Abstract
Purpose
The presentation and etiology of cerebral palsy (CP) are heterogeneous. Diagnostic evaluation can be a prolonged and expensive process that might remain inconclusive. This study aimed to determine the diagnostic yield and impact on management of next-generation sequencing (NGS) in 50 individuals with atypical CP (ACP).
Methods
Patient eligibility criteria included impaired motor function with onset at birth or within the first year of life, and one or more of the following: severe intellectual disability, progressive neurological deterioration, other abnormalities on neurological examination, multiorgan disease, congenital anomalies outside of the central nervous system, an abnormal neurotransmitter profile, family history, brain imaging findings not typical for cerebral palsy. Previous assessment by a neurologist and/or clinical geneticist, including biochemical testing, neuroimaging, and chromosomal microarray, did not yield an etiologic diagnosis.
Results
A precise molecular diagnosis was established in 65% of the 50 patients. We also identified candidate disease genes without a current OMIM disease designation. Targeted intervention was enabled in eight families (~15%).
Conclusion
NGS enabled a molecular diagnosis in ACP cases, ending the diagnostic odyssey, improving genetic counseling and personalized management, all in all enhancing precision medicine practices.
Similar content being viewed by others
INTRODUCTION
With a prevalence of approximately 2–3 in 1000 live births, cerebral palsy (CP) is one of the most common neurological disorders presenting in early childhood. A common definition for CP is “a group of permanent disorders of the development of movement and posture, causing activity limitation, that are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain.” The clinical presentation of CP is complicated by comorbidities including intellectual disability (ID), epilepsy, visual/hearing impairments, autism spectrum disorder, and movement disorders. These additional features contribute to the clinical heterogeneity of CP and make the diagnostic process challenging.
Since the original report by Little in 1861 (refs.1,2), several classification systems have attempted to clarify distinct clinical presentations of CP.3,4,5 Although historically oxygen deprivation causing brain insult has been regarded as a primary etiology, frank brain asphyxia accounts for fewer than 10% of current CP cases.6,7 Efforts to capture motor features and categorize them according to the nature and typology of the motor disorder, anatomical distribution, and functional motor abilities have advanced the understanding and management of individuals with CP.1 It is now generally agreed that CP is an umbrella term for a group of clinically defined conditions.8 These different motor conditions are heterogeneous with respect to etiology, type, severity, and associated features. In spite of this enormous volume of work, some cases of CP cannot be accurately classified in any of the existing etiologic categories.
Several recent studies have helped to clarify the underlying etiology and highlight the substantial contribution of genetic conditions in the etiology of CP.9 Responsible conditions include inborn errors of metabolism (IEM) and rare monogenic conditions which may present as CP. Many IEMs are amenable to treatment, therefore, it is imperative to identify such conditions in a timely fashion.10 Other genetic disorders underlying CP include various monogenic syndromes, and chromosomal and methylation abnormalities.2,9
Exome (ES) and genome sequencing (GS) have accelerated discovery in the genetics of many diseases including neurodevelopmental disorders. ES is a reliable method to identify both novel and known pathogenic rare disease variants.9,11 Deep phenotyping accompanied by ES has yielded diagnostic rates as high as 68–89% in well-characterized cohorts of likely monogenic neurodevelopmental disorders.12 These methods have been successful in CP. Recently, likely pathogenic variants were identified in 9 of 17 cases within eight different genes, demonstrating a diagnostic success rate of 50% (ref. 1313
Our study moves to further resolve and understand the genetic causes of CP. We have applied ES with a semiautomated bioinformatics pipeline in 50 exquisitely phenotyped individuals from 49 families presenting with atypical CP (ACP, meeting criteria as defined below) of unknown etiology, despite clinical genetic and metabolic testing. The diagnostic yield and impact on management of ES for this group of individuals with ACP are discussed.
MATERIALS AND METHODS
Ethics
The study was approved by the Children’s and Women’s Hospital, University of British Columbia Research Ethics Board (#H12-00067), and University of Alberta Ethics Board (HREB B). Each patient or guardian provided informed consent for study participation and subsequent publication of established results.
Patients
Between 2011 and 2016, children and adults meeting the below defined eligibility criteria were consecutively recruited from three tertiary centers in Canada: BC Children’s Hospital in Vancouver and in Edmonton, Glenrose Rehabilitation Hospital, and Stollery Children’s Hospital.
Eligibility criteria
Eligibility criteria were as follows:
-
1.
The participant must have had features associated with loss or impairment of motor function with onset before the age of 1 year and one or more of the following:
-
Severe or profound ID
-
Global developmental delay was ascertained using the Bayley Scales of Infant and Toddler Development (BSID-III third edition), and ID using the Wechsler Preschool and Primary Scale of Intelligence (WIPPSI-IV)
-
Autism spectrum disorder according to the Diagnostic and Statistical Manual of Mental Disorders V (DSM V)
-
Progressive neurological deterioration after the initial clinical confirmation of CP
-
Additional abnormal neurological features (e.g., hemiplegia, diplegia, dyskinesia, ataxia, hypo-/hypertonia, or transient episodic exacerbation of neurological symptoms)
-
Neuroimaging findings: structural abnormalities of the brain not typical for classical cerebral palsy using the existing classification system;14 OR white or gray matter changes that are not characteristic of classical CP (e.g., evidence of brain iron accumulation, atypical white matter lesions); OR a normal brain magnetic resonance image (MRI)
-
Multiorgan disease
-
One or more major congenital anomalies outside the central nervous system
-
An abnormal neurotransmitter metabolite profile or another abnormal biochemical phenotype
-
Positive family history: consanguineous union between the index's parents OR>2 similarly affected siblings; OR a similarly affected parent and child; OR in the case of a male index, one or more similarly affected male relatives related through unaffected female relatives
-
2)
Detailed diagnostic evaluation of the index and family by a neurologist and/or geneticist including biochemical investigations (as outlined in further detail in Dunbar et al.15), neuroimaging, and a chromosomal microarray without identification of an etiology
Next-generation sequencing and bioinformatics analysis and interpretation
Genomic DNA was extracted from peripheral blood using standard techniques. Samples were collected from all available family members. Sample-specific details such as the machine and Library Prep Kit used are found in Table S1. As previously published,12 a semiautomated bioinformatics pipeline was used to process data and prioritize variants. Briefly, raw data was processed using Bowtie2 and Genome Analysis Toolkit (GATK) then variants were called using SAMtools and annotated using SNPEff mode of inheritance specific custom scripts (homozygous recessive, compound heterozygous, hemizygous, and de novo) were used to filter against several databases, including an in-house database of more than 400 samples, ExAC, EVS, and dbSNP. Inheritance specific thresholds were as follows: homozygous and hemizygous (dbSNP, EVS and ExAC = 0.015), compound heterozygous (dbSNP = 0.01, EVS and ExAC = 0.02), and de novo (dbSNP and EVS = 0.0001, ExAC = 0.01). The final step of the variant prioritization was a manual analysis of all remaining variants. Detailed clinical and biochemical information, and family history were collected from the hospital records and supplemented by the clinician who provided hypotheses for the affected pathways and genes, to facilitate bioinformatics analysis. The American College of Medical Genetics and Genomics (ACMG) classifications were applied independently by two separate bioinformaticians and compared. Where differences in classifications were present, additional experts and clinicians were consulted to reach consensus. The term “proposed candidate gene” was used for the five genes not currently associated with an OMIM disease.12,16 The term “secondary variant” was applied to cases with complex phenotypes to describe the non-ACP disease.
RESULTS
Demographics
A total of 49 families with 50 affected individuals (ACP45 contained a pair of affected brothers) were examined. Table 1 lists the major clinical characteristics for all 49 probands; a complete presentation of clinical findings, including details of age, sex, and ethnicity can be found in Table S2. For 31 of the 49 families, NGS via a combination of ES and GS was performed on three family members. In four families, four family members were examined while in the remaining families only the proband (n = 4) or the proband and one other family member (n = 10) were examined.
The majority of ACP probands were male (61%), and 42 patients (86%) were under 19 years of age at enrollment (Table 1). Five cases were the product of a consanguineous union. Approximately half of the families were Caucasian, however, a range of ethnicities were represented across the 49 families. Global developmental delay was confirmed in 8 probands, and ID was present in 37 probands; in 22 probands the ID was in the severe to profound range. The exceptions were the proband (and brother) in family ACP45, as well as the proband of family ACP40, who had normal developmental/cognitive function, and the proband of ACP14 for whom this information was not available.
Clinical features
Additional remarkable clinical and biochemical features are described in Table S2.
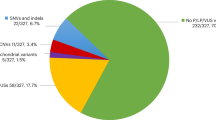
Diagnostic yield and molecular details
A molecular diagnosis was established in 65% of the families (Table. 2). In 28/49 families, the ACP was attributed to a known disease gene(s) and in four cases we propose novel candidate genes that at present lack an associated OMIM disease designation (DGKZ, EPHA4, PALM, PLXNA2). The remaining 35% (n = 17) of cases remain unsolved. Both solved and unsolved cases included families where NGS was performed on one to four family members suggesting that lack of a molecular diagnosis was not due to the unavailability of family members. The majority of variants (37/46 = 80%) in the known and proposed ACP genes were not previously reported in ClinVar. All novel variants reported in this paper have been uploaded to ClinVar (SCV000540926, SCV000540927, SCV000586815–SCV000586858).
Of the monogenic etiologies identified, half (n = 16) segregate with an autosomal dominant inheritance pattern (Table 3). This included one case of imprinted inheritance (ACP26: KANK1), one case of a bialternative mosaic dominant inheritance (ACP20: SPAST)17 and one case of likely parental germline mosaicism resulting in a variant shared between siblings (ACP22: KIDINS220). Two of the three homozygous variants (ACP2: CSTB and ACP31: KMT2C) were identified in known consanguineous families. Only two genes (MECP2 and WDR45) were found in more than one family. All variants were Sanger confirmed in all available family members. Sanger segregation studies were especially useful in eliminating potential variants when multiple siblings were present.
Missense variants were the most common candidate ACP variant observed (n = 28, 67%) followed by stop gains (n = 5, 12%) (Table 4). ACMG classification of all variants was performed and nearly two-thirds were classified as either pathogenic (29%, n = 12) or likely pathogenic (33%, n = 14), while the remaining variants were classified as variants of uncertain significance (VUS; 38%, n = 16) (ref.18). Detailed information for all variants is provided in Table S1.
Proposed candidate genes
We propose four novel candidate genes for ACP, which are not currently assigned an OMIM disease designation (DGKZ, EPHA4, PALM, and PLXNA2). Both autosomal dominant and autosomal recessive inheritance patterns are proposed. Further justification for selection of each gene is provided in the Discussion section. Additional families with variants in these genes are being sought through personal communications and GeneMatcher.org.
Multilocus pathogenic variation results in complex phenotypes
Three patients were found to have two molecular diagnoses, due to variants in two different genes, explaining their complex phenotypes. In ACP31 the MRI and neurodevelopmental features are explained well by two compound heterozygous variants in MED13L. We propose the severe childhood-onset dystonia to be explained by homozygous variants in KMT2C. This is likely an example of an overlapping phenotype, as features of Kleefstra syndrome (617768) are reported in both KMT2C- and MED13L-related conditions. Although ataxia and dysarthria are common, in MED13L, dystonia is not reported. Given its expression pattern and known function, KMT2C is a strong candidate gene for dystonia.19 Moreover, variants in another histone lysine methyltransferase, KMT2B, have recently been reported to cause early-onset dystonia (responsive to deep brain stimulation), further implicating chromatin modifiers in movement disorders.20 Further work must be undertaken to prove an autosomal recessive pattern in MED13L that to date is reported as a dominant disorder, and to clarify the potential role of KMTC2. In ACP8 we propose two distinct phenotypes. The primary phenotype results from a heterozygous de novo in-frame deletion in MeCP2, while biochemical features are due to methionine adenosyltransferase deficiency caused by compound heterozygous missense variants in MAT1A. However, because dystonia is reported in both MeCP2- and MAT1A-related conditions this too is considered an overlapping phenotype. Lastly, in ACP18, variants in two genes, ITPA and NBAS, are proposed to contribute together to this patient’s overlapping and complex ACP phenotype.
Expanded phenotypes
Phenotypic complexity present in four patients was not explained by multilocus variation. We propose expanded phenotypes in known disease genes for ATP1A3 in ACP21 (infantile-onset of chorea dystonia), PAK3 in ACP12 (dopamine responsive automutilation), PLP1 in ACP3 Hypomyelination of Early Myelinating Structures (HEMS phenotype), KCNJ6 in ACP13 with severe hyperkinetic movement disorder, and SCN3A in ACP28 (dystonia in addition to ID and microcephaly).
Targeted interventions
For many families in this study, a molecular diagnosis assisted to end the diagnostic odyssey, improved genetic counseling, and directed access to services and resources in the community (data not shown). Targeted therapeutic interventions aiming to improve clinical features were undertaken in eight families with eight different causal ACP genes (GNAO1, CSTB, GCDH, PAK3, TUBB4A, ATP1A3, RANBP2, and TBCK). Patient ACP1 (GNAO1) had a severe movement disorder phenotype, with multiple prolonged admissions to ICU for dystonic/hyperkinetic crises refractory to pharmacological therapies. These episodes/movements finally responded to deep brain stimulation, as described in other patients with this condition.21,22 In cases ACP2 (CSTB), ACP12 (ref. 23) (PAK3), and ACP15 (TUBB4A) a molecular diagnosis enabled targeted treatment with neurotransmitter supplements. ACP2 has an additional movement disorder, with severe myoclonus and dystonia. Of note, cerebrospinal fluid (CSF) levels of dopamine and serotonin metabolites were significantly lowered, and the movement disorder improved with L-dopa/carbidopa and 5-hydroxytryptophan treatment. Patient ACP15 (TUBB4A) with hypomyelination with atrophy of the basal ganglia and cerebellum (H-ABC) responded favorably to dopamine treatment with a reduction of dystonia and improvement in initiation of motor tasks. ACP12 (PAK3) (ref. 23) presented with severe self-injurious behavior, and low levels of dopamine metabolites in CSF. Self-abusive conduct improved significantly on treatment with low-dose L-dopa/carbidopa and 5-hydroxytryptophan. Molecular diagnosis of glutaric aciduria type I due to biallelic GCDH variants in patient ACP4 allowed for initiation of a lysine- and tryptophan-restricted diet, sick day protocols, and carnitine and thiamine supplementation. Furthermore, molecular diagnosis in ACP23 of RANBP2 deficiency enabled proactive measures to be initiated for possible immune dysregulation (the gene has potential roles in CD8 and immune system function). Because the patient had a history of recurrent upper respiratory tract infections with longer recovery periods, she was referred for further immunological assessment.
DISCUSSION
Classically, CP has been defined based on clinical presentation rather than on underlying etiology. Guidelines for diagnostic assessment in CP do not typically include routine genetic testing; however, genetic evaluation in medicine is rapidly evolving, and novel diagnostic tools in genomic analysis offer remarkable opportunities for a more detailed characterization of the heterogeneous genetic etiology of CP. Approaches including targeted metabolic, tissue, chromosomal microarray, and single-gene/gene panel investigations have been highly successful, particularly in atypical presentations of CP.13 Through applying ES to 49 families with atypical CP (ACP), our work helps broaden the understanding of the complex genetic landscape of CP. Utilizing our proven, multidisciplinary approach with subsequent ES in these patients, we achieved a diagnostic yield of 65%, similar to the diagnostic rate (68%) established in our previous study of unexplained neurometabolic phenotypes.12
These 49 ACP probands represent the second largest exome-based study of CP patients to date; McMichael et al. 9 performed ES in 183 cases, 14% of whom were found to have a potentially CP-causing variant. The higher diagnostic rate in our study can be explained by focused recruitment (strict criteria to augment the likelihood of a genetic condition); exquisite phenotyping; close communication between clinical, laboratory, and bioinformatics team members; and unbiased analysis open to different forms of Mendelian inheritance (including complex forms of dominant inheritance with incomplete penetrance, imprinting, and mosaicism). In addition to the known ACP genes KANK1 and SPAST, this study identified a second family (ACP12) with a PAK3 variant supporting the initial publication by McMichael et al.9 of ACP as a possible PAK3-related phenotype.9 Furthermore, our study highlights the important role of autosomal recessive conditions, with nearly a third (32%) of the variants/genes implicated following this inheritance pattern. The diversity of candidate genes found by different ACP studies highlights that this is a heterogeneous condition both in terms of presentation as well as cause.
We propose four novel candidate genes for ACP (DGKZ, EPHA4, PALM, and PLXNA2) not yet associated with an OMIM-designated disease. The compound heterozygous variants in DGKZ are proposed to account for the complex phenotype reported in ACP30 with severe ID, atrophy of the cerebellum and vermis, microcephaly, and nystagmus. DGKZ, a diacylglycerol kinase, is a critical regulator of intracellular signaling, highly expressed in the hippocampus, cerebellum and retina.24 Murine models of DGKZ deficiency suggest impairment of dendritic spine maintenance and altered synaptic activation status.25 Semitargeted lipidomics analysis is underway to compare the lipidome of the proband’s cells against the lipidome of control cells to look for possible effects on diacylglycerol metabolites. ACP29 (EPHA4) presents with bilateral optic atrophy, spasticity in the lower limbs, and severe ID. EPHA4 has critical roles in the development and guidance of spinal cord axons and visual system development among other functions.26 A model other than haploinsufficiency may have to be involved because this patient does not have the short stature reported in those with contiguous gene deletions involving EPHA4 (ref. 27). Epha4-deficient mouse models demonstrate a unique “hopping gait” overlapping with the lower limb involvement and abnormal gait observed in this patient.28 The paralemmin (PALM) gene encodes a phosphoprotein highly expressed in the brain associated with brain synaptic plasma membranes.29 Studies suggest its role as a regulator of dendritic filopodia and neuronal spine maturation.29,30 We consider PALM as likely candidates for case ACP27 with spastic quadriplegia, dysautonomia, and severe ID because dendritic spine dysgenesis is a recognized feature of multiple neurodevelopmental disorders such as autism, ID, and movement disorders including spastic paraplegia and CP.31 Finally, PLXNA2 is considered a strong candidate in ACP32 presenting with CP and ataxia. Plexins, including Plexin-A2, appear to be signaling receptors for semaphorins in guiding developing axons in both the peripheral and central nervous systems.32 Murine models of PLXNA2 deficiency show abnormal cerebellar morphology, abnormal neuronal migration, with mild ataxia in some.33 Additional functional work is being undertaken to determine the impact on protein function. We seek additional cases with similar phenotypes and/or overlapping gene involvement for further analysis and assessment.
Chromosomal microarrays to detect copy-number variants (CNVs) and mitochondrial DNA (mtDNA) sequencing still have a place in ACP diagnostics; however, NGS is gaining momentum as demonstrated by the recent establishment of the International Cerebral Palsy Genomics Consortium.34 NGS in ACP patients alleviates strain on families, as well as being a cost-effective option for the health-care system;35 and most importantly it facilitates the arrival at a precise molecular diagnosis. For families, a family this provides closure and a better understanding of the disorder for informed decision making. It allows for tailored genetic counseling (reproductive planning, disease inheritance pattern alterations, identification of family members at risk) and potential changes in clinical management along with application of precision medicine practices. These changes include better-informed disease monitoring, treatment initiation and/or discontinuation, as well as investigations into systemic involvement.36 Although our and other studies demonstrate the diagnostic efficacy of ES, this technology is accompanied by various limitations such as less than 100% coverage, and an inability to detect large insertions/deletions, regulatory variants, intron alterations (potential nonexonic regulatory regions) and structural chromosome rearrangements and tandem repeat expansions.36 Furthermore, communication of findings to patients and families can be challenging, with respect to uncertainty (VUS, novel genes, atypical phenotypes, potential for false associations, etc.). Finally, molecular findings of this nature should be screened for by GS and transcriptomics such as demonstrated for mitochondrial and neuromuscular diseases; metabolomics analysis of CSF and other body fluids might well enhance diagnostic yield and provide targets for interventions.37
Our results add to the knowledge on CP by increasing the number of novel human disease genes with this phenotype, and delineation of the phenotypic spectrum of known causal conditions. Furthermore, we demonstrate the additional utility of ES in the characterization of clinically complex phenotypes by allowing resolution of multiple underlying genetic etiologies and phenotypic expansion of reported clinical findings. Multilocus variation, whereby pathogenic variation is present in two or more disease-associated genes, is now recognized as an explanation for some complex phenotypic presentations.38 Three families examined in this study demonstrate either overlapping phenotypes, in which two distinct diseases are present with overlapping features (ACP18, ACP31), or distinct phenotypes when two or more disorders are present without clearly shared features (ACP8) (ref. 39). These three cases (~9%) represent a rate similar to the frequency of multiple molecular diagnoses reported in another large-scale analysis by ES.12,38
ES is instrumental in allowing for recognition and definition of expanded phenotypes in single-gene disorders; however, it can be challenging to distinguish from unidentified multilocus variation.38 It is always possible that a pathogenic variant in a yet unknown disease-causing gene may be responsible for a second disease in these cases. The best way to reduce the likelihood of this possibility is to collect additional unrelated patients with the extended phenotype. Alternatively, Karaca et al.38 demonstrated how the examination of additional affected family members can clarify that suspected phenotype expansion of a single-locus condition is in fact a complex phenotype due to a dual molecular diagnosis, or two genetic conditions.38 We describe unique findings in four cases diagnosed with a known disease, likely broadening the phenotype of these conditions (ACP3, ACP12, ACP21, ACP28), of which three have been published as individual case reports. These complex cases emphasize the power of ES in diagnostics, but also underscore the critical role of the physician in detailed clinical phenotyping and the necessary communication and feedback that must exist between clinician and bioinformatics specialist for an accurate molecular diagnosis.12
References
Rosenbaum P, Paneth N, Leviton A, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109:8–14.
Aisen ML, Kerkovich D, Mast J, et al. Cerebral palsy: clinical care and neurological rehabilitation. Lancet Neurol. 2011;10:844–852.
Mac Keith RC, Keith RCM, Polani PE, Lipmann K, Wheeler DE, Shepherd IDD. Cerebral palsy. Lancet. 1958;271:961–962.
Bax MCO. Terminology and classification of cerebral palsy. Dev Med Child Neurol. 1964;6:295–297.
World Health Organization. International Classification of Functioning, Disability and Health: ICF. World Health Organization; 2001.
Oskoui M, Coutinho F, Dykeman J, Jetté N, Pringsheim T. An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol. 2013;55:509–519.
Moreno-De-Luca A, Andres M-D-L, Ledbetter DH, Martin CL. Genetic insights into the causes and classification of the cerebral palsies. Lancet Neurol. 2012;11:283–292.
Bax M, Goldstein M, Rosenbaum P, et al. Proposed definition and classification of cerebral palsy, April 2005. Dev Med Child Neurol. 2005;47:571–576.
McMichael G, Bainbridge MN, Haan E, et al. Whole-exome sequencing points to considerable genetic heterogeneity of cerebral palsy. Mol Psychiatry. 2015;20:176–182.
Leach EL, Shevell M, Bowden K, Stockler-Ipsiroglu S, van Karnebeek CDM. Treatable inborn errors of metabolism presenting as cerebral palsy mimics: systematic literature review. Orphanet J Rare Dis. 2014;9:197.
Boycott KM, Rath A, Chong JX, et al. International cooperation to enable the diagnosis of all rare genetic diseases. Am J Hum Genet. 2017;100:695–705.
Tarailo-Graovac M, Shyr C, Ross CJ, et al. Exome sequencing and the management of neurometabolic disorders. N Engl J Med. 2016;374:2246–2255.
Takezawa Y, Kikuchi A, Haginoya K, et al. Genomic analysis identifies masqueraders of full-term cerebral palsy. Ann Clin Transl Neurol. 2018;5:538–551.
Himmelmann K, Horber V, De La Cruz J, et al. MRI classification system (MRICS) for children with cerebral palsy: development, reliability, and recommendations. Dev Med Child Neurol. 2017;59:57–64.
Dunbar M, Jaggumantri S, Sargent M, Stockler-Ipsiroglu S, van Karnebeek CDM. Treatment of X-linked creatine transporter (SLC6A8) deficiency: systematic review of the literature and three new cases. Mol Genet Metab. 2014;112:259–274.
De Ligt J, Willemsen MH, Van Bon BWM, et al. Diagnostic exome sequencing in persons with severe intellectual disability. N Engl J Med. 2012;367:1921–1929.
Matthews AM, Tarailo-Graovac M, Price EM, et al. A de novo mosaic mutation in SPAST with two novel alternative alleles and chromosomal copy number variant in a boy with spastic paraplegia and autism spectrum disorder. Eur J Med Genet. 2017;60:548–552.
Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–424.
Shen E, Shulha H, Weng Z, Akbarian S Regulation of histone H3K4 methylation in brain development and disease. Philos Trans R Soc Lond B Biol Sci 2014;369. https://doi.org/10.1098/rstb.2013.0514. Accessed 7 Dec. 2018.
Meyer E, Carss KJ, Rankin J, et al. Mutations in the histone methyltransferase gene KMT2B cause complex early-onset dystonia. Nat Genet. 2017;49:223–237.
Waak M, Mohammad SS, Coman D, et al. GNAO1-related movement disorder with life-threatening exacerbations: movement phenomenology and response to DBS. J Neurol Neurosurg Psychiatry. 2018;89:221–222.
Honey CM, Malhotra AK, Tarailo-Graovac M, van Karnebeek CDM, Horvath G, Sulistyanto A. GNAO1 mutation-induced pediatric dystonic storm rescue with pallidal deep brain stimulation. J Child Neurol. 2018;33:413–416.
Horvath GA, Tarailo-Graovac M, Bartel T, et al. Improvement of self-injury with dopamine and serotonin replacement therapy in a patient with a hemizygous PAK3 mutation: a new therapeutic strategy for neuropsychiatric features of an intellectual disability syndrome. J Child Neurol. 2018;33:106–113.
Rincón E, Gharbi SI, Santos-Mendoza T, Mérida I. Diacylglycerol kinase ζ: at the crossroads of lipid signaling and protein complex organization. Prog Lipid Res. 2012;51:1–10.
Ishisaka M, Hara H. The roles of diacylglycerol kinases in the central nervous system: review of genetic studies in mice. J Pharmacol Sci. 2014;124:336–343.
Flanagan JG, Vanderhaeghen P. The ephrins and Eph receptors in neural development. Annu Rev Neurosci. 1998;21:309–345.
Li C, Chen R, Fan X, et al. EPHA4 haploinsufficiency is responsible for the short stature of a patient with 2q35-q36.2 deletion and Waardenburg syndrome. BMC Med Genet. 2015;16:23.
Leighton PA, Mitchell KJ, Goodrich LV, et al. Defining brain wiring patterns and mechanisms through gene trapping in mice. Nature. 2001;410:174–179.
Kutzleb C, Sanders G, Yamamoto R, et al. Paralemmin, a prenyl-palmitoyl-anchored phosphoprotein abundant in neurons and implicated in plasma membrane dynamics and cell process formation. J Cell Biol. 1998;143:795–813.
Arstikaitis P, Gauthier-Campbell C, Carolina Gutierrez Herrera R, et al. Paralemmin-1, a modulator of filopodia induction is required for spine maturation. Mol Biol Cell. 2008;19:2026–2038.
Bortolato M, Floris G, Shih JC. From aggression to autism: new perspectives on the behavioral sequelae of monoamine oxidase deficiency. J Neural Transm (Vienna). 2018;125:1589–1599.
Yaron A, Huang P-H, Cheng H-J, Tessier-Lavigne M. Differential requirement for Plexin-A3 and -A4 in mediating responses of sensory and sympathetic neurons to distinct class 3 Semaphorins. Neuron. 2005;45:513–523.
Smith CL, Blake JA, Kadin JA, Richardson JE, Bult CJ, Mouse Genome Database Group. Mouse Genome Database (MGD)-2018: knowledgebase for the laboratory mouse. Nucleic Acids Res. 2017;46(D1):D836–D842.
MacLennan AH, Kruer MC, Baynam G, et al. Cerebral palsy and genomics: an international consortium. Dev Med Child Neurol. 2018;60:209–210.
Centers for Disease Control and Prevention (CDC). Economic costs associated with mental retardation, cerebral palsy, hearing loss, and vision impairment—United States, 2003. MMWR Morb Mortal Wkly Rep. 2004;53:57–59.
Srivastava S, Siddharth S, Cohen JS, et al. Clinical whole exome sequencing in child neurology practice. Ann Neurol. 2014;76:473–483.
van Karnebeek CDM, Wortmann SB, Tarailo-Graovac M, et al. The role of the clinician in the multi-omics era: are you ready? J Inherit Metab Dis. 2018;41:571–582.
Karaca E, Posey JE, Coban Akdemir Z, et al. Phenotypic expansion illuminates multilocus pathogenic variation. Genet Med. 2018 Apr 26; https://doi.org/10.1038/gim.2018.33 [Epub ahead of print].
Theunissen TEJ, Sallevelt SCEH, Hellebrekers DMEI, et al. Rapid resolution of blended or composite multigenic disease in infants by whole-exome sequencing. J Pediatr. 2017;182:371–374.e2.
Acknowledgements
We would like to thank the patients and families for participation in this study, and their local physicians and health care teams for providing us the medical reports. We are grateful to X. Han, F. Miao, and M. Higginson for DNA extraction, triplet repeat primed polymerase chain reaction (TP-PCR), and Sanger sequencing; and to E. Lomba, A. Ghani, L. Muttumacoroe, and D. Pak for patient enrollment, study administration, and logistic support.
This work was supported by funding from the B.C. Children’s Hospital Foundation (1st Collaborative Area of Innovation), Neurodevnet (Strategic Opportunity Fund to C.D.v.K., S.S.), Glenrose Rehabilitation Hospital Foundation, the Canadian Institutes of Health Research (grant number 301221), the National Ataxia Foundation, and the Rare Diseases Foundation. Informatics infrastructure was supported by Genome BC and Genome Canada (ABC4DE Project). C.D.v.K. and C.J.R. are recipients of the Michael Smith Foundation for Health Research Scholar Award. C.D.v.K. received a salary award from Stichting Metakids. A.M.M. received stipends from the BC Children’s Research Institute as postdoctoral fellow; B.D. received stipends from the Canadian Institutes of Health Research Drug Safety and Effectiveness Cross-Disciplinary Training Program (CIHR-DSECT), CIHR, and the Michael Smith Foundation for Health Research during the period of this study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosure
The authors declare no conflicts of interest.
Additional information
Senior co-authors:Helly Goez and Clara D. van Karnebeek.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Matthews, A.M., Blydt-Hansen, I., Al-Jabri, B. et al. Atypical cerebral palsy: genomics analysis enables precision medicine. Genet Med 21, 1621–1628 (2019). https://doi.org/10.1038/s41436-018-0376-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-018-0376-y
Keywords
This article is cited by
-
Redefining cerebral palsies as a diverse group of neurodevelopmental disorders with genetic aetiology
Nature Reviews Neurology (2023)
-
Integrative Multi-Omics Research in Cerebral Palsy: Current Progress and Future Prospects
Neurochemical Research (2023)
-
Secondary biogenic amine deficiencies: genetic etiology, therapeutic interventions, and clinical effects
neurogenetics (2021)