risk of maternal morbidity and she delivered by an uncomplicated cesarean section with a low-transverse incision. After birth, the baby received a full-body MRI to screen for additional Proteus syndrome–related overgrowth. Her known diagnosis and enrollment in palliative care allowed her medical team to minimize the duration of her hospital stay and she was discharged at 10 days of life. She later developed seizures requiring polypharmacy, including the mTOR inhibitor sirolimus to target the AKT1 biochemical pathway. Unfortunately, she died of respiratory failure at 6 months. The parents were counseled about the negligible recurrence risk for future pregnancies due to the sporadic nature of Proteus syndrome. The parents reported psychosocial utility of the result as it facilitated their connection to Proteus syndrome support groups.
Case 3
Arthrogryposis and hydrops detected by ultrasound at 25 2/7 weeks gestation
Since the parents had a previous female child with arthrogryposis who died as a neonate and remained undiagnosed after a multigene panel for fetal akinesia, pES was felt to be the best test to identify a diagnosis in this fetus. The patient delivered shortly after pES was ordered and the baby died prior to the availability of results. pES detected compound heterozygous pathogenic variants in SCN4A associated with congenital myopathy, which confirmed the 25% recurrence risk and a diagnosis for their previous child. To our knowledge, the parents are investigating options for PGT to prevent further recurrence.
Case 4
Hypoplastic nose, micrognathia, hypogenesis of the corpus callosum, and pelvocaliectasis detected by ultrasound at 18 0/7 weeks gestation, with cystic hygroma detected at 11 3/7 weeks gestation
pES was recommended to guide the parental decision-making about neonatal management options due to the wide range outcomes associated with the fetal anomalies (Fig. 1c) and detected a de novo pathogenic variant in KANSL1 consistent with a diagnosis of Koolen–de Vries syndrome (KdVS; OMIM 610443). The parents opted for full intervention after receiving the genetic diagnosis. After birth, the baby received a screening electroencephalogram (EEG) and early placement of a gastrostomy tube due to the known risks for seizures and feeding problems associated with KdVS. He developed worsening respiratory distress and received a tracheostomy at 6 weeks of life. His postnatal X-rays demonstrated epiphyseal stippling in addition to his severely hypoplastic nose, consistent with chondrodysplasia punctata (CDP). His ES data were reanalyzed and a multigene deletion/duplication panel was ordered, but neither identified a genetic etiology for CDP. It remains unknown whether CDP represents an unrecognized phenotype of KdVS or if there is another etiology for this phenotype.
Case 5
Microphthalmia, micrognathia, pectus excavatum, horseshoe kidney, hypoplastic left heart syndrome, and polyhydramnios detected by ultrasound at 21 1/7 weeks gestation
pES was recommended to guide parental decision-making about whether to pursue neonatal surgical intervention for hypoplastic left heart syndrome in the context of multiple congenital anomalies, but the results were not available until 18 days after birth due to difficulties obtaining a maternal DNA sample. The mother had opted for full neonatal intervention prior to receiving the pES results of a presumed de novo pathogenic variant in KMT2D consistent with a diagnosis of Kabuki syndrome (OMIM 147920). Due to the risk for immunodeficiency associated with Kabuki syndrome, an immunology evaluation was performed at 3 weeks of life which demonstrated lymphopenia. At 18 months, he developed hypogammaglobulinemia requiring intravenous immunoglobulin. The diagnosis improved counseling about the long-term medical and developmental prognosis for this baby to inform future medical management decisions, as well as counseling about the likely low recurrence risk due to the presumed de novo nature of the variant.
Case 6
Arthrogryposis, deficient muscle mass, scoliosis, micrognathia, frontal bossing, soft tissue edema, ventricular septal defect, and polyhydramnios detected by ultrasound at 20 0/7 weeks gestation
Due to the anomalies visualized with prenatal imaging (Fig. 1d), the parents were counseled that their baby would likely need an ex utero intrapartum therapy (EXIT) delivery and a prolonged hospital. Therefore, pES was recommended to guide parental decision-making. pES detected compound heterozygous pathogenic variants in NEB consistent with nemaline myopathy 2 (OMIM 256030). After receiving the pES results, the prenatal care team recommended against performing an EXIT delivery due to the poor long-term prognosis of this condition and the increased risk of maternal complications associated with EXIT delivery. Instead, the care team and mother elected for a C-section delivery with attempt to intubate the infant while still on placental support. They also referred the parents to a perinatal palliative care team. Given the likely respiratory distress and lifelong need for mechanical ventilation, the parents requested intubation and a trial of mechanical ventilation after delivery but declined chest compressions and tracheostomy placement. The delivery and intubation were successful, and the baby ultimately remained ventilator dependent. His parents took time for valuable psychosocial interventions including memory-making activities and baptism prior to removal of his breathing tube. The diagnosis also allowed for counseling about the 25% recurrence risk.
Case 7
Short limbs, micrognathia, bell-shaped chest, edema, and hypoplastic left heart syndrome detected by ultrasound at 16 2/7 weeks gestation
The imaging findings of a complex heart defect and suspected pulmonary hypoplasia due to a bell-shaped chest (Fig. 1e) suggested a poor prognosis, so the parents sought a genetic diagnosis to inform their prenatal and neonatal decision-making. pES detected a de novo pathogenic variant in COL2A1 associated with skeletal dysplasia. While COL2A1 is known to be associated with multiple types of skeletal dysplasia, it had not been previously associated with heart defects. Therefore, it is uncertain whether this case expands the phenotype of COL2A1-related skeletal dysplasia or if the heart defect had a separate etiology. The prenatal genetic diagnosis supported the decision to pursue palliative care and facilitated counseling about the low recurrence risk for the skeletal dysplasia due to the de novo nature of the variant. pES also identified two variants in PIEZO1, a gene associated with autosomal dominant iron overload, splenomegaly, and gallstones (OMIM 194380), and autosomal recessive lymphedema (OMIM 616843). The father reported a personal history of splenomegaly and a family history of gallstones, so he was counseled that he likely has the autosomal dominant PIEZO1-related disorder, which has a 50% recurrence risk.
Case 8
Hydrops, short nasal bone, mild ventriculomegaly, and pelvocaliectasis detected by ultrasound at 18 4/7 weeks gestation, with cystic hygroma detected at 13 4/7 weeks gestation
pES performed after fetal demise identified a maternally inherited pathogenic variant in PTPN11 consistent with Noonan syndrome (OMIM 163950). The mother was referred to a RASopathy-specific genetics clinic where she was noted to have short stature, mitral valve regurgitation, and a bleeding tendency including easy bruising, heavy periods, gum bleeding, and significant bleeding after a previous surgery. It was recommended that her care include continued follow-up with this clinic, regular echocardiograms due to the increased risk of hypertrophic cardiomyopathy, and hematology screening for platelet anomalies. The diagnosis also facilitated accurate counseling of a 50% recurrence risk and the parents have expressed an interest in PGT.
Case 9
Severe micrognathia, midface hypoplasia, short ribs, pulmonary hypoplasia, and polyhydramnios detected by ultrasound at 24 5/7 weeks gestation, with cystic hygroma detected at 13 weeks gestation
pES was recommended to guide delivery planning as the severe fetal micrognathia (Fig. 1f) would likely necessitate an EXIT delivery to establish an airway, increasing the risk of maternal morbidity. The patient declined amniocentesis solely for genetic testing, so pES was sent at 36 weeks gestation when she required an amnioreduction due to polyhydramnios. The results were not available for delivery planning and she delivered by EXIT-to-tracheostomy due to severe fetal micrognathia (jaw index measured less than 5th percentile at 34 weeks gestation) and glossoptosis. She continues to be dependent on mechanical ventilation by tracheostomy at 2 years of life. pES results were reported 17 days after delivery and did not identify a conclusive primary diagnosis. However, it identified a paternally inherited likely pathogenic variant in ALPL thought to be consistent with a later-onset autosomal dominant form of hypophosphatasia (HPP; OMIM 146300). The baby had very poor bone mineralization, low alkaline phosphatase activity, and elevated vitamin B6, so she was treated with asfotase alfa, an HPP-targeted medication. This result also led to a paternal diagnosis of HPP and informed counseling about a 50% recurrence risk for HPP.
DISCUSSION
In our cohort, 40% of patients with severe and/or multiple fetal anomalies received a diagnosis from pES, which is comparable to the diagnostic yields previously reported for fetuses with similar presentations. In fetuses with multiple anomalies and/or suspected Mendelian disorders, the incremental diagnostic yield of pES over microarray is at least comparable to, if not better than, the 5–10% incremental diagnostic yield of microarray over karyotype. Thus, the value of pES in diagnosing genetic conditions should no longer be questioned. However, the clinical utility of pES still needs to be established.
In our cohort, pES led to clinical management changes in 45% of patients, most often related to family planning (45%) and neonatal medical management (25%), as well as diagnoses in family members (25%). Previously, two studies from the Netherlands reported that clinical management was directly impacted by pES results in 70% of their patients, where results were used to make decisions about pregnancy termination and pre- and postnatal medical management.10,26 Notably, half of the patients in these studies with negative results had clinical management changes, primarily related to supporting their decision to continue their pregnancy and/or pursue intervention for the fetal anomalies, which further underscores the difference between diagnostic yield and clinical utility.
Surveys of clinicians and parents have reported that most believe that pES will have clinical utility related to diagnosing genetic conditions, impacting pregnancy management, facilitating decisions about pregnancy termination, preparing for childhood-onset conditions, and informing reproductive planning.22,24,30,31,32,33 In stark contrast, a study of 14 US health-care insurance payers reported that none believed that decisions about TOP, withdrawal of intensive care, provision of palliative care, family planning, or directing families to disease-specific resources (e.g., support groups, research) were aspects of clinical utility of pES, and only a minority agreed that referral to a tertiary center for specialized care was an aspect of clinical utility.28 Therefore, it will be challenging to reconcile the different perspectives of the various pES stakeholders to establish its clinical utility.
One argument against pES is that, given the availability of rapid postnatal ES, pES adds no value until in utero interventions for fetal genetic disorders are clinically available. However, the fetus is not the sole patient of concern in the prenatal period; the mother should also be considered since results can directly impact her health, as demonstrated by cases 2 and 6 where the genetic diagnosis led to modifications of the delivery plans to reduce maternal morbidity. These decisions would not have been possible if testing had been deferred to the postnatal period. Thus, it is imperative to consider maternal health outcomes as part of the clinical utility of pES.
The claim that rapid neonatal ES obviates the need for pES also overlooks the importance of perinatal medical management decisions for the baby, such as planning for optimal delivery room resuscitation and timely initiation of diagnosis-specific treatment. Kingsmore et al. recently reviewed studies of rapid ES and reported median TAT ranging from 9 to 23 days.34 Given that some genetic conditions have targeted therapies available, such as cases 2 and 9 as well as 27% of Kingsmore’s cohort, treatment could be delayed for days to weeks while awaiting rapid neonatal results. As intensive neonatal care and targeted therapies are not available at all hospitals, prenatal genetic diagnosis can facilitate referrals to institutions that are able to provide the appropriate therapies without delay. A prenatal genetic diagnosis may also limit expensive or invasive diagnostic testing that may be performed while postnatal testing is pending.
Furthermore, the notion that in utero or neonatal treatments are the only clinically useful interventions ignores the value of perinatal palliative care, which empowers parents to consider their values and hopes for their child’s quality of life while ensuring that their physical and psychosocial needs are met. With earlier referrals to palliative care services, families form stronger bonds with their health-care team and have a healthier grieving process.35,36 While families may choose to redirect to a palliative care approach after learning of a life-limiting diagnosis in their newborn, deciding to withdraw care that has already begun is often more difficult for families than avoiding invasive and painful care in the first place.37 Indeed, the diagnoses in cases 2 and 6 facilitated prenatal enrollment in a perinatal palliative care program, allowing these families to request avoidance of futile, painful procedures such as chest compressions; decrease the baby’s inpatient hospital stay to maximize family bonding at home; and plan meaningful rituals, such as baptism and memory-making, prior to the baby’s death. Therefore, while it is not always possible to improve a baby’s long-term outcome, prenatal diagnosis can improve the baby’s quality of life and the overall experience of the family.
Another significant difference between pre- and postnatal genetic testing is that TOP may be considered during an ongoing pregnancy, but prenatal imaging findings may not be sufficient to guide this decision without knowledge of the underlying etiology. For example, parents of a baby with an isolated heart defect detected on ultrasound are more likely to terminate their pregnancy if an underlying genetic condition is identified.38 As this decision is restricted to the prenatal period, access to prenatal genetic testing including pES is imperative for parents to make informed decisions about their pregnancy.
Certainly, there are important limitations of pES that must be considered. Due to the broad nature of the testing, there is the possibility of receiving variants of uncertain clinical significance, as seen in 35% of our cohort. Since parents may make irreversible decisions, such as pursuing pregnancy termination or declining intensive interventions, it is imperative that uncertain results are fully explained in both pre- and post-test counseling to limit the risk of harm. Additionally, since there is an inherent timeframe in which prenatal and delivery management decisions can be made, the TAT for pES results needs to be optimized.
In our cohort, the decision to perform pES was at the discretion of the multidisciplinary clinical team that included a clinical geneticist and was based on a high suspicion of a Mendelian genetic disorder. As a result, the diagnostic yield and rate at which clinical management changes occurred in our study are likely higher than cohorts of all prenatally diagnosed congenital anomalies. However, the data presented here may be representative of yields expected in actual clinical practice. Additionally, our cohort represents the patients with health insurance carriers who approved pES, personal financial resources to pay for the testing, or who qualified for free testing by other means, and thus excludes patients who lacked the financial ability to access this testing.
The retrospective nature of our study limited identification of clinical management changes to those explicitly documented in the patients’ medical records. While we made every effort possible to only report clinical management changes that specifically resulted from the pES results, including speaking with the clinical staff when the patients’ charts were unclear, it is possible that some decisions may have been influenced by other factors (e.g., progression of imaging findings). We did not identify any cases where clinical management changes were made based on the lack of a genetic diagnosis from an inconclusive or negative result, which may be in part because pregnancy termination is not common in our clinic’s population. Additionally, for our patients who had pES during an ongoing pregnancy, it was ordered in the late second to late third trimesters; we therefore cannot comment on the clinical utility of pES results in the first or early second trimesters. Future prospective studies should be performed to better evaluate and maximize the impact of positive, inconclusive, and negative pES results on clinical decision-making throughout pregnancy.
In conclusion, results from pES can have significant impacts on the clinical management of the mother, neonate, and other family members, such as reducing risks of maternal morbidity during delivery, planning for optimal neonatal resuscitation, early initiation of diagnosis-targeted treatments, avoiding futile neonatal interventions, diagnosing other family members, and facilitating informed reproductive decision-making. As some of these decisions are only possible in the prenatal period, deferring genetic testing to the postnatal period is not always ideal. In cases where a genetic etiology is suspected and parents are pursuing TOP or where intrauterine fetal demise is likely, pES may be the only feasible opportunity to establish a genetic diagnosis to guide future reproductive planning. Additionally, pES may have clinical utility in cases where multiple care options are available, such as intensive in utero or neonatal intervention, TOP, and palliative care, but where the imaging findings alone are not sufficient to guide parental decision-making.
Data availability
The authors are willing to share additional details about the data included in this publication in accordance with HIPAA and institutional review board (IRB) regulations. The corresponding author can be contacted with requests for additional information.
References
Carmichael, S. L. Birth defects epidemiology. Eur. J. Med. Genet. 57, 355–358 (2014).
Wojcik, M. H. et al. Infant mortality: the contribution of genetic disorders. J. Perinatol. 39, 1611–1619 (2019).
ACOG. Committee opinion no. 682: microarrays and next-generation sequencing technology. The use of advanced genetic diagnostic tools in obstetrics and gynecology. Obstet. Gynecol. 128, e262–e268 (2016).
Wapner, R. J. et al. Chromosomal microarray versus karyotyping for prenatal diagnosis. N. Engl. J. Med. 367, 2175–2184 (2012).
ISPD. Joint position statement from the International Society for Prenatal Diagnosis (ISPD), the Society for Maternal Fetal Medicine (SMFM), and the Perinatal Quality Foundation (PQF) on the use of genome-wide sequencing for fetal diagnosis. Prenat. Diagn. 38, 6–9 (2018).
Monaghan, K. G., Leach, N. T., Pekarek, D., Prasad, P. & Rose, N. C. The use of fetal exome sequencing in prenatal diagnosis: a points to consider document of the American College of Medical Genetics and Genomics (ACMG). Genet. Med. 22, 675–680 (2020).
Boissel, S. et al. Genomic study of severe fetal anomalies and discovery of GREB1L mutations in renal agenesis. Genet. Med. 20, 745–753 (2018).
Chandler, N. et al. Rapid prenatal diagnosis using targeted exome sequencing: a cohort study to assess feasibility and potential impact on prenatal counseling and pregnancy management. Genet. Med. 20, 1430–1437 (2018).
Daum, H., Meiner, V., Elpeleg, O. & Harel, T. Fetal exome sequencing: yield and limitations in a tertiary referral center. Ultrasound Obstet. Gynecol. 53, 80–86 (2019).
de Koning, M. A. et al. From diagnostic yield to clinical impact: a pilot study on the implementation of prenatal exome sequencing in routine care. Genet. Med. 21, 2303–2310 (2019).
Fu, F. et al. Whole exome sequencing as a diagnostic adjunct to clinical testing in fetuses with structural abnormalities. Ultrasound Obstet. Gynecol. 51, 493–502 (2018).
Lord, J. et al. Prenatal exome sequencing analysis in fetal structural anomalies detected by ultrasonography (PAGE): a cohort study. Lancet. 393, 747–757 (2019).
Normand, E. A. et al. Clinical exome sequencing for fetuses with ultrasound abnormalities and a suspected Mendelian disorder. Genome Med. 10, 74 (2018).
Petrovski, S. et al. Whole-exome sequencing in the evaluation of fetal structural anomalies: a prospective cohort study. Lancet. 393, 758–767 (2019).
Vora, N. L. et al. Prenatal exome sequencing in anomalous fetuses: new opportunities and challenges. Genet. Med. 19, 1207–1216 (2017).
Westerfield, L. E. et al. Reproductive genetic counseling challenges associated with diagnostic exome sequencing in a large academic private reproductive genetic counseling practice. Prenat. Diagn. 35, 1022–1029 (2015).
Yadava, S. M. & Ashkinadze, E. Whole exome sequencing for prenatal diagnosis in cases with fetal anomalies: criteria to improve diagnostic yield. J. Genet. Couns. 28, 251–255 (2019).
Vora, N. L. et al. An approach to integrating exome sequencing for fetal structural anomalies into clinical practice. Genet. Med. 22, 954–961 (2020).
Aggarwal, S. et al. Exome sequencing for perinatal phenotypes: the significance of deep phenotyping. Prenat. Diagn. 40, 260–273 (2020).
Han, J. et al. Rapid prenatal diagnosis of skeletal dysplasia using medical trio exome sequencing: benefit for prenatal counseling and pregnancy management. Prenat. Diagn. 40, 577–584 (2020).
ACMG. Clinical utility of genetic and genomic services: a position statement of the American College of Medical Genetics and Genomics. Genet. Med. 17, 505–507 (2015).
Best, S., Wou, K., Vora, N., Van der Veyver, I. B., Wapner, R. & Chitty, L. S. Promises, pitfalls and practicalities of prenatal whole exome sequencing. Prenat. Diagn. 38, 10–19 (2018).
Mone, F., Quinlan-Jones, E. & Kilby, M. D. Clinical utility of exome sequencing in the prenatal diagnosis of congenital anomalies: a review. Eur. J. Obstet. Gynecol. Reprod. Biol. 231, 19–24 (2018).
Narayanan, S., Blumberg, B., Clayman, M. L., Pan, V. & Wicklund, C. Exploring the issues surrounding clinical exome sequencing in the prenatal setting. J. Genet. Couns. 27, 1228–1237 (2018).
Brew, C. E., Castro, B. A., Pan, V., Hart, A., Blumberg, B. & Wicklund, C. Genetics professionals’ attitudes toward prenatal exome sequencing. J. Genet. Couns. 28, 229–239 (2019).
Deden, C. et al. Rapid whole exome sequencing in pregnancies to identify the underlying genetic cause in fetuses with congenital anomalies detected by ultrasound imaging. Prenat. Diagn. 40, 972–983 (2020).
Vora, N. L. & Hui, L. Next-generation sequencing and prenatal ‘omics: advanced diagnostics and new insights into human development. Genet. Med. 20, 791–799 (2018).
Trosman, J. R., Weldon, C. B., Slavotinek, A., Norton, M. E., Douglas, M. P. & Phillips, K. A. Perspectives of US private payers on insurance coverage for pediatric and prenatal exome sequencing: results of a study from the Program in Prenatal and Pediatric Genomic Sequencing (P3EGS). Genet. Med. 22, 283–291 (2020).
Lukacs, M. et al. Severe biallelic loss-of-function mutations in nicotinamide mononucleotide adenylyltransferase 2 (NMNAT2) in two fetuses with fetal akinesia deformation sequence. Exp. Neurol. 320, 112961 (2019).
Quinlan-Jones, E. et al. Prenatal whole exome sequencing: the views of clinicians, scientists, genetic counsellors and patient representatives. Prenat. Diagn. 36, 935–941 (2016).
Quinlan-Jones, E., Hillman, S. C., Kilby, M. D. & Greenfield, S. M. Parental experiences of prenatal whole exome sequencing (WES) in cases of ultrasound diagnosed fetal structural anomaly. Prenat. Diagn. 37, 1225–1231 (2017).
Kalynchuk, E. J., Althouse, A., Parker, L. S., Saller, D. N. Jr. & Rajkovic, A. Prenatal whole-exome sequencing: parental attitudes. Prenat. Diagn. 35, 1030–1036 (2015).
Wou, K. et al. Parental perceptions of prenatal whole exome sequencing (PPPWES) study. Prenat. Diagn. 38, 801–811 (2018).
Kingsmore, S. F. et al. A randomized, controlled trial of the analytic and diagnostic performance of singleton and trio, rapid genome and exome sequencing in ill infants. Am. J. Hum. Genet. 105, 719–733 (2019).
Rocha Catania, T. et al. When one knows a fetus is expected to die: palliative care in the context of prenatal diagnosis of fetal malformations. J. Palliat. Med. 20, 1020–1031 (2017).
Williams, C., Munson, D., Zupancic, J. & Kirpalani, H. Supporting bereaved parents: practical steps in providing compassionate perinatal and neonatal end-of-life care. A North American perspective. Semin. Fetal Neonatal Med. 13, 335–340 (2008).
Kamrath, H. J., Osterholm, E., Stover-Haney, R., George, T., O’Connor-Von, S. & Needle, J. Lasting legacy: maternal perspectives of perinatal palliative care. J. Palliat. Med. 22, 310–315 (2019).
van Nisselrooij, A. E. L. et al. The prevalence of genetic diagnoses in fetuses with severe congenital heart defects. Genet. Med. 22, 1206–1214 (2020).
Acknowledgements
D.T.S. was supported by National Institutes of Health (NIH) 5K08HL130666.
Author information
Authors and Affiliations
Contributions
Conceptualization: L.K.T., P.H., B.W., D.T.S. Data curation: L.K.T. Investigation: L.K.T. Methodology: L.K.T., P.H., B.W., D.T.S. Project administration: L.K.T. Visualization: L.K.T., P.H., B.W., D.T.S. Writing—original draft: L.K.T. Writing—review & editing: L.K.T., P.H., B.W., D.T.S.
Corresponding author
Ethics declarations
Ethics Declaration
This study was reviewed by the IRB at Cincinnati Children’s Hospital. It was deemed to be exempt from ongoing IRB oversight and granted a waiver of informed consent. All clinical data contained in this report has been de-identified.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tolusso, L.K., Hazelton, P., Wong, B. et al. Beyond diagnostic yield: prenatal exome sequencing results in maternal, neonatal, and familial clinical management changes. Genet Med 23, 909–917 (2021). https://doi.org/10.1038/s41436-020-01067-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-020-01067-9