Abstract
Purpose
Exome sequencing (ES) has the potential to improve management of congenital anomalies and neurodevelopmental disorders in fetuses, infants, and children. US payers are key stakeholders in patient access to ES. We examined how payers view insurance coverage and clinical utility of pediatric and prenatal ES.
Methods
We employed the framework approach of qualitative research to conduct this study. The study cohort represented 14 payers collectively covering 170,000,000 enrollees.
Results
Seventy-one percent of payers covered pediatric ES despite perceived insufficient evidence because they saw merit in available interventions or in ending the diagnostic odyssey. None covered prenatal ES, because they saw no merit. For pediatric ES, 50% agreed with expanded aspects of clinical utility (e.g., information utility), and 21% considered them sufficient for coverage. For prenatal ES, payers saw little utility until in utero interventions become available.
Conclusion
The perceived merit of ES is becoming a factor in payers’ coverage for serious diseases with available interventions, even when evidence is perceived insufficient. Payers’ views on ES’s clinical utility are expanding to include informational utility, aligning with the views of patients and other stakeholders. Our findings inform clinical research, patient advocacy, and policy-making, allowing them to be more relevant to payers.
Similar content being viewed by others
INTRODUCTION
Congenital anomalies and neurodevelopmental disorders affect 3–5% of live-born infants and children.1 These conditions are among the leading causes of infant mortality.2 Life-saving and progression-curbing interventions tailored to some of these conditions are now available, but many interventions must be applied expediently, given the possibility of rapid disease progression.3,4 Accurate and timely genetic diagnosis is critical, but traditional testing methods, such as chromosomal microarray (CMA) and single-gene and/or gene panel tests, produce lower diagnostic rates5 and may take the patient/family and clinicians on a prolonged diagnostic odyssey.6,7
Exome sequencing (ES), using next-generation sequencing technology, offers a broader and more comprehensive diagnosis of pediatric and prenatal genetic diseases than tradition testing. Studies have demonstrated that ES diagnosed up to 78% of pediatric neurodevelopmental disorders when other tests did not yield a result8,9 and led to changed medical management in 30% of diagnosed cases.10 Time-to-diagnosis advantages have been shown in studies of rapid genome and/or exome sequencing in the neonatal/pediatric intensive care unit setting.11,12 ES was also determined to be more cost-effective than traditional testing.13
As a result, ES is being adopted into clinical practice to diagnose suspected neurodevelopmental genetic conditions in children—either in conjunction with CMA or as a first-line test.14,15 Given the ES diagnostic advantages, it is also being evaluated for use in the prenatal setting, usually following a normal CMA result,16 to diagnose ultrasound-detected fetal structural anomalies, which affect 2–3% of pregnancies.17 Adding prenatal ES to CMA has been shown to increase the rate of genetic diagnosis of fetal anomalies, Compared with standard of care testing.18,19 The increased genetic diagnosis rate has the potential to improve family counseling and to inform prenatal and neonatal medical management. However, at this time, prenatal ES is considered emergent and experimental, due to the small body of evidence of clinical benefit and few proven in utero interventions available.16 As new evidence of ES’s benefit is demonstrated and new fetal therapies for prenatally detected congenital disorders are available outside of the research setting, prenatal ES is likely to become increasingly integrated into clinical practice.
For sustainable clinical adoption in the pediatric and prenatal settings, ES must be covered by insurance payers. Although it is possible to receive reimbursement for a novel genomic technology from a US payer without a formal positive coverage policy, the absence or variability of formal positive coverage leads to payment uncertainty, variation in clinical practice, and barriers to access, particularly for underserved populations. A study of US payers’ policies has shown that coverage for pediatric ES increased between 2015 and 2017 but remained fragmented: nearly half of payers whose policies were reviewed did not formally cover pediatric ES.20 Prenatal ES is currently not formally covered in the US, although it is sometimes possible to receive payment. To facilitate more consistent insurance coverage of pediatric ES, as well as future coverage for prenatal ES and other novel genomic tests, it is crucial to understand payers’ coverage decision-making related to these technologies. This understanding is essential to inform researchers developing relevant evidence, clinicians ordering ES, patient advocacy efforts, and the work of policy makers.21
The objective of our study was to examine US payers’ views and perspectives on pediatric and prenatal ES in the context of coverage decision-making. We focused on the perspective of private payers because private payers cover two-thirds of the insured US population.22 The study was conducted at the University of California–San Francisco (UCSF) within the Program in Prenatal and Pediatric Genomic Sequencing (P3EGS). P3EGS is a part of the Clinical Sequencing Evidence-Generating Research (CSER) consortium, and this study is aligned with CSER objectives to engage key stakeholders, including payers.23 This study builds on our previous research on payer coverage decision-making for genomics.24,25,26 These data add to our understanding of payers’ perspectives regarding pediatric and prenatal ES and how payers view their clinical utility. We focused on clinical utility because it is a central concept in payers’ coverage decision-making.25,26,27 Our findings are significant and timely for stakeholders not only in pediatric and prenatal ES but also in other current and future genomic innovations.
MATERIALS AND METHODS
We used the modified framework approach of qualitative research to design and conduct this semistructured interview study.28,29 The study was reviewed by the University of California at San Francisco (UCSF) Institutional Review Board. The study was classified as exempt under category 2 (Research using educational tests, survey procedures, interview procedures or observation of public behavior), and verbal consent was obtained of all interviewees.
Study cohort
Study participants were members of the UCSF Center For Translational and Policy Research on Personalized Medicine (TRANSPERS) Payer Advisory Council.30 The Council was established in 2007, and its members have participated in a number of our previous studies on payer decision-making.24,25,26 The Council is comprised of senior executives from 14 US payer entities, including the 8 largest national health plans, 3 major regional health plans, 1 state Medicaid agency, and 2 non–health plan bodies (a multipayer association and a laboratory benefit management company). Payers participating in the Council collectively cover over 170,000,000 lives. We invited all 14 Council members to take part in our study, and they all participated.
The non–health plan entities were invited because they develop coverage policies or coverage recommendations for health plans. For the purposes of this study, we refer to all participants as payers, to protect the individual and company anonymity. All participants were decision-makers regarding coverage for genomic technologies in their respective organizations: for example, a chief medical officer, a vice president of medical policy, a head of genetics, and other senior positions.
Developing the interview guide
To inform the development of the interview guide, we conducted a literature review and discussions with six clinical and/or research experts on pediatric and prenatal ES: four UCSF P3EGS investigators and two outside experts. The interviews collected their perspectives on the benefits and risks of pediatric and prenatal ES, with a specific focus on clinical utility. Experts also suggested questions for payer interviews that would be of interest to clinicians and researchers.
Based on literature review and expert input, we developed a semistructured interview guide. The guide included interview questions (see Table 1 for an excerpt), as well as background and context, such as a description of the standard of care testing for congenital anomalies and neurodevelopmental disorders and the role of ES in management of these conditions. The interview questions asked about the level of interest in prenatal and pediatric ES, the reasons that payers covered or did not cover these technologies, how they perceived risks of ES in these settings, and what they thought about suggestions provided by experts on how to facilitate coverage of pediatric and prenatal ES (see Table 1).
In addition, the interview guide contained background and questions related to the clinical utility of pediatric and prenatal ES. To frame these questions, we reviewed definitions of the clinical utility of genomic tests in the literature. The debate over how to define clinical utility is ongoing, and numerous definitions have been proposed.31,32 They vary in breadth (e.g., whether it is improvement in health outcomes, or also the ability to diagnose and/or change clinical management), and in scope (e.g., whether it pertains only to the patient tested, or also to the family). To explore payers’ perspectives, we followed the recommendation by the American College of Medical Genetics and Genomics (ACMG) to expand the framing of clinical utility to a broader, multifaceted view of clinical utility for genomics.33 We used a definition adapted from ACMG: clinical utility of genetic testing is a continuum of benefits, which encompasses a spectrum of aspects, including the value of a diagnosis to the individual and family, as well as effects on diagnostic or therapeutic management, and implications for prognosis, health, and physiological benefits to patients and their relatives.
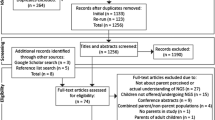
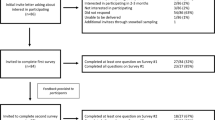
Guided by this definition, and informed by discussions with experts, we conceptualized clinical utility for pediatric and prenatal ES in two diagrams (Figs. 1 and 2), which were included with the interview guide. One of the interview questions explored whether payers agreed with the various aspects of clinical utility conceptualized in the diagrams and whether these aspects were independently sufficient for granting coverage to pediatric and/or prenatal ES.
Data collection and analysis
Semistructured interviews were conducted with the study cohort from January through April 2019. The interviews were conducted over the phone; they lasted 45–60 minutes each, were recorded, with interviewee’s verbal consent, and later transcribed verbatim for analyses. Interviewees received the study description and the interview guide in advance. They were promised that all results would be reported in an unattributable, anonymous, and aggregate fashion. No interviewees were offered or received payment for participation. Two investigators (J.R.T., C.B.W.) conducted thematic analyses and coding of the transcribed interviews. Disagreements were resolved by discussion and consensus. Simple frequencies were used to further describe the findings.
RESULTS
Payers’ interest in and coverage of pediatric and prenatal ES
Considerably more payers reported high or medium interest in pediatric than prenatal ES (Table 2). Cited reasons for high and medium interest in pediatric ES were significant test implications, both positive and negative; the serious nature of relevant conditions; and cost concerns driven by high test prices and increasing usage of pediatric ES. Payers with low interest explained it by insufficient demand from their physician networks, the perception that ES is not ready for clinical practice, and competing internal priorities related to genetic testing, such as cancer genetics.
Most payers in our cohort noted that their organizations provided (or recommended) coverage for pediatric ES (71%, 10/14), while none covered prenatal ES (Table 2). Payers covering pediatric ES found evidence of its clinical utility insufficient but recognized the merit of the test (i.e., saw the overall underlying need for it). The merit for pediatric ES was based on its potential to inform the available clinical interventions (70%, 7/10) or to end the diagnostic odyssey (30%, 3/10). However, half of the payers covering pediatric ES still expressed concerns about potential inappropriate use, expanding indications, and difficulty interpreting test results. Hence, they established limitations on covered clinical scenarios and ordering specialties, and some have implemented prior authorization and utilization management programs.
In contrast to pediatric ES, where payers saw some, albeit insufficient evidence, they found no evidence of clinical utility for prenatal ES, and some of them doubted the ability to generate enough evidence in the future. Also, the majority saw no merit in its use, explaining that the lack of in utero interventions outside of research settings obviated the need to perform ES in the prenatal versus postnatal setting, where interventions are available. Thus, in their opinions, ES added no informational value above prenatal ultrasound and standard genetic testing.
How payers viewed clinical utility of pediatric and prenatal ES
The obtained insights regarding clinical utility are summarized in Table 3 and described below. The interviews assessed two angles: whether payers agreed with a specific aspect of ES’s clinical utility (Table 3, column 2), and whether they considered this aspect independently sufficient for coverage if other aspects are absent and/or unproven (Table 3, column 3).
Pediatric ES
Payers viewed aspects of the clinical utility of pediatric ES relative to the current standard of testing. All payers agreed that from a coverage perspective, the incremental impact on clinical outcomes for pediatric patients tested with ES versus standard is the most desirable aspect of clinical utility. However, a sizable minority (43%, 6/14) considered a change in clinical management and/or another aspect of clinical utility as acceptable and sufficient for coverage (Table 3).
While 64% (9/14) of payers perceived withdrawal of futile interventions as a valid component of clinical utility, only 36% (5/14) viewed it as independent and stand-alone. Others commented that this aspect is secondary to outcome improvement and change in interventions, and therefore should not be used independently to demonstrate the utility of a genetic test. As one interviewee stated: “I hope we are not using genetics to discontinue care for patients. I would not encourage that this sort of treatment futility is demonstrated through a genetic test.”
Similarly, 50% (7/14) of payers acknowledged the informational utility of ES (directing family to disease-specific support, education, and research), but most regarded informational utility as secondary to other aspects of clinical utility. Only three payers considered informational utility as potentially sufficient for coverage if evidence demonstrated an impact on patient care. None of the payers regarded utility for family care—reproductive decisions or diagnosis for siblings—as independently sufficient for coverage. They commented that “supporting or informing the family is not the primary reason to use ES—these should be linked to other aspects. For example, a support group is important for parents when stopping futile care or transferring to hospice.”
The end of the diagnostic odyssey was viewed by most payers (64%, 9/14) as a valid aspect of clinical utility, and several of them considered it sufficient for coverage (Table 3). These payers agreed with Fig. 1 that the end of the diagnostic odyssey is different from informational utility, in that it stops further genetic testing and may inform disease-specific medical management. However, of these nine payers, only two agreed that receiving a negative result may, in fact, end the diagnostic odyssey. Others noted that “on the surface, the rule-out utility makes sense, but only if we can resolve the challenge of VUS (variants of unknown significance) or inaccurate results, which may result in additional work that could be unnecessary or harmful.”
Prenatal ES
Here, payers discussed clinical utility not only relative to standard testing but also compared with testing ES after birth. Overall, 79% (11/14) of payers expressed difficulty recognizing the clinical utility of prenatal ES, in the absence of proven in utero clinical interventions. Consequently, they viewed other aspects of clinical utility in Fig. 2 as secondary and not relevant until in utero interventions become available in clinical practice. All interviewed payers stated that they would not consider pregnancy termination as an intervention or an aspect of clinical utility in the context of coverage policy. Provided reasons included regulatory, political, and/or ethical challenges, and skepticism that a genetic diagnosis adds to the termination decision beyond sonographic results.
Likewise, most payers expressed skepticism that prenatal ES and an in utero genetic diagnosis provide any incremental value compared with sonography and CMA testing. Accordingly, 57% (8/14) of payers thought that referral to a tertiary center for delivery and specialized newborn management should happen anyway, based on abnormal ultrasound results. All payers described other aspects of clinical utility (informing withdrawal of futile interventions, informational utility, and utility for parents’ reproductive decisions) as occurring after birth, and therefore relevant to the pediatric but not prenatal clinical utility of ES (Table 3). Several payers noted that availability of rapid sequencing made a timely diagnosis after birth feasible and obviated the necessity for prenatal ES. One payer added that in exceptional circumstances, ES may be performed several weeks before birth, to prepare for the immediate neonatal intervention.
Payers’ opinions on potential risks and harms of pediatric and prenatal ES
All interviewed payers argued that considerations of clinical utility include not only potential benefits of ES but also potential risks and harms. Each payer expressed several concerns of risks and harms, including the impact of VUS on additional testing, care, and costs; VUS-related anxiety for families and clinicians; difficulty interpreting ES results; accuracy of ES; uncertainty of how to handle secondary genetic findings; and psychological trauma of genetic diagnosis for parents. Payers believed that the risks and harms were higher in the prenatal setting, where the absence of clinical interventions and the inability to phenotypically examine the baby add to the uncertainty of diagnosis and management and elevate parents’ stress. This was one of the reasons they saw higher net utility for pediatric than prenatal ES.
Payers’ responses to experts’ suggestions for insurance coverage of pediatric and prenatal ES
In preparing the interview guide, experts made two suggestions for expanding insurance coverage of pediatric ES and establishing coverage for prenatal ES. First, they suggested that for rare serious conditions, such as pediatric congenital anomalies and neurodevelopmental disorders, the research setting is the only one available for patients to receive clinical care; therefore, payers should consider covering ES as part of this care. In the interviews, 21% (3/14) of payers agreed that research in these settings could be considered clinical practice because of the very rare conditions and high disease burden. However, they noted regulatory and business challenges in providing insurance coverage in research settings. Other payers did not agree with this suggestion because covering research would contradict their mission and contractual obligations to employers and enrollees. They also noted that it would be challenging to decide which research settings, diseases, and modalities should or should not be covered.
Second, experts suggested coverage of pediatric and prenatal ES only when ordered by selected tertiary centers with specialized resources able to interpret results and provide adequate care. A slight majority of payers (57%, 8/14) agreed that this approach could be effective and appropriate for pediatric and prenatal ES. They described similar approaches in managing other rare and complex conditions, such as organ transplant, by developing a network of centers of excellence. Nevertheless, they stated challenges associated with such programs: establishing clear criteria, quality metrics, and standards for participating centers, and addressing the needs of patients in remote locations from tertiary centers. Several payers, both affiliated and not affiliated with Blue Cross Blue Shield, shared that they were considering such networks for complex modalities such as ES.
DISCUSSION
This study examined perspectives of a cohort of US payers on insurance coverage for pediatric and prenatal ES for congenital anomalies and neurodevelopmental disorders. We found that 71% of the payer cohort covers pediatric ES, despite perceived insufficient evidence, because they see merit in available interventions or in ending the diagnostic odyssey. None of them covered prenatal ES, primarily because they saw no merit in prenatal versus postnatal ES (79%). Our study also examined how payers viewed an expanded spectrum of clinical utility for ES, beyond the impact on clinical outcomes and management. For pediatric ES, at least 50% agreed with expanded aspects of clinical utility, including ending diagnostic odyssey, informational utility (directing family to disease-specific support, education, and research) or family utility for reproductive decision-making. Moreover, 21% considered ending the diagnostic odyssey and informational utility independently sufficient for coverage. None of the payers viewed information utility as a compelling aspect of clinical utility prenatally until in utero interventions are available in clinical practice.
Previous studies explored payers’ views on other genomic tests, including those in cancer and pharmacogenomics.24,25,26,34 They found that while payers use a range of considerations in coverage decision-making, sufficient evidence of clinical utility was a central and necessary factor for coverage. In contrast, we found that for pediatric neurodevelopmental disorders and congenital anomalies, the perceived merit of ES was a key factor in coverage, despite perceptions of insufficient clinical evidence. This finding suggests that payers’ perception of merit is a concept that should be further studied to understand how it is shaped, if/how it applies to other clinical areas, and how it relates to other coverage decision-making factors.
Consistent with previous studies, payers in our cohort consider the impact on clinical outcomes and management as primary aspects of clinical utility. However, unlike prior studies, our findings indicate that payers are open to accepting expanded aspects of clinical utility, notably diagnostic and informational utility, for settings with available clinical interventions, such as pediatric neurodevelopmental disorders. Personal and family information utility has been deemed important by medical societies who urged their inclusion in the scope of the clinical utility of genomics.33,35 It has also been shown of value to parents of children with rare genetic disorders undergoing exome sequencing.7 Our findings imply that payers’ views on the clinical utility of genomic sequencing are evolving toward higher congruence with those of other constituencies.
Our study may have implications for a range of stakeholders in the field of genomic sequencing, including clinicians, researchers, patient advocates, policy makers, and payers themselves. Our results inform the efforts of researchers studying established and emergent applications of ES to produce evidence of clinical utility relevant to payers and other audiences. One such effort is the UCSF P3EGS program, under which this study was conducted. P3EGS is a part of the CSER consortium and is aimed at investigating clinical utility for pediatric and prenatal ES.36 Although many payers cover pediatric ES, coverage varies across payers and often has limited indications.20 By generating evidence of clinical utility relevant to payers’ expectations, P3EGS and other investigators could help facilitate broader and more consistent coverage. Likewise, for emerging sequencing tests, such as prenatal ES, payers’ perspectives on clinical utility in the context of available interventions could help design relevant studies, as well as shape broader research priorities, focused on developing interventions in clinical areas where they are lacking.
Our study may be instructive to patient advocates, policy makers, and others aiming to improve equitable access to genomic technologies, particularly for underrepresented and minority patients. Understanding how payers evaluate these technologies may inform advocacy and policy work and potentially make it more effective. We also believe that the expanded conceptualization of clinical utility for ES developed in this study could be applied to other clinical areas and used to facilitate dialogues with a broader range of stakeholders. We plan to pursue this avenue by examining clinical utility from the broader perspective across CSER sites and stakeholders, and working with the Clinical Utility, Health Economics, and Policy (CUHEP) working group formed within the CSER consortium.37
As the genomic field is likely to transition from exome to genome sequencing,38 understanding payers’ coverage considerations will become increasingly important. Genome sequencing may exacerbate payers’ concerns about merit and utility in various diseases, and the risks and harms from VUS. This and future studies on payer decision-making will help to frame a cohesive and proactive research, advocacy, and policy agenda for integrating genomic sequencing into coverage policy, reimbursement, and clinical practice.
Our study had several limitations. We used a relatively small cohort of payers, although collectively, their policies affect over 170 million enrollees. Public payers who cover substantial numbers of underserved and minority populations were underrepresented in our cohort. Medicaid is especially relevant to coverage for pediatric and prenatal disorders, but we were unable to broadly examine Medicaid policy decision-making in this study. Engaging Medicaid and other public payers in direct interview studies has been a challenge for researchers. Public multistakeholder forums organized by quasi-government bodies such as the National Academy of Medicine may be a more feasible mechanism to elucidate their insight on coverage for sequencing technologies. Finally, some experts recommend encompassing cost-effectiveness as an aspect of the clinical utility of genomic testing. We did not include cost-related aspects in the scope of our study. Future research should elucidate whether and how payers consider cost-effectiveness as an aspect of clinical utility in coverage decisions.
Conclusions
We examined the views of US payers on insurance coverage and clinical utility of exome sequencing (ES) for congenital anomalies and neurodevelopmental disorders in pediatric and prenatal settings. We found that the perceived merit of ES is becoming a factor in payers’ coverage for serious diseases, such as pediatric neurodevelopmental disorders, with available interventions, even when payers consider clinical evidence insufficient. We also found that payers’ perspectives on ES are evolving to include expanded aspects of clinical utility, notably information utility. This may indicate a trend toward higher congruence of payers’ perspectives with those of patients and other stakeholders. Future research should elucidate payers’ views on expanded clinical utility for exome and genome sequencing across diseases. Our findings inform clinical research, patient advocacy, and policy-making, allowing their efforts to be more relevant in a dialogue with payers.
References
Feldkamp ML, Carey JC, Byrne JLB, Krikov S, Botto LD. Etiology and clinical presentation of birth defects: population based study. BMJ. 2017;357:j2249.
Mone F, Quinlan-Jones E, Ewer AK, Kilby MD. Exome sequencing in the assessment of congenital malformations in the fetus and neonate. Arch Dis Child Fetal Neonatal Ed. 2019;104:F452–F456.
Soden SE, Saunders CJ, Willig LK, et al. Effectiveness of exome and genome sequencing guided by acuity of illness for diagnosis of neurodevelopmental disorders. Sci Transl Med. 2014;6:265ra168.
Willig LK, Petrikin JE, Smith LD, et al. Whole-genome sequencing for identification of Mendelian disorders in critically ill infants: a retrospective analysis of diagnostic and clinical findings. Lancet Respir Med. 2015;3:377–387.
Clark MM, Stark Z, Farnaes L, et al. Meta-analysis of the diagnostic and clinical utility of genome and exome sequencing and chromosomal microarray in children with suspected genetic diseases. NPJ Genom Med. 2018;3:16.
Lewis C, Skirton H, Jones R. Living without a diagnosis: the parental experience. Genet Test Mol Biomarkers. 2010;14:807–815.
Marshall DA, MacDonald KV, Heidenreich S, et al. The value of diagnostic testing for parents of children with rare genetic diseases. Genet Med. 2019 Jun 26; https://doi.org/10.1038/s41436-019-0583-1 [Epub ahead of print].
Vissers L, van Nimwegen KJM, Schieving JH, et al. A clinical utility study of exome sequencing versus conventional genetic testing in pediatric neurology. Genet Med. 2017;19:1055–1063.
Niguidula N, Alamillo C, Shahmirzadi Mowlavi L, Powis Z, Cohen JS, Farwell Hagman KD. Clinical whole-exome sequencing results impact medical management. Mol Genet Genomic Med. 2018;6:1068–1078.
Stark Z, Tan TY, Chong B, et al. A prospective evaluation of whole-exome sequencing as a first-tier molecular test in infants with suspected monogenic disorders. Genet Med. 2016;18:1090–1096.
Petrikin JE, Cakici JA, Clark MM, et al. The NSIGHT1-randomized controlled trial: rapid whole-genome sequencing for accelerated etiologic diagnosis in critically ill infants. NPJ Genom Med. 2018;3:6.
Mestek-Boukhibar L, Clement E, Jones WD, et al. Rapid Paediatric Sequencing (RaPS): comprehensive real-life workflow for rapid diagnosis of critically ill children. J Med Genet. 2018;55:721–728.
Stark Z, Schofield D, Alam K, et al. Prospective comparison of the cost-effectiveness of clinical whole-exome sequencing with that of usual care overwhelmingly supports early use and reimbursement. Genet Med. 2017;19:867–874.
Iglesias A, Anyane-Yeboa K, Wynn J, et al. The usefulness of whole-exome sequencing in routine clinical practice. Genet Med. 2014;16:922–931.
Rexach J, Lee H, Martinez-Agosto JA, Nemeth AH, Fogel BL. Clinical application of next-generation sequencing to the practice of neurology. Lancet Neurol. 2019;18:492–503.
Jelin AC, Vora N. Whole exome sequencing: applications in prenatal genetics. Obstet Gynecol Clin North Am. 2018;45:69–81.
Centers for Disease Control and Prevention (CDC). Update on overall prevalence of major birth defects--Atlanta, Georgia, 1978–2005. MMWR Morb Mortal Wkly Rep. 2008;57:1–5.
Lord J, McMullan DJ, Eberhardt RY, et al. Prenatal exome sequencing analysis in fetal structural anomalies detected by ultrasonography (PAGE): a cohort study. Lancet. 2019;393:747–757.
Petrovski S, Aggarwal V, Giordano JL, et al. Whole-exome sequencing in the evaluation of fetal structural anomalies: a prospective cohort study. Lancet. 2019;393:758–767.
Douglas MP, Parker SL, Trosman JR, Slavotinek AM, Phillips KA. Private payer coverage policies for exome sequencing (ES) in pediatric patients: trends over time and analysis of evidence cited. Genet Med. 2019;21:152–160.
Deverka PA, Kaufman D, McGuire AL. Overcoming the reimbursement barriers for clinical sequencing. JAMA. 2014;312:1857–1858.
United States Census Bureau. Health insurance coverage in the United States: 2017. https://www.census.gov/library/publications/2018/demo/p60-264.html. Accessed 15 July 2019.
Amendola LM, Berg JS, Horowitz CR, et al. The Clinical Sequencing Evidence-Generating Research Consortium: integrating genomic sequencing in diverse and medically underserved populations. Am J Hum Genet. 2018;103:319–327.
Trosman JR, Van Bebber SL, Phillips KA. Coverage policy development for personalized medicine: private payer perspectives on developing policy for the 21-gene assay. J Oncol Pract. 2010;6:238–242.
Trosman JR, Weldon CB, Kelley RK, Phillips KA. Challenges of coverage policy development for next-generation tumor sequencing panels: experts and payers weigh in. J Natl Compr Canc Netw. 2015;13:311–318.
Trosman JR, Weldon CB, Douglas MP, et al. Payer coverage for hereditary cancer panels: barriers, opportunities, and implications for the Precision Medicine Initiative. J Natl Compr Canc Netw. 2017;15:219–228.
Pezalla EJ. Payer view of personalized medicine. Am J Health Syst Pharm. 2016;73:2007–2012.
Ritchie J, Lewis J. Qualitative research practice: a guide for social science students and researchers. Thousand Oaks, CA: Sage Publications; 2003.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117.
UCSF Center for Translational and Policy Research onPersonalized Medicine (TRANSPERS). Evidence and reimbursement for personalized medicine program. https://pharm.ucsf.edu/transpers/grants-programs/evidence-reimbursement. Accessed 15 July 2019.
Grosse SD, Khoury MJ. What is the clinical utility of genetic testing? Genet Med. 2006;8:448–450.
Burke W, Laberge AM, Press N. Debating clinical utility. Public Health Genomics. 2010;13:215–223.
ACMG Board of Directors. Clinical utility of genetic and genomic services: a position statement of the American College of Medical Genetics and Genomics. Genet Med. 2015;17:505–507.
Keeling NJ, Rosenthal MM, West-Strum D, Patel AS, Haidar CE, Hoffman JM. Preemptive pharmacogenetic testing: exploring the knowledge and perspectives of US payers. Genet Med. 2019;21:1224–1232.
Joseph L, Cankovic M, Caughron S, et al. The spectrum of clinical utilities in molecular pathology testing procedures for inherited conditions and cancer: a report of the Association for Molecular Pathology. J Mol Diagn. 2016;18:605–619.
Clinical Sequencing Evidence-Generating Research (CSER). Prenatal and Pediatric Genome Sequencing (P3EGS). https://cser-consortium.org/projects/4073. Accessed 30 July 2019.
National Human Genome Research Institute. Clinical Sequencing Evidence-Generating Research (CSER). https://www.genome.gov/Funded-Programs-Projects/Clinical-Sequencing-Evidence-Generating-Research-CSER2. Accessed 10 July 2019.
Prokop JW, May T, Strong K, et al. Genome sequencing in the clinic: the past, present, and future of genomic medicine. Physiol Genomics. 2018;50:563–579.
Acknowledgements
This study was funded by grants from the National Human Genome Research Institute (U01 HG009599) and National Cancer Institute (R01 CA221870).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
K.A.P. and M.P.D. receives consulting income from Illumina, Inc., M.E.N. receives grant support from Natera and is a consultant to Invitae. The other authors declare no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Trosman, J.R., Weldon, C.B., Slavotinek, A. et al. Perspectives of US private payers on insurance coverage for pediatric and prenatal exome sequencing: Results of a study from the Program in Prenatal and Pediatric Genomic Sequencing (P3EGS). Genet Med 22, 283–291 (2020). https://doi.org/10.1038/s41436-019-0650-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-019-0650-7
Keywords
This article is cited by
-
Genomic medicine in neonatal care: progress and challenges
European Journal of Human Genetics (2023)
-
Diagnostic yield of pediatric and prenatal exome sequencing in a diverse population
npj Genomic Medicine (2023)
-
The influence of social determinants of health on the genetic diagnostic odyssey: who remains undiagnosed, why, and to what effect?
Pediatric Research (2021)
-
The Medical Genome Initiative: moving whole-genome sequencing for rare disease diagnosis to the clinic
Genome Medicine (2020)
-
Clinical utility of genomic sequencing: a measurement toolkit
npj Genomic Medicine (2020)