Abstract
Purpose
Pediatric cardiomyopathy is rare, has a broad differential diagnosis, results in high morbidity and mortality, and has suboptimal diagnostic yield using next-generation sequencing panels. Exome sequencing has reported diagnostic yields ranging from 30% to 57% for neonates in intensive care units. We aimed to characterize the clinical utility of exome sequencing in infantile heart failure.
Methods
Infants diagnosed with acute heart failure prior to 1 year old over a period of 34 months at a large tertiary children’s hospital were recruited. Demographic and diagnostic information was obtained from medical records. Fifteen eligible patients were enrolled.
Results
Dilated cardiomyopathy was the predominant cardiac diagnosis, seen in 60% of patients. A molecular diagnosis was identified in 66.7% of patients (10/15). Of those diagnoses, 70% would not have been detected using multigene next-generation sequencing panels focused on cardiomyopathy or arrhythmia disease genes. Genetic testing changed medical decision-making in 53% of all cases and 80% of positive cases, and was especially beneficial when testing was expedited.
Conclusion
Given the broad differential diagnosis and critical status of infants with heart failure, rapid exome sequencing provides timely diagnoses, changes medical management, and should be the first-tier molecular test.
Similar content being viewed by others
INTRODUCTION
Pediatric cardiomyopathy is a rare condition of the myocardium occurring in approximately 4.4 in 100,000 infants per year.1,2,3 Dilated cardiomyopathy (DCM) is the most common subtype affecting the pediatric population, followed by hypertrophic cardiomyopathy (HCM), restrictive cardiomyopathy, and then a mixed or other cardiomyopathy phenotype.3 In one study, 46% of patients with pediatric DCM progressed to death or transplant within the first 5 years of diagnosis, highlighting the often devastating outcomes of pediatric cardiomyopathy.1 The etiologies for pediatric patients with cardiomyopathy are varied and include infections, metabolic diseases, syndromic diagnoses, nonsyndromic familial cardiomyopathy, and idiopathic cardiomyopathy.4,5,6,7,8
Yield of genetic testing varies widely based on the phenotype, age of presentation, and type of testing pursued. Many recent studies have demonstrated a diagnostic yield between 33% and 58% of patients who received exome or genome sequencing for any indication while in a neonatal intensive care unit or while critically ill.10,11,12,13,14 Exome and genome sequencing provide rapid results for patients and families and also change medical management in up to half of cases.11,13 Next-generation sequencing panels identify a genetic diagnosis in 10–60% of cardiomyopathy cases, depending on the subtype and cohort.5 In one cohort of patients with pediatric dilated cardiomyopathy, multigene panel testing yielded a diagnosis in 54% of patients whereas exome sequencing identified a genetic diagnosis in 87% (13/15) of probands.9 Herein, we report the experience of a large tertiary children’s hospital and cardiac transplant center with exome sequencing in neonates and infants with acute presentations of heart failure.
MATERIALS AND METHODS
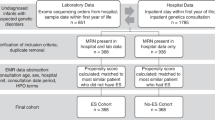
Eighteen patients presented to our institution with heart failure within the first year of life and were evaluated by metabolic and genetics physicians as part of their clinical care between June 2016 and May 2019. Participants were consented into one of two institutional review board (IRB)–approved pediatric genomic sequencing studies at CHOP (IRB #16-013231 and IRB #18-014911) for this prospective observational study. These protocols include permission for publication of de-identified patient data. All appropriate consent and protocol forms have been archived. Three patients (two with DCM, one with HCM) were not enrolled due to parental decision to not participate in this study. Exclusion criteria included anatomic congenital heart disease sufficient to cause the degree of heart failure and age at presentation of greater than 12 months.
Clinical genetic testing recommendations were made by the clinical team per standard of care, and included either standard or rapid exome sequencing with or without concurrent mitochondrial sequencing. Standard exome sequencing was performed by GeneDx (Gaithersburg, MD) or the Children’s Hospital of Philadelphia’s Division of Genomic Diagnostics (Philadelphia, PA). All mitochondrial sequencing and rapid exome sequencing were performed by GeneDx. XomeDxXpress was utilized for its rapid turnaround time of verbal result in 7 days and written report in approximately 2 weeks in nine cases. All testing was trio based, including both parents, with the exception of patient 12 whose father was unavailable for testing. Pertinent demographic, diagnostic, and outcomes data were abstracted from their medical records.
Genetic testing was considered diagnostic when a likely pathogenic or pathogenic variant(s) were identified in gene(s) associated with the patient’s clinical features. In two cases, variants of uncertain significant (VUS) were included in the diagnostic category, as the patients had extracardiac features strongly consistent with these syndromic diagnoses (Table 1). One patient had a homozygous VUS in PPCS and had other features of PPCS deficiency including profound hypotonia and elevated creatine kinase levels. Another patient, who already carried a clinical diagnosis of Noonan syndrome, had one VUS in LZTR1, a Noonan syndrome gene.
Change in management for probands was defined as initiating targeted treatment based on genetic testing, consultation of other pertinent subspecialties, or redirection of care. Change in management for family members was defined as identifying genetic predisposition to cardiomyopathy in family members without a known history of cardiomyopathy, change in recurrence risk counseling, or clearance of family members from cardiac surveillance.
RESULTS
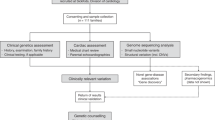
Fifteen patients with infantile heart failure who had exome sequencing recommended as part of their diagnostic evaluation were enrolled (Table 1). Of those, 60% of patients presented with dilated cardiomyopathy (Fig. 1a). The median age of diagnosis of cardiomyopathy was 10 days (range 0 days to 8 months). Seven patients (46.7%) were diagnosed prenatally or within the first 48 hours of life (Fig. 1b). Patient 11 was the only with a first- or second-degree relative with cardiomyopathy prior to the patient’s presentation. Rapid exome sequencing was sent for nine patients (60%), with a median written report turnaround time of 10 days (range 9–14). Standard exome sequencing in the remaining six patients had a median turnaround time of 42 days (range 29–71). Nine of 15 (60%) had mitochondrial DNA sequencing at the time of exome sequencing, all of which was normal. At the time of publication, 9/15 (60%) patients were alive. All six deceased patients died as a result of redirection of care, either due to clinical status or genetic diagnosis. Two patients underwent successful cardiac transplantation.
Exome sequencing was diagnostic in 10/15 (67.7%) patients (Table 1; Supplementary Table 1). Seventy percent of these diagnoses would have been missed using standard cardiomyopathy panels at the majority of commercial laboratories investigated. All six patients with extracardiac manifestations prior to testing received diagnoses via exome sequencing. Four of nine without extracardiac manifestations received diagnoses. Four metabolic or mitochondrial cardiomyopathies were identified: NDUF11-related disorder (OMIM 300403), ACAD9 deficiency (OMIM 611103) PPCS-related cardiomyopathy (OMIM 609853), and mitochondrial trifunctional protein deficiency (OMIM 609015). Four syndromic diagnoses were identified: Noonan syndrome (OMIM 600574), Alström syndrome (OMIM 203800), X-linked agammaglobulinemia (OMIM 300705), and NAA15-related neurodevelopmental disorder (OMIM 608000). Only two of ten diagnoses were in primarily cardiac related genes: MYH7 (OMIM 613426) and FLNC (OMIM 102565).
Exome sequencing results changed the patient’s medical management in eight cases (53.3%) and changed familial management in two-thirds of cases. Three families chose to reorient care goals away from aggressive life support, such as extracorporeal membrane oxygenation, based on the genetic testing results and prognosis. In the case of ACAD9 deficiency, riboflavin supplementation was initiated in conjunction with other cardiac medications with subsequent resolution of his severe ventricular dysfunction and dilation, and improvement in left ventricular hypertrophy. For syndromic diagnoses, multiple subspecialist evaluations were initiated.
DISCUSSION
Exome sequencing in infantile heart failure has a high diagnostic yield (67%) in our cohort and impacted medical management in all diagnostic cases. Genes for 70% of diagnoses were not on cardiomyopathy panels and would have been missed without the use of exome sequencing. Extracardiac manifestations may have been challenging to identify in critically ill neonates for many of the syndromic diagnoses identified in our cohort. As such, exome sequencing was critical for making a diagnosis and ensuring proper care, regardless of time to result, though additionally so for rapid testing. For example, patient 9 was a healthy infant girl who presented with acute decompensated heart failure at 2 months of age and was identified to have Alström syndrome via rapid exome sequencing. Not only were results returned in a timely manner allowing the intensive care team to provide prognostication information for the family, but also other subspecialists were involved for the syndromic nature of this disease. The child has since been noted to have cone–rod dystrophy, photophobia, nystagmus, and elevated triglycerides. These manifestations of the disease were not identified until targeted subspecialist screening was initiated due to the molecular diagnosis. Additionally, her mother was able to have targeted genetic testing via chorionic villus sampling for her ongoing subsequent pregnancy, which confirmed the fetus was unaffected.
The diagnoses identified in this cohort demonstrate the wide clinical spectrum of diagnoses that can present with infantile heart failure, notably metabolic and syndromic diagnoses in the majority of patients with diagnostic exome sequencing. This highlights the importance of genetics and metabolism specialists in the diagnostic work-up for patients with infantile heart failure. While this study is limited by a relatively small cohort size at one medical center, infantile heart failure due to cardiomyopathy is a rare disease and diagnostic yields were consistent with other larger studies of exome sequencing in neonatal or pediatric intensive care units.10,11,12,13,14 Further studies including cost–benefit analysis and multicenter prospective studies may help refine the diagnostic yield and clinical utility of rapid exome sequencing in this unique population. In conclusion, given the broad differential diagnosis and critical status of infants with heart failure, rapid exome sequencing provides timely diagnoses, changes medical management, and should be the first-tier molecular test for infantile heart failure.
References
Towbin JA, Lowe AM, Colan SD, et al. Incidence, causes, and outcomes of dilated cardiomyopathy in children. JAMA. 2006;296:1867–1876.
Lipshultz SE, Sleeper LA, Towbin JA, et al. The incidence of pediatric cardiomyopathy in two regions of the United States. N Engl J Med. 2003;348:1647–1655.
Wilkinson JD, Westphal JA, Bansal N, Czachor JD, Razoky H, Lipshultz SE. Lessons learned from the Pediatric Cardiomyopathy Registry (PCMR) Study Group. Cardiol Young. 2015;25 suppl 2:140–153.
Kindel SJ, Miller EM, Gupta R, et al. Pediatric cardiomyopathy: importance of genetic and metabolic evaluation. J Card Fail. 2012;18:396–403.
Hershberger RE, Givertz MM, Ho CY, et al. Genetic evaluation of cardiomyopathy: a clinical practice resource of the American College of Medical Genetics and Genomics (ACMG). Genet Med. 2018;20:899–909.
Tariq M, Ware SM. Importance of genetic evaluation and testing in pediatric cardiomyopathy. World J Cardiol. 2014;6:1156–1165.
Ware SM. Genetics of paediatric cardiomyopathies. Curr Opin Pediatr. 2017;29:534–540.
Byers SL, Ficicioglu C. Infant with cardiomyopathy: when to suspect inborn errors of metabolism? World J Cardiol. 2014;6:1149–1155.
Herkert JC, Abbott KM, Birnie E, et al. Toward an effective exome-based genetic testing strategy in pediatric dilated cardiomyopathy. Genet Med. 2018;20:1374–1386.
Willig LK, Petrikin JE, Smith LD, et al. Whole-genome sequencing for identification of Mendelian disorders in critically ill infants: a retrospective analysis of diagnostic and clinical findings. Lancet Respir Med. 2015;3:377–387.
Stark Z, Tan TY, Chong B, et al. A prospective evaluation of whole-exome sequencing as a first-tier molecular test in infants with suspected monogenic disorders. Genet Med. 2016;18:1090–1096.
Mestek-Boukhibar L, Clement E, Jones WD, et al. Rapid Paediatric Sequencing (RaPS): comprehensive real-life workflow for rapid diagnosis of critically ill children. J Med Genet. 2018;55:721–728.
Meng L, Pammi M, Saronwala A, et al. Use of exome sequencing for infants in intensive care units: ascertainment of severe single-gene disorders and effect on medical management. JAMA Pediatr. 2017;171:e173438.
Daoud H, Luco SM, Li R, et al. Next-generation sequencing for diagnosis of rare diseases in the neonatal intensive care unit. CMAJ. 2016;188:E254–E260.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
J.J., D.C. and S.Y. are employees of GeneDx, Inc. The other authors declare no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ritter, A., Bedoukian, E., Berger, J.H. et al. Clinical utility of exome sequencing in infantile heart failure. Genet Med 22, 423–426 (2020). https://doi.org/10.1038/s41436-019-0654-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-019-0654-3
Keywords
This article is cited by
-
The expanding diagnostic toolbox for rare genetic diseases
Nature Reviews Genetics (2024)
-
Tools to differentiate between Filamin C and Titin truncating variant carriers: value of MRI
European Journal of Human Genetics (2023)
-
Comprehensive Genetic Testing for Pediatric Hypertrophic Cardiomyopathy Reveals Clinical Management Opportunities and Syndromic Conditions
Pediatric Cardiology (2022)