Abstract
Purpose
Pharmacogenomic biomarkers are increasingly listed on medication labels and authoritative guidelines but pharmacogenomic-guided prescribing is not yet common. Our objective was to assess the potential for incorporating knowledge of patients’ genomic characteristics into prescribing practices.
Methods
We performed a retrospective analysis of claims data for 2,096,971 beneficiaries with pharmacy coverage from a national, commercial health insurance plan between January 2017 and December 2019. Children between 0 and 17 years comprised 21% of the cohort. Adults were age 18 to 64. Medications with actionable pharmacogenomic biomarkers (MAPBs) were identified using public information from the US Food and Drug Administration (FDA), Clinical Pharmacogenomics Implementation Consortium (CPIC), and PharmGKB.
Results
MAPBs were dispensed to 63% of the adults and 29% of the children in the cohort. Most frequently dispensed were ibuprofen, ondansetron, codeine, and oxycodone. Most common were medications with CYP2D6, G6PD, or CYPC19 pharmacogenomic biomarkers. Ten percent of the cohort were codispensed more than one MAPB for at least 30 days.
Conclusion
The number of people who might benefit from pharmacogenomic-guided prescribing is substantial. Future work should address obstacles to integrating genomic data into prescriber workflows, complex factors contributing to the magnitude of benefit, and the clinical availability of reliable on-demand or pre-emptive pharmacogenomic testing.
Similar content being viewed by others
INTRODUCTION
The lowest hanging fruit for introducing genomics into routine care may be use of a patient’s pharmacogenomic variants to influence prescribing.1 Genetic variants are linked to interindividual differences in efficacy and toxicity of many medications and are involved in drug metabolism, drug transport, and target binding. Hundreds of genes affecting medication metabolism have been reported and availability of genomic data is leading to discovery of new interactions. Actionable pharmacogenomic biomarkers are increasingly listed on US Food and Drug Administration (FDA) labels, and the Clinical Pharmacogenomics Implementation Consortium (CPIC) has published 25 peer-reviewed consensus guidelines for pharmacogenomic-guided therapy. We characterize use of medications with an actionable pharmacogenomic biomarker (MAPB) among beneficiaries from a national scale, privately insured health plan, and estimate the opportunity for pharmacogenomic-guided prescribing.
MATERIALS AND METHODS
Subjects
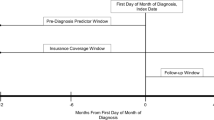
Claims data from a national commercial health insurance plan were used to select beneficiaries with continuous pharmacy coverage from 1 January 2017 to 31 December 2019. Individuals 0 to 64 years old were included even if they had no pharmacy claims (14.5%) but were known to have pharmacy coverage. The final cohort (n = 2,096,971) included 1,067,875 females (50.9%), 1,029,065 males (49.1%), and 31 with sex unknown. Children (n = 439,828, 21%) were defined as those who remained 0 to 17 years old throughout the study period. Adults were similarly defined as age 18 to 64 years. Individuals who would change age groups during the study were excluded.
Boston Children’s Hospital Institutional Review Board approved waiving consent. Risks were determined to be minimal with no potential for direct benefit. Aetna gave approval for the manuscript submission, confirming that no beneficiaries were identifiable.
Medications with an actionable pharmacogenomic biomarkers
Actionability was defined for medications with recommended variant-based dose modification, drug choice modification, frequency modification, increased therapeutic drug monitoring recommendations, or enhanced screening for adverse reactions. This is in keeping with a CPIC description of actionable variants as those that would alter standard prescribing practices if the data were present.2 Our initial search list was compiled from three publicly available sources: CPIC, FDA, and the Pharmacogenomics Knowledgebase (PharmGKB).3 Drugs included were listed on the FDA Table of Pharmacogenetic Associations (https://www.fda.gov/medical-devices/precision-medicine/table-pharmacogenetic-associations), had a CPIC guideline (https://cpicpgx.org/guidelines/), were listed as Level A or B on the CPIC Table of Genes-Drugs (https://cpicpgx.org/genes-drugs/), or were on the FDA Table of Biomarkers (https://www.fda.gov/drugs/science-and-research-drugs/table-pharmacogenomic-biomarkers-drug-labeling) and labeled Actionable, Testing recommended, or Testing required in the FDA column of the PharmGKB Drug Label Annotations (https://www.pharmgkb.org/labelAnnotations).
Topical preparations were excluded except for mafenide.4 We included all drug–gene pairs with evidence suggesting a possibility for adverse events. Our list contained 253 MAPBs. Other studies have focused on high level associations such as CPIC Level A drug–gene pairs only4,5 or Dutch Pharmacogenetics Working Group clinical relevance classes C to F.4 The FDA Table of Pharmacogenomic Biomarkers in drug labeling was used to assign a therapeutic area to each MAPB. Those not listed in this table were assigned a therapeutic area by S.F.M.
Dispensed medications with pharmacogenomic biomarkers
To find patients exposed to MAPBs, drug names were used to select a set of drug identification codes from the Cerner Multum™ VantageRx™ database (https://www.cerner.com/solutions/drug-database). These were converted to 11-digit US National Drug Codes and used to filter pharmacy claims.
Simultaneous dispensing of MAPBs
MAPBs were considered codispensed when they had at least 30 consecutive overlapping dispensed days. Days summed for total days dispensed did not all have to be consecutive.
Analysis
Counts and percentages for medications reflect the number of distinct individuals, not the number of pharmacy dispenses. A two-sided t-test was used to compare means.
RESULTS
There were 206 MAPBs in the claims database (see Supplementary Table 1), dispensed in the form of 270 unique single or combination drugs; 1,176,011 beneficiaries (56% of the total population) were dispensed a mean of 2.6 (SD = 2.0) MAPBs. Among adults, 63% (1,049,939) were dispensed at least one MAPB, and among children, this figure was 29% (126,072). Among those with claims for MAPBs, adults were dispensed more (mean 2.7, SD 2.0) medications than children (mean 1.5, SD 1.0, p < 0.001).
The ten most frequently dispensed MAPBs for each age group are shown in Table 1. The two lists have five MAPBs in common, although in different proportions for each age group. Most frequent for children was ondansetron (9.3%), which was number 4 for adults (10%). Most frequent for adults was ibuprofen (17%), which was number 5 for children (2.9%), although this is likely an underrepresentation given the ubiquitous availability of ibuprofen without a prescription. Age group differences for all the MAPBs are presented in Supplementary Table 2. For children, four MAPBs from the top ten were dispensed for more than 180 days, on average (methylphenidate, amphetamine, sertraline, escitalopram). For adults, only one drug in the top ten was dispensed for an average of 180 days or more (omeprazole), which is unsurprising given these drugs are primarily indicated for short-term use. The total days supply for each MAPB is presented in Supplementary Table 3, reflecting the longer duration of use expected for most drugs prescribed for chronic conditions.
The most common biomarker, CYP2D6, was associated with 51 medications dispensed to 98,907 (22%) children, and 63 medications to 731,753 (44%) adults. G6PD was the next most frequent, associated with 26 medications dispensed to 26,312 (6%) children, and 34 dispensed to 435,956 (26%) adults. The next five top genes (CYP2C9, CYP2C19, nonspecific NAT, NAT2, SLC6A4) are common to both age groups, although in a different rank order after the first two. Supplementary Table 4 contains the complete list of biomarkers.
In terms of therapeutic area, 15 MAPBs for gastroenterology were dispensed to 45,159 (10.3%) children, 29 for psychiatry to 33,412 (7.6%), and 13 for neurology for 32,044 (7.3%). These same areas ranked number 3, 4, and 5 for adults. Nine MAPBs for anesthesiology were dispensed to 619,233 (37.4%) adults, 29 for infectious diseases to 370,602 (22.4%), and 14 for gastroenterology to 356,077 (21.5%). The first two adult therapeutic areas were ranked number 4 and 5 for children. Supplementary Table 5 contains the complete list.
Two or more MAPBs were codispensed for at least 30 consecutive days to 6,869 children (1.6%) and 204,748 adults (12.4%). This is 10% of the full population or 18% of those dispensed any MAPB. Table 2 lists the ten most common pairs for each age group as well as descriptive statistics regarding the total number of days the pair was dispensed. Adults were dispensed 5,624 different pairs of MAPBs, and 23% (1,277) of them were unique to single individuals. Children were dispensed 913 different pairs, and 42% (385) were dispensed to single individuals. The MAPBs in the most common pairs differed for adults and children. The most frequent for children were methylphenidate-sertraline (n = 1,130, 0.26%), amphetamine–sertraline (n = 569, 0.13%), and escitalopram–methylphenidate (n = 469, 0.11%). The top ten pairs for children were also observed in adults, but with different percentages and lower rank orders. For adults, the most frequent pairs were metoprolol–rosuvastatin (n = 7,045, 0.43%), metoprolol–pantoprazole (n = 5,666, 0.34%), and clopidogrel–metoprolol (n = 5,252, 0.32%). Of the top ten pairs for adults, five were not observed in children, four were only dispensed to one child, and one (meloxicam–omeprazole) was dispensed to 12 children. All pairs are listed in Supplementary Tables 6 and 7.
DISCUSSION
We find substantial opportunity for pharmacogenomic-guided medication prescribing. MAPBs were dispensed to 56% of a cohort of child and adult beneficiaries of a national health plan over a three-year period. Further, 18% of those prescribed MAPBs are coprescribed an additional MAPB for at least 30 days, potentially increasing risk of toxicity and adverse events, particularly when the metabolic pathway is shared. Adverse drug events are responsible for 4 of 1000 US emergency department visits, with 27.3% resulting in hospitalization.6 Anticoagulants, antibiotics, and diabetic agents are responsible for 47% of these visits, several of which have clinically relevant MAPBs.
A previous study of 10 years of administrative claims from three sources for over 73 million patients with private insurance (from multiple employers/payers across the United States), public insurance (Medicaid from multiple US states), or public/private insurance (employer-paid Medicare supplemental for US retirees) focused on incident use of 61 MAPBs during a four-year period.4 Two genetic testing strategies were evaluated: pre-emptive (at the start of the four-year period, before any MAPBs were dispensed), and a mixed strategy where testing would occur at the time the first MAPB was used. Incident use for younger patients (age 0 to 13) was quite low (11–14% depending on data source) and few received 2 drugs (1–2%) in the pre-emptive group. Older age groups had higher incidence, up to 55% for the public insurance group (age 40 to 64) and 51% for those age 65 and older who were covered by both government and supplemental private insurance. Incident use of a second drug was 33% and 27%, respectively for these two adult age groups.
A recent study projected prevalence of genes associated with CPIC Level A drugs using sequencing data from the 1000 Genomes Project.7 They estimated that almost all 7.7 million veterans who used the US Veterans Health Administration pharmacy could potentially benefit from pharmacogenetic guided prescribing because they had a gene with actionable medication recommendations.5 In fact, 55% were dispensed a Level A drug.
A recent pilot study offered clinical pharmacogenomic testing to 667 patients in five cardiology and four perioperative clinics.8 The 41-gene panel contained 12 genes with CPIC guidelines. Both CPIC drugs and FDA labels were used to identify actionable gene–drug pairs. MAPBs were prescribed to 46% of the 600 patients with medication data. Depending on source of information (FDA, CPIC), 88% or 99% of the patients had an actionable test result, with 5% or 16% currently prescribed an associated medication. One lesson learned from this pilot study was that additional expertise, perhaps from automated clinical decision support systems consultants, might help providers better utilize pharmacogenomic recommendations.
We were able to assess prevalence of MAPB use in two distinct age groups covered by the same national insurer. Our finding that 29% of children age 0 to 17 and 63% of adults age 18 to 64 had MAPBs dispensed, is in keeping with prior studies, given that our expanded drug list included medications with any evidence of actionability as described in the methods. In addition, 10% of the people in the cohort were dispensed more than one MAPBs simultaneously, which further complicates potential clinical decisions.
This study has limitations. The cohort is restricted to a single, though large, private insurer with formulary restrictions. Patients 65 and older were not assessed. A general limitation of pharmacy claims for measuring medication use is that not all dispensed medications are necessarily taken by the patient as prescribed, and some medications may be purchased without exercising a pharmacy benefit. Further, though we measured total exposure of the cohort to MAPBs, we did not estimate the magnitude of benefit from pharmacogenomic-guided prescribing. Of course, genotype does not universally correspond to phenotype, so a predicted drug metabolism response may be inaccurate. Medication metabolism involves factors beyond genetics, including drug–drug interactions, organ function, and diet.
In contrast to diagnostic genomic testing—which risks incidental findings, can implicate unconsented genetically related family members, and can identify of risks of unknown significance—pharmacogenomic testing poses few medical, ethical, or legal dilemmas. Yet unresolved obstacles prevent widespread real-time use of pharmacogenomic variants, including difficulties integrating large sets of retrievable genomic data into electronic health records and scaling clinician decision support.9 However, the near ubiquitous use of electronic health records and emerging standards for point of care integration of external data sets and applications may soon make decision support at scale possible.10,11,12,13,14
Profiling an individual patient’s response to medications is a rapidly maturing capability. Most pharmacogenomic testing is performed reactively after development of toxicity or nonresponse.15 Pre-emptive screening16 will likely increase as microarray-based genetic testing and next-generation sequencing become more affordable. Effectiveness of on-demand as well as pre-emptive pharmacogenomic testing should be both modeled and measured.17 Advancing clinical practice requires thorough evaluation of diagnostic testing strategies and expansion of the limited number of pharmacogenomic-based prescribing guidelines.
Data availability
Raw data for this study were pharmacy claims and membership and enrollment information from a private insurer. The Data Use Agreement does not allow the investigators to share these beneficiary level data. The supplementary materials contain counts derived from the raw data files. In particular, Supplementary Table 2 has counts of the number of enrollees who were dispensed each MAPB by age group and for the whole cohort.
References
Abbasi, J. Getting pharmacogenomics into the clinic. JAMA 316, 1533–1535 (2016).
Relling, M. V., Klein, T. E. & Gammal, R. S. et al. The Clinical Pharmacogenetics Implementation Consortium: 10 years later. Clin. Pharmacol. Ther. 107, 171–175 (2020).
Whirl-Carrillo, M., McDonagh, E. M. & Hebert, J. M. et al. Pharmacogenomics knowledge for personalized medicine. Clin. Pharmacol. Ther. 92, 414–417 (2012).
Samwald, M., Xu, H. & Blagec, K. et al. Incidence of exposure of patients in the United States to multiple drugs for which pharmacogenomic guidelines are available. PLoS One 11, e0164972 (2016).
Chanfreau-Coffinier, C., Hull, L. E. & Lynch, J. A. et al. Projected prevalence of actionable pharmacogenetic variants and level A drugs prescribed among US Veterans Health Administration pharmacy users. JAMA Netw. Open 2, e195345 (2019).
Shehab, N., Lovegrove, M. C. & Geller, A. I. et al. US emergency department visits for outpatient adverse drug events, 2013-4. JAMA. 316, 2115–2125 (2016).
Auton, A., Brooks, L. D. & Durbin, R. M. et al. A global reference for human genetic variation. Nature. 526, 68–74 (2015).
Smith, D. M., Peshkin, B. N., Springfield, T. B. et al. Pharmacogenetics in practice: estimating the clinical actionability of pharmacogenetic testing in perioperative and ambulatory settings. Clin. Transl. Sci. 13, 618–627 (2020).
Relling, M. V. & Evans, W. E. Pharmacogenomics in the clinic. Nature. 526, 343–350 (2015).
Kho, A. N., Rasmussen, L. V. & Connolly, J. J. et al. Practical challenges in integrating genomic data into the electronic health record. Genet. Med. 15, 772–778 (2013).
Mandl, K. D. & Kohane, I. S. No small change for the health information economy. N. Engl. J. Med. 360, 1278–1281 (2009).
Manzi, S. F., Fusaro, V. A. & Chadwick, L. et al. Creating a scalable clinical pharmacogenomics service with automated interpretation and medical record result integration—experience from a pediatric tertiary care facility. J. Am. Med. Inform. Assoc. 24, 74–80 (2017).
Mathias, P. C., Hendrix, N. & Wang, W. J. et al. Characterizing pharmacogenomic-guided medication use with a clinical data repository. Clin. Pharmacol. Ther. 102, 340–348 (2017).
Warner, J. L., Jain, S. K. & Levy, M. A. Integrating cancer genomic data into electronic health records. Genome Med. 8, 113 (2016).
Vassy, J. L., Stone, A. & Callaghan, J. T. et al. Pharmacogenetic testing in the Veterans Health Administration (VHA): policy recommendations from the VHA Clinical Pharmacogenetics Subcommittee. Genet. Med. 21, 382–390 (2019).
Gammal, R. S., Caudle, K. E., Klein, T. E. & Relling, M. V. Considerations for pharmacogenomic testing in a health system. Genet. Med. 21, 1886–1887 (2019).
Marquart, J., Chen, E. Y. & Prasad, V. Estimation of the percentage of US patients with cancer who benefit from genome-driven oncology. JAMA Oncol. 4, 1093–1098 (2018).
Acknowledgements
This study was supported by a postdoctoral fellowship from Aetna (D.L.), funding from the Boston Children’s Hospital PrecisionLink Initiative, and by cooperative agreement U01TR002623 from the National Center for Advancing Translational Sciences (NCATS)/National Institutes of Health (NIH) and R01GM104303 from The National Institute of General Medical Sciences (NIGMS), NIH. None of the funding organizations influenced the design of the study, or the collection, analysis, or interpretation of the data.
Author information
Authors and Affiliations
Contributions
Conceptualization: K.D.M. Methodology D.L., K.L.O. Data curation: S.F.M., D.L., K.L.O. Formal analysis: D.L., K.L.O. Writing: D.L., K.L.O., S.F.M., K.D.M.
Corresponding author
Ethics declarations
Ethics declaration
Boston Children’s Hospital Institutional Review Board approved waiving consent for this study. Risks were determined to be minimal with no potential for direct benefit. Aetna gave approval for the manuscript submission, confirming that no beneficiaries were identifiable.
Competing interests
S.F.M. is a Scientific Advisory Board member at Global Gene, Inc. Quest Diagnostics sponsors research for and contributes philanthropy for K.D.M.’s research program at Boston Children’s Hospital. The other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Liu, D., Olson, K.L., Manzi, S.F. et al. Patients dispensed medications with actionable pharmacogenomic biomarkers: rates and characteristics. Genet Med 23, 782–786 (2021). https://doi.org/10.1038/s41436-020-01044-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-020-01044-2
This article is cited by
-
Implementation of pharmacogenomic clinical decision support for health systems: a cost-utility analysis
The Pharmacogenomics Journal (2022)