Abstract
Purpose
The 2015 American College of Medical Genetics and Genomics/Association for Molecular Pathology (ACMG/AMP) guidelines for the interpretation of sequence variants provide a framework to standardize terminology in the classification of variants uncovered through genetic testing. We aimed to assess the validity of utilizing clinical response to therapies specifically targeted to a suspected disease in clarifying variant pathogenicity.
Methods
Five families with disparate clinical presentations and different genetic diseases evaluated and treated in multiple diagnostic settings are summarized.
Results
Extended evaluations indicated possible genetic diagnoses and assigned candidate causal variants, but the cumulative clinical, biochemical, and molecular information in each instance was not completely consistent with the identified disease. Initiation of treatment specific to the suspected diagnoses in the affected individuals led to clinical improvement in all five families.
Conclusion
We propose that the effect of therapies that are specific and targeted to treatable genetic diseases embodies an in vivo physiological response and could be considered as additional criteria within the 2015 ACMG/AMP guidelines in determining genomic variant pathogenicity.
Similar content being viewed by others
INTRODUCTION
The guidelines for the interpretation of sequence variants formulated through the joint efforts of the American College of Medical Genetics and Genomics (ACMG) and Association for Molecular Pathology (AMP) are an important framework to standardize how laboratories, researchers, clinicians, and others categorize and curate the ever-increasing number of sequence variants uncovered during the course of molecular testing to determine the genetic etiology of human diseases.1 Accurate variant classifications are critical for clinical management decisions and recurrence risk discussions, in addition to guiding research pursuits and determining eligibility for clinical trials. Assigning a pathogenic or benign direction and strength to a variant relies on information in population, disease-specific, and sequence databases; predictions from numerous in silico algorithms; inheritance patterns; and the published literature. If there is an insufficient amount of relevant data, then a classification of “uncertain significance” is assigned. Functional studies can assist in these circumstances and thus comprise strong criteria in determining a variant’s pathogenic (PS3) or benign (BS3) nature. However, model or experimental systems have inherent limitations, it is difficult to test every identified variant, and often, functional assays do not exist or are not readily accessible.
There are an increasing number of targeted therapeutic options available to personalize management and treatment for genetic diseases (e.g., nutritional therapies, medical diets, enzyme therapies, antisense oligonucleotides, gene therapies, small molecular inhibitors, chaperone therapies), which if initiated in a patient, the ensuing physiologic reaction is, in effect, an in vivo functional response. In this article we highlight multiple cases in which variants were identified that did not have enough evidence to score as pathogenic according to the 2015 ACMG/AMP guidelines, but positive clinical responses to treatments targeted to the suspected genetic conditions provided useful functional evidence of variant pathogenicity.
MATERIALS AND METHODS
Patients were evaluated by diagnosticians following standard clinical practice (Supplementary Data). Genetic testing results were as reported by the performing laboratories. Variant calls were re-evaluated by two independent variant analysis teams incorporating current information. Informed consent for testing and publication was obtained from all families. Formal research ethics approval at each of the institutions was not required because the cases initially were evaluated independently, and then retrospectively identified and compiled.
RESULTS
Clinical reports
Family 1
This case is described in detail in Shen et al.2 In brief, the proband was evaluated because of hepatomegaly and the diagnosis of lysosomal acid lipase (LAL) deficiency (MIM 278000) was suspected. However, the Lalistat2 assay repeatedly indicated normal or mildly low enzymatic activity, and although sequencing of LIPA uncovered compound heterozygous variants (c.260G>T, p.Gly87Val and c.853C>T, p.Pro285Ser) in trans, only one was classified as pathogenic.2
The proband was started on sebelipase alfa and there has been improvement in her transaminases, dyslipidemia, hepatomegaly, and liver pathology.
Family 2
The proband presented at 11 years old for poor ability to gain weight (Z-score = −2.70) and gastroparesis. Her 9-year-old brother had hypotonia starting at 3 years old but, in contrast to his sister, was without weight concerns.
A comprehensive biochemical and pathological workup (Supplementary Data) did not indicate a diagnosis. Clinical exome sequencing revealed a previously reported likely pathogenic homozygous TK2 variant (c.173A>G, p.Asn58Ser) present in both the proband and her brother, suggestive of thymidine kinase 2 (TK2)-related mitochondrial DNA depletion syndrome (MIM 609560). However, at the time of diagnosis, patients were reported as having a severe clinical course with early respiratory failure and death, while both siblings denied any respiratory issues; additionally, cachexia was not a known phenotypic feature.
The siblings were enrolled in an expanded access protocol for nucleoside bypass therapy3,4 (Dr. Michio Hirano, Columbia University, New York, NY, USA). There has been a dramatic increase in the proband’s weight (Z-score = −6.28 prior to therapy, Z-score = −1.59 after 6 months of therapy), and improvements in objective measures of strength, endurance, and pulmonary function for both the proband and her brother (personal communication, M. Hirano).
Family 3
The proband presented at 2 years of age because of falling episodes and intellectual disability. Her electroencephalogram (EEG) was consistent with absence seizures and she was started on clobazam.
An extensive workup indicated a disorder of serine biosynthesis, likely 3-phosphoglycerate dehydrogenase (PHGDH) deficiency (MIM 601815) (Supplementary Data). However, all reported cases of PHGDH deficiency have significantly decreased cerebrospinal fluid (CSF) serine levels (Supplementary Table S1) while hers was only minimally decreased at 22.9 micromol/L (normal range 25.0–56.0 micromol/L). Additionally, in vitro PHGDH enzymatic activity assayed as normal (29 nmol/min/mg protein, normal range 20–70 nmol/min/mg protein). PHGDH sequencing uncovered previously unreported compound heterozygous variants (c.1117G>T, p.Ala373Ser and c.792+6T>G) in the trans configuration.
Oral L-serine 250 mg/kg/day supplementation was started and within 3 months, her seizures decreased and her antiepileptic medication was stopped. Her developmental progress improved and therapy services were no longer required after 12 months. After more than 2.5 years of serine supplementation, she attends regular classes and neurodevelopmental evaluations assess her as age-appropriate.
Family 4
The proband was referred at 28 months of age for severe encephalopathy and epilepsy since 10 months of age. Her younger sister had seizures as a neonate and at 11 months of age, but when evaluated at 16 months of age was developmentally normal.
After extensive evaluations (Supplementary Data) did not uncover an etiology, exome sequencing showed a homozygous PNPO variant of uncertain significance (c.500T>C, p.Ile167Thr), suggestive of pyridoxamine 5’-phosphate oxidase (PNPO) deficiency (MIM 610090), that was also present in her sister; each parent was heterozygous. Pyridoxine 20 mg/kg/day was started and seizures improved in the proband although no new developmental skills were acquired, while her sister has been seizure-free and continues with age-appropriate developmental progress.
Family 5
The proband had congenital normocytic anemia requiring transfusions every 5–7 weeks, neutropenia, and nephrolithiasis. Exome sequencing did not reveal a likely diagnosis.
Subsequent metabolic testing (Supplementary Data) showed urine orotic acid of ~3000 micromol/mmol creatinine (normal range 0–4 micromol/mmol creatinine), leading to a suspicion of hereditary orotic aciduria, or uridine monophosphate synthase (UMPS) deficiency (MIM 258900). Retrospective analysis of the exome data revealed compound heterozygous UMPS variants both originally called as likely benign (c.866A>G, p.Asp289Gly and c.1064A>C, p.Gln355Pro) inherited one from each parent.
Uridine was started (250 mg daily, then 250 mg twice daily). His leukocyte count has normalized, and he has not needed a transfusion for more than 33 weeks at the time of this report.
DISCUSSION
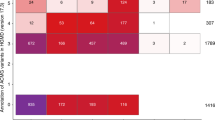
All of the patients described had detailed clinical assessments followed by thorough biochemical and molecular evaluations indicating a likely diagnosis, with genetic testing uncovering relevant missense and intronic variants (Supplementary Table S3). However, when critically evaluating the cumulative information in each family, important aspects were conflicting or insufficiently abnormal to fully “clinch” the diagnosis (Table 1, Supplementary Data). Initiation of therapy and supplementation specifically targeted to the presumed disease led to significant improvement clinically and across objective measures, helping to confirm the diagnosis that was originally suspected.
Alternative explanations could be proposed to account for the therapeutic responses observed. The proband in family 1 could have a lipid metabolism disorder unable to be identified through exome sequencing that was ameliorated by sebelipase alfa; however, a newer LAL assay demonstrated clear enzymatic deficiency.2 For the proband in family 3, perhaps resolution of her developmental delay and seizures was the natural course of her disease independent of any therapy, but a trial off serine led to seizure relapse, supporting a treatment effect. For the sisters of family 4, there could be additional loci responsible for their clinical responses as pyridoxine (and pyridoxal 5-phosphate) administration has led to seizure improvement in individuals without identifiable variants in ALDH7A1 or PNPO.5,6,7,8 For the remaining two families, supplementation with deoxycytidine and deoxythymidine (family 2) and uridine (family 5) is known only to have effects on the biochemical pathways to which they are targeted.
As it has been more than 4 years after sequencing was performed for three of these families, including two prior to the 2015 ACMG/AMP guidelines, additional molecular information and newer prediction algorithms would be available to refine the classification of their variants. However, variant reanalyses for all five families did not more strongly indicate pathogenicity (Table 1, Supplementary Table S4).
The passage of time has provided additional insight into variant pathogenicity through other means, instead. The assay confirming LAL deficiency for the proband of family 1 was developed 3 years after this disease was first suspected.2 Two years after genetic testing of family 2, published information from larger cohorts of individuals affected with TK2-related mitochondrial DNA depletion syndrome indicated that the siblings’ discordant phenotype fits within the broader disease spectrum.9,10 For the sisters of family 4, plasma vitamin B6 vitamer studies have demonstrated that the correct pathway is targeted (Supplementary Data).
With the clinical improvement in our families after initiation of targeted therapies, we were able to accelerate the timeline of confirming the pathogenicity of their variants. In our view, this capability to rapidly classify variants adds a significant and impactful aspect to their positive responses to treatment, second in importance only to the clinical benefit itself.
We propose that new criteria are added to the 2015 ACMG/AMP guidelines that take into account clinical response to treatment for a genetic disease, with a positive benefit representing a human-based in vivo physiologic response and thus justifying a pathogenic strong (PS level) assertion, while lack of a clear effect would be a benign supporting (BP level) code. These response to treatment criteria would be considered meaningful corroborative evidence, but are not intended to be sufficient by themselves or standalone, in determining variant pathogenicity. The missense variants described in this article are likely hypomorphic alleles, which especially in autosomal recessive diseases generally are difficult to classify. Various disease/gene groups under the ClinGen umbrella are evaluating modifications of the ACMG/AMP guidelines criteria to determine how best to include minor allele frequencies (MAF) and other information that can assist in clarifying the pathogenicity of these types of variants.11,12,13 For our families, clinical improvement and objective measures of treatment response as incorporated through our proposed criteria led to recharacterization of multiple variants of uncertain significance to likely pathogenic (Table 1, Supplementary table S4). For two variants already designated as likely pathogenic, as often is the case, with current guidelines this is the most pathogenic direction that the laboratory could assign to the variant with the limited information available. Inclusion of therapeutic response assisted in driving classification to complete pathogenicity.
We categorically do not envision or recommend that treatment is started solely for the purpose of variant classification. It is important that a full genomic workup has been performed and, from a clinical perspective, there needs to be sufficiently high suspicion for an identified disease in a patient to justify potential side effects and logistical difficulties associated with initiating therapy. Additionally, the value of the treatment response in providing functional evidence of variant pathogenicity is tied to and proportional to how specific and targeted the therapeutic option is to the affected gene product, molecular pathway, and suspected diagnosis. As an example, levocarnitine can be helpful in numerous inborn errors of metabolism so any benefit is nonspecific and may not assist in reclassifying variants through our proposed criteria. Our families underwent thorough and extensive evaluations that narrowed down the diagnostic considerations, pinpointing which biochemical pathways were affected and implicating the associated disorders for which specific treatment options were available. Although we recognize that other loci could underlie some of their clinical responses to treatment (as one of the PHGDH variants was still classified as benign there could be another variant missed by the original genetic testing or another disorder of serine biosynthesis responsive to serine supplementation for family 3; another form of pyridoxine-dependent epilepsy for family 4; and anemia in CAD deficiency which improves with uridine supplementation14 for family 5), additional relevant variants were not identified through exome sequencing.
Rapid molecular diagnostics capabilities are being implemented more widely,15,16,17,18,19 and a variety of treatment options are becoming available with personalized medicine initiatives.20 It is our hope that additional criteria such as those we have proposed can be utilized in variant classification to help in definitively assigning pathogenicity, allowing earlier initiation of appropriate treatment to actualize the benefit and purpose of these rapid diagnostic techniques in improving the clinical outcome and lives of patients affected by genetic disorders.
References
Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–423.
Shen JJ, Davis JL, Hong X, et al. A case of lysosomal acid lipase deficiency confirmed by response to sebelipase alfa therapy. J Pediatr Gastroenterol Nutr. 2020. https://doi.org/10.1097/MPG.0000000000002870. Online ahead of print.
Chanprasert S, Wang J, Weng S, et al. Molecular and clinical characterization of the myopathic form of mitochondrial DNA depletion syndrome caused by mutations in the thymidine kinase (TK2) gene. Mol Genet Metab. 2013;110:153–161.
Garone C, Garcia‐Diaz B, Emmanuele V, et al. Deoxypyrimidine monophosphate bypass therapy for thymidine kinase 2 deficiency. EMBO Mol Med. 2014;6:1016–1027.
Plecko B, Paul K, Mills P, et al. Pyridoxine responsiveness in novel mutations of the PNPO gene. Neurology. 2014;82:1425–1433.
Veerapandiyan A, Winchester SA, Gallentine WB, et al. Electroencephalographic and seizure manifestations of pyridoxal 5′-phosphate-dependent epilepsy. Epilepsy Behav. 2011;20:494–501.
Goyal M, Fequiere PR, McGrath TM, Hyland K. Seizures with decreased levels of pyridoxal phosphate in cerebrospinal fluid. Pediatr Neurol. 2013;48:227–231.
Mills PB, Camuzeaux SSM, Footitt EJ, et al. Epilepsy due to PNPO mutations: genotype, environment and treatment affect presentation and outcome. Brain. 2014;137:1350–1360.
Garone C, Taylor RW, Nascimento A, et al. Retrospective natural history of thymidine kinase 2 deficiency. J Med Genet. 2018;55:515–521.
Wang J, Kim E, Dai H, et al. Clinical and molecular spectrum of thymidine kinase 2-related mtDNA maintenance defect. Mol Genet Metab. 2018;124:124–130.
Richards CS, Aziz N, Bale S, et al. Response to Biesecker and Harrison. Genet Med. 2018;20:1689–1690.
Tavtigian SV, Greenblatt MS, Harrison SM, et al. Modeling the ACMG/AMP variant classification guidelines as a Bayesian classification framework. Genet Med. 2018;20:1054–1060.
Abou Tayoun AN, Pesaran T, DiStefano MT, et al. Recommendations for interpreting the loss of function PVS1 ACMG/AMP variant criterion. Hum Mutat. 2018;39:1517–1524.
Koch J, Mayr JA, Alhadadad B, et al. CAD mutations and uridine-responsive epileptic encephalopathy. Brain. 2017;140:279–286.
Berg JS, Agrawal PB, Bailey DB, et al. Newborn sequencing in genomic medicine and public health. Pediatrics. 2017;139:e20162252.
Brunelli L, Jenkins SM, Gudgeon JM, et al. Targeted gene panel sequencing for the rapid diagnosis of acutely ill infants. Mol Genet Genomic Med. 2019;7:e796.
Elliott AM, du Souich C, Lehman A, et al. RAPIDOMICS: rapid genome-wide sequencing in a neonatal intensive care unit—successes and challenges. Eur J Pediatr. 2019;178:1207–1218.
Kingsmore SF, Cakici JA, Clark MM, et al. A randomized, controlled trial of the analytic and diagnostic performance of singleton and trio, rapid genome and exome sequencing in ill infants. Am J Hum Genet. 2019;105:719–733.
Meng L, Pammi M, Saronwala A, et al. Use of exome sequencing for infants in intensive care units: ascertainment of severe single-gene disorders and effect on medical management. JAMA Pediatr. 2017;171:e173438.
van Karnebeek CDM, Wortmann SB, Tarailo-Graovac M, et al. The role of the clinician in the multi-omics era: are you ready? J Inherit Metab Dis. 2018;41:571–582.
Acknowledgements
We thank the families for participating in this study. We thank Michio Hirano for kindly providing updated clinical information. R.v.d.L. was supported by a Rubicon fellowship from the Netherlands Organization for Scientific Research (NWO & ZONMW, 452172015).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
S.R., C.D.C., and M.R.H. are employees of PerkinElmer Genomics, Inc., but were not involved in the testing of these families. The other authors declare no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shen, J.J., Wortmann, S.B., de Boer, L. et al. The role of clinical response to treatment in determining pathogenicity of genomic variants. Genet Med 23, 581–585 (2021). https://doi.org/10.1038/s41436-020-00996-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-020-00996-9
Keywords
This article is cited by
-
An AI-based approach driven by genotypes and phenotypes to uplift the diagnostic yield of genetic diseases
Human Genetics (2024)
-
The clinical utility of rapid exome sequencing in a consanguineous population
Genome Medicine (2023)
-
Mitochondrial “dysmorphology” in variant classification
Human Genetics (2022)
-
Treatable inherited metabolic disorders causing intellectual disability: 2021 review and digital app
Orphanet Journal of Rare Diseases (2021)
-
Correspondence on “The role of clinical response to treatment in determining pathogenicity of genomic variants” by Shen et al.
Genetics in Medicine (2021)