Abstract
Purpose
To estimate the value of genomic sequencing for complex pediatric neurological disorders of suspected genetic origin.
Methods
A discrete choice experiment (DCE) was undertaken to elicit societal preferences and values. A Bayesian D-efficient and explicit partial profile design was used. The design included 72 choice tasks, split across six blocks, with eight attributes (three overlapping per choice task) and three alternatives. Choice data were analyzed using a panel error component mixed logit model and a latent class model. Preference heterogeneity according to personal socioeconomic, demographic, and attitudinal characteristics was explored using linear and fractional logistic regressions.
Results
In total, 820 members of the Australian public were recruited. Statistically significant preferences were identified across all eight DCE attributes. We estimated that society on average would be willing to pay AU$5650 more (95% confidence interval [CI]: AU$5500 to $5800) (US$3955 [95% CI: US$3850 to $4060]) for genomic sequencing relative to standard care. Preference heterogeneity was identified for some personal characteristics.
Conclusion
On average, society highly values all diagnostic, process, clinical, and nonclinical components of personal utility. To ensure fair prioritization of genomics, decision makers need to consider the wide range of risks and benefits associated with genomic information.
Similar content being viewed by others
INTRODUCTION
Complex neurological disorders (CNDs) are characterized by significant genetic heterogeneity causing developmental delay, intellectual disability, seizures, physical disabilities, and behavioral problems. The process of establishing a diagnosis has, in most cases, been long and challenging,1,2 due to the heterogeneous and nonspecific clinical presentations.3 This process involves a multitude of clinical evaluations and investigations with low diagnostic utility, including imaging, biochemical and metabolic testing, biopsies, chromosomal microarray, and single or panel gene testing.1,2,3,4 The sequential pursuit of diagnosis commonly results in a costly diagnostic odyssey,2,5 posing significant health, social, and economic challenges to patients and families.6,7
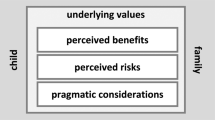
Genomic sequencing (GS) has come to shape a new paradigm for the diagnosis and management of rare genetic conditions,8 with studies increasingly demonstrating significant diagnostic and clinical outcomes in the context of neurology.3 Nonclinical outcomes, including the value of information, the knowledge about the condition, and the opportunity to make informed choices, enhance coping, and access peer support, are also increasingly evidenced.9 The aggregate value of the diagnostic, clinical, and nonclinical value components of GS is commonly referred to as personal utility.10,11 While the benefits of GS are predominantly emphasized,12 concerns associated with data protection and privacy, secondary findings, and the purpose and result of GS, for example when genomic information leads to uncertainty, anxiety, emotional distress, or guilt, are equally well documented.13
The criteria determining reimbursement decisions for genomic technologies are as yet unclear,14 and the complexity of GS has brought up significant challenges to assessing value for money.15,16 An increasing body of evidence generated using preference elicitation methods, which explicitly require tradeoffs between risks and benefits, is demonstrating that patients and society, on average, highly value the personal utility of GS.16,17,18,19,20 To enable informed reimbursement decisions, the value of GS needs to reflect the utility or disutility associated with the different outcomes generated.16 One promising method to valuing the wide range of outcomes of GS for informing health-care priorities is the discrete choice experiment (DCE),21 and interest in the application of DCEs in health economics and, more specifically, in the context of genomics is increasing.16,22
This study reports the findings of a large DCE conducted to estimate the value that Australian society places on GS for children with CNDs of suspected genetic origin. Our findings can be used in a cost–benefit analysis to establish whether GS of children with CNDs should be reimbursed in publicly funded health-care systems.
MATERIALS AND METHODS
Ethics statement
Informed consent was obtained from all participants prior to entering the survey. Ethics approval was granted from the Medicine and Dentistry Human Ethics Sub-Committee of the University of Melbourne (Ethics ID: 1852388).
Study design and participants
A survey was developed to elicit societal preferences and values for different components of personal utility associated with GS in the context of pediatric CNDs. The survey was designed following best practice recommendations.23,24 Focus groups were conducted to identify and develop the DCE attributes.25 Detailed information about the focus groups is available elsewhere.26 In brief, clinical genomics staff, operational genomics staff, and community representatives with lived experience of rare genetic conditions and CNDs were purposefully selected to provide a broad range of perspectives and experiences. Focus groups adopted a multiphase mixed methods approach involving quantitative ratings and qualitative discussions. An iterative and coproductive approach with all participating stakeholders was then used to finalize the selection and labeling of attributes.25 Attribute levels were identified in consultation with the genetic experts of the research team to ensure clinical face validity.
The final attributes and corresponding levels are provided in Table 1. The attributes were (1) number of children who receive a genetic diagnosis, (2) chance of improving the process of the child’s medical care, (3) availability of treatments, (4) time until your child does the test, (5) time between test and results, (6) enabling access to other services and professional or peer support, (7) enabling access to clinical trials, and (8) cost of testing to you. Similar to Goranitis et al.,20 individual-specific cost levels (in Australian dollars) conditional on participants' self-reported annual household income were used. This approach ensures fairness in the marginal disutility of cost levels across participants and reflects the way the Australian health-care system is funded with income proportional tax contributions.20
We used a Bayesian D-efficient and explicit partial profile design developed with Ngene (ChoiceMetrics [2018] Ngene 1.2 User Manual & Reference Guide, Australia). The experimental design included 72 choice tasks split across six blocks based on the minimum correlation principle, with each participant required to complete 12 choice tasks. Choice tasks were drawn from a candidate set of all relevant attribute combinations using the modified Federov algorithm.27 Restrictions were applied to the algorithm to ensure fair representation of all attribute levels without imposing attribute level balance. Bayesian priors accommodate the uncertainty associated with parameter values using distributions that ensure minimal loss of statistical efficiency in the design in cases of prior parameter misspecification. Bayesian priors for the pilot survey were informed by published evidence, where available, and the expectations of the research team.28 Explicit partial profiles with three overlapping attributes were chosen to reduce task complexity and avoid dominancy issues.27,29 Different overlapping attributes or levels were used across choice tasks.
Choice tasks required participants to indicate the situation under which they would prefer their child to have GS. Participants could choose either one of the two GS situations provided (situation 1 or situation 2) or the opt-out option (“I would not like my child to have a genomic test”). A choice task example is shown in Fig. 1. The survey was initially piloted in 85 members of the Australian adult population, recruited through an online panel firm (Dynata [formerly Research Now SSI]), and pilot results were used to refine the DCE experimental design and final survey. The survey is available in the Supplementary material.
An Australia-wide sample of participants over the age of 18, stratified by age, gender, and income, was recruited through the online panel firm. The sample size was determined based on the S-efficiency measure, which indicates the lower bound of the sample size required to obtain statistically significant parameter estimates at the 5% significance level when parameter priors have been correctly specified.30 Societal preferences were sought per current health economics gold-standard practice on valuing outcomes.31 The representativeness of the sample in these variables was validated against other national sources.32 Several randomizations were applied to safeguard the study findings from possible biases and errors. Initially, a randomization of participants to one of the six blocks was applied. Further randomization was applied (1) in the order of choice tasks within blocks, (2) in the order of the two GS situations to control for a left-to-right bias, and (3) to a survey version with or without pictogram for the attribute “number of children who receive a genetic diagnosis” to control for potential framing effect.
Choice analysis
Choice data were analyzed using a panel error component mixed logit model, which uses random parameters to account for unobserved heterogeneity of preferences among participants. The error component additionally allows for a covariance structure in the error variances of the GS situations.23 Continuous coding was applied for the attributes “number of children who receive a genetic diagnosis," “chance of improving the process of the child’s medical care," “time until your child does the test," “time between test and results," and “cost of testing to you” to facilitate estimations of incremental benefits in a cost–benefit analysis. Dummy coding was used for the remaining attributes. A constrained triangular distribution was used for the cost and time attributes as a result of their established disutility.23 A normal distribution was used for the other parameters. Random parameters were estimated using 1000 standard Halton sequences. To determine the relative importance of each attribute on individuals’ choice, we estimated importance scores by comparing the range in estimated utility between best and worst attribute levels divided by the sum of the utility ranges across attributes. Importance scores, therefore, reflect the proportion of the overall change in utility, when moving from worst to best levels across attributes, that corresponds to each of the attributes.
Marginal willingness-to pay (WTP) values for the DCE attributes were estimated using the conditional and unconditional population moments estimates.23 The delta method was used to generate 95% confidence intervals (CIs). We then estimated the overall WTP, as a measure of value, and predicted uptake of GS on the basis of assumptions regarding the incremental difference between GS and standard care for each of the DCE attributes using the sample preferences. Given that risk–benefit tradeoffs are likely to vary within CNDs, different assumptions can be made in a similar way to enable estimations of context-specific WTP values. Based on the study by Vissers et al.,2 an incremental diagnostic and clinical utility of 22% and 24% was assumed for GS. We assumed an additional availability of specific and nonspecific treatment options in 3% and 5% of the children respectively.5 The average length of the testing period under standard care was assumed to be 40 months,2 and the time to a molecular diagnosis with GS was assumed to be 14 months.5 Finally, it was assumed that GS is reimbursed by the government and that it enables access to clinical trials and to other services and professional or peer support for all additional children being diagnosed through GS. The additional value of GS relative to standard care was estimated based on the compensating variation formula.33 The uptake of GS was estimated based on the percentage of the population predicted to choose GS.34 Both WTP and uptake estimates were produced based on population simulated data incorporating identified preference heterogeneity using robust and quintile regressions.23 WTP values are reported in both Australian and US dollars (using 1 January 2020 Reserve Bank of Australia exchange rate of 0.70). All analyses were undertaken using NLOGIT 6 (Econometric Software, Inc., Waverton, NSW, Australia).
We used two approaches to explore participants’ heterogeneity of preferences. The first approach relied directly on the outputs of the main choice model. More specifically, we obtained the estimated individual parameters for marginal utilities and GS choice probability. We used linear regression to explore utility differences depending on socioeconomic, demographic, and attitudinal characteristics. Fractional logistic regression was used to explore preference heterogeneity for the probability of choosing GS. The second approach relied on a latent class (LC) choice model,35 which splits the sample into a finite number of groups (classes) with distinct preferences. Preferences within groups are assumed to be homogeneous. We estimated a model with five classes based on the Bayesian information criterion (BIC). A fractional logistic regression was then used to explore whether personal characteristics were significantly associated with class membership probabilities. These analyses were conducted in Stata 16 (StataCorp, College Station, TX, USA).
RESULTS
In total, 820 members of the Australian adult population participated in the study. Detailed information about the socioeconomic, demographic, and attitudinal characteristics is provided in the Supplementary material (Table S1). In short, the mean age was 46 years, with 55.8% of study participants being married (44.5%) or in a committed relationship (11.3%). Nearly 25% of the sample had a university-level education, with a further 15% having undertaken additional postuniversity studies. The majority of participants reported being parents (55.6%) and having annual household income of less than AU$100k (75.3%). Approximately 38% of participants had heard about GS prior to the study, with 28.3% and 16.6% reporting direct (themselves) or indirect (close family members or friends) experience with genetic conditions and genetic testing respectively. Other than being relatively more educated, participants were representative of the Australian public in terms of age, gender, marital status, and household income. The histograms of participants’ familiarity with the effect of genetic conditions on patients and families, knowledge about genetics, attitudes toward GS, and health are available in the Supplementary material (Figure S1).
Table 2 presents participants’ preferences for the different attributes. On average, participants’ utility for GS increased when more children received genetic diagnosis, when the chance of improving the process of the child’s medical care increased, when specific and nonspecific treatment options were available, and when GS enabled access to clinical trials or to other services and professional or peer support. Longer time to access the test, longer turnaround times for results, and higher costs caused disutility. Preferences for the attributes “availability of nonspecific treatment options” and “enabling access to other services and professional or peer support” were homogeneous, as evidenced by the non–statistically significant standard deviation estimates (Table 2), which means that there was not statistically significant preference variation from the reported mean. Preference heterogeneity existed across the remaining attributes.
Table 2 presents additional information about the relative importance of each attribute on individuals’ choice. The most important attribute was “chance of improving the process of the child’s medical care," followed by “availability of treatments," “number of children who receive a genetic diagnosis," “cost of testing to you," “time until your child does the test," “enabling access to clinical trials," “enabling access to other services and professional or peer support," and “time between test and results.” The main difference between this ranking and the ranking conducted as part of the focus groups is that focus group members placed more emphasis on receiving genetic diagnosis and accessing professional or peer support and less emphasis on cost,26 possibly due to their professional or lived experience with genetic disease.
The marginal WTP for each attribute is also shown in Table 2. For every additional child in a hundred receiving a diagnosis, participants on average were willing to pay AU$40 (95% CI: AU$35 to $45). For every percentage point increase in the chance of improving the process of the child’s medical care, participants on average were willing to pay AU$88 (95% CI: AU$78 to $97). On average, participants were willing to pay an additional AU$991 (95% CI: AU$701 to $1280) and AU$2810 (95% CI: AU$2484 to $3137) for GS in the presence of available nonspecific and specific treatment options respectively. Participants on average were willing to accept AU$164 (95% CI: AU$130 to $198) and AU$111 (95% CI: AU$67 to $154) to face an additional month waiting to access GS or waiting for the test results respectively. To enable access to other services and professional or peer support, participants on average were willing to pay AU$913 (95% CI: AU$703 to $1124). For enabling access to clinical trials, the average willingness-to pay was AU$921 (95% CI: AU$702 to $1140). Based on published evidence for the additional personal utility of GS relative to standard care for CNDs across the DCE attributes (Table 3), the mean uptake and WTP for GS were estimated at 74% (95% CI: 72% to 76%) and AU$5650 (95% CI: AU$5500 to $5800) (US$3955 [95% CI: US$3850 to $4060]).
Results on personal characteristics as sources of preference heterogeneity for the uptake of GS and the corresponding marginal utilities are shown in Table S2. Participants who had heard about GS before completing the survey and participants with more positive attitudes toward genomics were significantly more likely to take up GS. Having a higher-level education was also marginally significant. For some of the DCE attributes, significant preference heterogeneity was identified in terms of age, gender, income, and attitudes toward health risk. For example, older people on average demonstrated significantly higher utility for the attributes “chance of improving the process of the child’s medical care," “availability of specific treatment options," “enabling access to other services and professional or peer support," “enabling access to clinical trials,” and significantly lower utility for the two time attributes compared with younger people.
Based on the results of the latent class model (Table 4), there are essentially five groups (classes) of participants. Class 1 includes people who have a negative preference for GS but who would consider testing when diagnostic and process utilities are high. Membership in class 1 is significantly associated with no experience of genetic conditions, not having heard about GS prior to the survey, and negative attitudes toward genomics in general (Table S3). About 26% of the sample was grouped in class 1. Class 2 includes 11% of sample participants who had a positive preference for GS regardless of the presence of clinical utility. Class 3 includes people with preferences across all attributes apart from the results turnaround time. There was 19.7% probability for class 3 membership, which was significantly associated with an experience of a genetic condition and higher income levels (Table S3). Class 4 was the largest group, with a class membership probability of 34.8%, which includes people who placed 2–3 times higher value across all attributes compared with class 3. Membership in class 4 was significantly associated with having heard about GS prior to the survey, having positive attitudes toward GS, and having higher-level education. Class 5 includes people who demonstrated high price sensitivity (8.7% of the sample).
DISCUSSION
In this study, we conducted a DCE to elicit the Australian public’s preferences and values for GS in the context of pediatric CNDs of suspected genetic origin. The study demonstrated that society on average highly values all personal utility components of GS. Overall, it was estimated that participants would be willing to pay AU$5650 (US$3955) more for GS in the context of CNDs relative to standard care.
The high value of GS is increasingly demonstrated. A recent study elicited societal preferences (n = 1913) to estimate the WTP for GS, as a measure of value, across pediatric and adult-onset genetic conditions in Australia using a DCE.20 In the pediatric context, the study estimated that society would be willing to pay between AU$5470 (US$3830) and AU$15250 (US$10,675) for GS depending on the risk–benefit tradeoffs involved. Interestingly, the AU$5470 estimate related to the value of GS in complex neurological conditions. The estimate is approximately equal to the value estimated as part of this study. The value of GS for pediatric rare genetic conditions was also explored in Canada based on preferences from parents of children with either confirmed or suspected rare genetic condition (n = 319).19 The study estimated that the value of GS relative to standard operative procedures was US$4943.19 Despite the agreement between the three studies, more evidence is needed to understand how value may differ across a wider range of genetic conditions, across countries, and between people experiencing a genetic condition and society.
Where the evidence base is becoming more established is around the significant value placed across all elements of personal utility derived from GS. The study by Marshall et al.,19 for example, concluded that parents with lived experience of genetic conditions were placing almost equal value, ranging between US$5633 and $6038, on all types of benefits of genomic testing, such as changes to medical management, access to disease-specific services, and knowledge about cause, progression, and family risk. The study by Regier et al.36 concluded that uncertainty around the health benefit from genetic information and the medical expert agreement on changing medical care based on genetic markers had a significant effect on the demand for precision medicine. A study by Buchanan et al.18 demonstrated that patients in the context of chronic lymphocytic leukemia had significant preferences for attributes, such as the length of time clinicians spent describing GS, the type of clinician being involved, and the time to receive the test results. Significant preference for reduced genomic test results turnaround time or for trusting the cancer treatment doctor have also been identified in the context of colorectal and breast cancer by Weymann et al.37 and Marshall et al.38 respectively.
Despite the growing body of evidence demonstrating the strength and heterogeneity of individual preferences for genomics and personalized medicine, there is still limited exploration of the sources of preference heterogeneity, which can be an important tool for optimizing the translation of genomics into clinical care. We found that people who had heard about GS prior to the study and people who had more positive attitudes for genomics were significantly more likely to take up GS. Thus, familiarizing society with the risks and benefits of genomics and personalized medicine may be an important step for the implementation of genomics. We also found that preferences for certain attributes differed depending on personal characteristics, such as age, gender, education, and income; experience with a genetic condition or genetic testing; and attitudes toward health risk. Interestingly, being a parent was not significantly associated with higher uptake rates or systematic preference heterogeneity across DCE attributes. The study by Goranitis et al.20 found that age, education, and attitudes toward genomics had some effect on the utility for GS in both pediatric and adult contexts. Marital status, health status, and attitudes toward health risk influenced the utility for GS in the adult context.20 Similarly, the study by Buchanan et al.18 identified preference heterogeneity in terms of gender, income, health status, and experience with chemotherapy or genetic testing.
Our study estimated the value of GS in the context of CNDs drawing upon preferences and values of a large (n = 820) and reasonably representative sample of the Australian public, despite overrepresenting highly educated adults. The study also benefited from an extensive exploration of preference heterogeneity. There are, however, limitations worth noting. To ensure a nationally representative sample of the Australian public, recruitment was pursued through an established online panel firm. While this recruitment strategy may introduce self-selection or incentive biases, it has been established that such recruitment strategies encompass comparable validity and reliability to traditional recruitment methods.39 Given the hypothetical nature of stated preference methods, a hypothetical bias may also be introduced, whereby description-based choices are different from experienced-based choices. In our study, respondents were asked to imagine themselves as parents of children with CNDs of suspected genetic origin, and therefore the validity of the choices made for their [hypothetical] child can be questioned. Even though DCEs have demonstrated moderate external validity,40 it is still unclear how valid it is to extrapolate from assessments of external validity in the wider health economics literature to the predicted uptake of a novel testing strategy with low current uptake, which is not always appropriately documented.
Our study relied on societal preferences, as recommended when informing health-care priorities,31 but only 38% of the sample had heard about GS prior to completing the survey. This may mean that societal preferences are less informed and different compared with preferences of people experiencing the effects of genetic conditions. Further research comparing societal and patient preferences is essential for determining the appropriate way forward for valuing personal utility in genomics and personalized medicine. Finally, while our design allowed for inclusion of eight attributes, preferences for some important attributes associated with GS were not directly estimated. For example, a major aspect of GS implementation relates to actionable and nonactionable secondary findings. Also, cascade testing in family members of a child with positive GS findings is another issue that may be key for the prioritization of GS. This reflects an inherent tension between optimality and feasibility in DCEs, where relevant but lower ranked attributes are omitted to enable respondents to weigh all attributes in a fully compensatory manner.
In conclusion, our study provides empirical evidence on the value that society places on GS for pediatric CNDs of suspected genetic origin. We conclude that there is substantial personal utility in GS that relates to all diagnostic, clinical, process, and nonclinical components of utility. The monetary valuation of the benefits of GS that this study estimated needs to be compared against the direct and opportunity costs associated with GS to enable informed decisions about the reimbursement of GS in Australia, and possibly beyond. Even though the base criteria for reimbursing genomics and personalized medicine are yet unclear,14 the findings of this study make another strong case for the consideration of all personal utility aspects in the prioritization of genomics and personalized medicine to avoid biased and misinformed resource allocation decisions.
References
Thevenon J, Duffourd Y, Masurel‐Paulet A, et al. Diagnostic odyssey in severe neurodevelopmental disorders: toward clinical whole-exome sequencing as a first-line diagnostic test. Clin Genet. 2016;89:700–707.
Vissers L, van Nimwegen KJM, Schieving JH, et al. A clinical utility study of exome sequencing versus conventional genetic testing in pediatric neurology. Genet Med. 2017;19:1055–1063.
Srivastava S, Love-Nichols JA, Dies KA, et al. Meta-analysis and multidisciplinary consensus statement: exome sequencing is a first-tier clinical diagnostic test for individuals with neurodevelopmental disorders. Genet Med. 2019;21:2413–2421.
Srivastava S, Cohen JS, Vernon H, et al. Clinical whole exome sequencing in child neurology practice. Ann Neurol. 2014;76:473–483.
Soden SE, Saunders CJ, Willig LK, et al. Effectiveness of exome and genome sequencing guided by acuity of illness for diagnosis of neurodevelopmental disorders. Sci Transl Med. 2014;6:265ra168.
Lewis C, Skirton H, Jones R. Living without a diagnosis: the parental experience. Genet Test Mol Biomarkers. 2010;14:807–815.
Carmichael N, Tsipis J, Windmueller G, Mandel L, Estrella E. “Is it going to hurt?”: the impact of the diagnostic odyssey on children and their families. J Genet Couns. 2015;24:325–335.
Clark MM, Stark Z, Farnaes L, et al. Meta-analysis of the diagnostic and clinical utility of genome and exome sequencing and chromosomal microarray in children with suspected genetic diseases. NPJ Genom Med. 2018;3:16.
Kohler JN, Turbitt E, Biesecker BB. Personal utility in genomic testing: a systematic literature review. Eur J Hum Genet. 2017;25:662–668.
Feero WG, Wicklund C, Veenstra DL. The economics of genomic medicine: insights from the IOM Roundtable on Translating Genomic-Based Research for Health. JAMA. 2013;309:1235–1236.
Regier DA, Peacock SJ, Pataky R, et al. Societal preferences for the return of incidental findings from clinical genomic sequencing: a discrete-choice experiment. CMAJ. 2015;187:E190–E197.
Esquivel-Sada D, Nguyen MT. Diagnosis of rare diseases under focus: impacts for Canadian patients. J Community Genet. 2018;9:37–50.
Lewis C, Sanderson S, Hill M, et al. Parents’ motivations, concerns and understanding of genome sequencing: a qualitative interview study. Eur J Hum Genet. 2020;28:874–884.
Grosse SD, Rasmussen SA. Exome sequencing: value is in the eye of the beholder. Genet Med. 2020;22:280–282.
Phillips KA, Deverka PA, Marshall DA, et al. Methodological issues in assessing the economic value of next-generation sequencing tests: many challenges and not enough solutions. Value Health. 2018;21:1033–1042.
Regier DA, Weymann D, Buchanan J, Marshall DA, Wordsworth S. Valuation of health and nonhealth outcomes from next-generation sequencing: approaches, challenges, and solutions. Value Health. 2018;21:1043–1047.
Regier DA, Friedman JM, Makela N, Ryan M, Marra CA. Valuing the benefit of diagnostic testing for genetic causes of idiopathic developmental disability: willingness to pay from families of affected children. Clin Genet. 2009;75:514–521.
Buchanan J, Wordsworth S, Schuh A. Patients’ preferences for genomic diagnostic testing in chronic lymphocytic leukaemia: a discrete choice experiment. Patient. 2016;9:525–536.
Marshall DA, MacDonald KV, Heidenreich S, et al. The value of diagnostic testing for parents of children with rare genetic diseases. Genet Med. 2019;21:2798–2806.
Goranitis I, Best S, Christodoulou J, Stark Z, Boughtwood T. The personal utility and uptake of genomic sequencing in pediatric and adult conditions: eliciting societal preferences with three discrete choice experiments. Genet Med. 2020;22:1311–1319.
Grosse SD, Wordsworth S, Payne K. Economic methods for valuing the outcomes of genetic testing: beyond cost-effectiveness analysis. Genet Med. 2008;10:648–654.
Soekhai V, de Bekker-Grob EW, Ellis AR, Vass CM. Discrete choice experiments in health economics: past, present and future. PharmacoEconomics. 2019;37:201–226.
Hensher DA, Rose JM, Greene WH. Applied choice analysis. 2nd ed. Cambridge: Cambridge University Press; 2015.
Johnson FR, Lancsar E, Marshall D, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR conjoint analysis experimental design good research practices task force. Value Health. 2013;16:3–13.
Coast J, Horrocks S. Developing attributes and levels for discrete choice experiments using qualitative methods. J Health Serv Res Policy. 2007;12:25–30.
Best S, Stark Z, Phillips P, et al. Clinical genomic testing: what matters to key stakeholders? Eur J Hum Genet. 2020;28:866–873.
ChoiceMetrics. User manual & reference guide. Ngene 1.2 ed. Sydney, Australia; 2018.
Bliemer MC, Collins AT. On determining priors for the generation of efficient stated choice experimental designs. J Choice Model. 2016;21:10–14.
Kessels R, Jones B, Goos P. Bayesian optimal designs for discrete choice experiments with partial profiles. J Choice Model. 2011;4:52–74.
Rose JM, Bliemer MC. Sample size requirements for stated choice experiments. Transportation. 2013;40:1021–1041.
Brazier J, Ratcliffe J, Saloman J, Tsuchiya A. Measuring and valuing health benefits for economic evaluation. Oxford: Oxford University Press; 2017.
Australian Bureau of Statistics (ABS). Census QuickStats. 2016. https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/036. Accessed August 2019.
Small KA, Rosen HS. Applied welfare economics with discrete choice models. Econometrica. 1981;49:105–130.
Ryan M, Gerard K, Amaya-Amaya M. Using discrete choice experiments to value health and health care. Dordrecht, Netherlands: Springer; 2007.
Greene WH, Hensher DA. A latent class model for discrete choice analysis: contrasts with mixed logit. Transp Res B Methodol. 2003;37:681–698.
Regier DA, Veenstra DL, Basu A, Carlson JJ. Demand for precision medicine: a discrete-choice experiment and external validation study. PharmacoEconomics. 2020;38:57–68.
Weymann D, Veenstra DL, Jarvik GP, Regier DA. Patient preferences for massively parallel sequencing genetic testing of colorectal cancer risk: a discrete choice experiment. Eur J Hum Genet. 2018;26:1257–1265.
Marshall DA, Deal K, Bombard Y, Leighl N, MacDonald KV, Trudeau M. How do women trade-off benefits and risks in chemotherapy treatment decisions based on gene expression profiling for early-stage breast cancer? A discrete choice experiment. BMJ Open. 2016;6:e010981.
Evans JR, Mathur A. The value of online surveys. Internet Res. 2005;15:195–219.
Quaife M, Terris-Prestholt F, Di Tanna GL, Vickerman P. How well do discrete choice experiments predict health choices? A systematic review and meta-analysis of external validity. Eur J Health Econ. 2018;19:1053–1066.
Acknowledgements
Australian Genomics Health Alliance is funded by a National Health and Medical Research Council (NHMRC) grant (grant reference number 1113531) and the Australian Government’s Medical Research Future Fund (MRFF). The research conducted at the Murdoch Children’s Research Institute was supported by the Victorian Government’s Operational Infrastructure Support Program. This work represents independent research and the views expressed are those of the authors and not necessarily those of the NHMRC or MRFF.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Goranitis, I., Best, S., Stark, Z. et al. The value of genomic sequencing in complex pediatric neurological disorders: a discrete choice experiment. Genet Med 23, 155–162 (2021). https://doi.org/10.1038/s41436-020-00949-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-020-00949-2
Keywords
This article is cited by
-
The value of genomic testing in severe childhood speech disorders
European Journal of Human Genetics (2024)
-
Eliciting parental preferences and values for the return of additional findings from genomic sequencing
npj Genomic Medicine (2024)
-
Determining the utility of diagnostic genomics: a conceptual framework
Human Genomics (2023)
-
QALYs and rare diseases: exploring the responsiveness of SF-6D, EQ-5D-5L and AQoL-8D following genomic testing for childhood and adult-onset rare genetic conditions in Australia
Health and Quality of Life Outcomes (2023)
-
Genomic sequencing for the diagnosis of childhood mitochondrial disorders: a health economic evaluation
European Journal of Human Genetics (2022)