Abstract
Purpose
Family studies are an important but underreported source of information for reclassification of variants of uncertain significance (VUS). We evaluated outcomes of a patient-driven framework that offered familial VUS reclassification analysis to any adult with any clinically ascertained VUS from any laboratory in the United States.
Methods
With guidance from FindMyVariant.org, participants recruited their own relatives for study participation. We genotyped relatives, calculated quantitative cosegregation likelihood ratios, and evaluated variant classifications using Tavtigian’s unified framework for Bayesian analysis with American College of Medical Genetics and Genomics/Association for Molecular Pathology (ACMG/AMP) criteria. We report participation and VUS reclassification rates from the 50 families enrolled for at least one year and reclassification results for 112 variants from the larger 92-family cohort.
Results
For the 50-family cohort, 6.7 relatives per family were invited to participate and 67% of relatives returned samples for genotyping. Sixty-one percent of VUS were reclassified, 84% of which were classified as benign or likely benign. Genotyping relatives identified a de novo variant, phase variants, and relatives with phenotypes highly specific for or incompatible with specific classifications.
Conclusions
Motivated families can contribute to successful VUS reclassification at substantially higher rates than those previously published. Clinical laboratories could consider offering family studies to all patients with VUS.
Similar content being viewed by others
Introduction
The increased use of next-generation sequencing has led clinical laboratories to report greater numbers of rare, family-specific variants of uncertain clinical significance (VUS).1 As clinical genetic testing shifts from diagnostic to predictive use, reported genetic variants can impact management recommendations at earlier ages.2 Previous studies have shown that the majority of VUS are reclassified as benign,1,3,4,5 and current guidelines recommend that physicians disregard VUS results for risk assessment and manage patients using only clinical and family history.6,7,8 However, physicians have a varied understanding of VUS, and some may still make familial testing and surgical management recommendations as if the VUS are pathogenic.5,9,10,11 Additionally, patients who receive VUS results may perceive their VUS as pathogenic, which may increase anxiety and fear that can influence screening and surgical decisions.3,4,12,13,14,15 Reclassification of VUS may improve psychological outcomes, improve risk assessment, and promote appropriate medical management, including variant-specific cascade testing for relatives and optimal screening plans for at-risk individuals.4,5,11
Family studies are an important source of information for variant classification. Families are typically the most efficient way to ascertain clinical data about VUS, which tend to be rare in the general population.16,17,18 Statistical approaches for cosegregation analysis, or determination if a disease occurs with a variant more often than expected by chance in a family, have been described.19,20,21 Families may also yield allelic information, inform de novo variants, and generate unbiased observation of variant effect if relatives are not preferentially sampled based on phenotype.22
VUS reclassification through family studies is currently available for selected, high-impact families. Although many laboratories report offering family studies for VUS reclassification, current family studies at most commercial laboratories have many barriers to entry, including application processes and potential fees for participation.23 Eligibility for family studies is typically limited by availability of affected relatives or laboratory interest in specific genes or variants. Although many research manuscripts and case studies report on selected families, commercial laboratories rarely publish family study methodologies or deposit results from individual family studies into public databases like ClinVar.24 Only one report about the process and outcomes of family studies for VUS reclassification is available.25 Hence, community-wide outcomes such as variant reclassification results, patient satisfaction, and participation metrics like drop-out rates and number of participating relatives are not clear.
To address growing interest in VUS reclassification,1,26,27 we developed a patient-driven framework for family studies for clinically ascertained VUS. Patient-driven research allows patients to actively inform their own health care by contributing data to research studies that align with patient goals and values and clinical outcomes.28,29 We offered sequencing, statistical cosegregation, and VUS reclassification analysis to any interested adult who had received a VUS through clinical testing at any laboratory in the United States. To assist families with the patient-driven study process, we created an online tutorial (FindMyVariant.org)23,30 that showed probands how to recruit their own relatives, coordinate communication within their families, and gather family history to build pedigrees. We present the outcomes of variant reclassification efforts for 112 variants from 92 families who enrolled over a period of 28 months. We document the success rate of patient-driven family recruitment, as well as the wide variety of variant reclassification pathways that arose for participating families.
Materials and methods
Study participants
Eligible participants were English-speaking adults in the United States with any clinically classified VUS in a gene with a well-defined disease phenotype. Proband exclusion criteria included being under the age of 18, having no phone number or email address, and not reading, writing, or speaking English.
Potential participants received study contact information from clinical genetics providers, a study announcement on the Facing Our Risk of Cancer Empowered (FORCE) online message board, word of mouth, patient forums, and Internet searches that turned up the study website. After a potential participant initially contacted the study by email or phone, study staff reached out by phone to answer questions and explain study steps and basic cosegregation analysis, and to discuss the proband’s responsibility to ask relatives to participate in the study (see Supplementary Materials and Methods). Study staff asked each proband to go through materials on FindMyVariant.org for more detailed explanations and examples of family studies for VUS classification.
Participant education using FindMyVariant.org
The FindMyVariant.org website23,30 is a publicly available online tutorial designed to educate individuals about the meaning of VUS and assist individuals in pursuing family studies for VUS reclassification through clinical and research laboratories. The site provides resources such as email templates for approaching relatives with the topic of family studies for VUS reclassification and hypothetical examples of families pursuing family studies for VUS reclassification. While participants anecdotally mentioned using the website to assist with family member recruitment, formal data on participant website usage was not collected.
Patient-driven participation, recruitment, and coordination of samples
Probands conducted and coordinated the recruitment and participation of other family members. They gathered family history information from relatives to expand and clarify their pedigree, and they also communicated the study aims to their relatives and gauged relatives’ interest in providing information and a sample to the study. Relatives contacted study staff directly by phone or email or passed their contact information to study staff through the proband. Study staff sent Oragene OGR-500 saliva kits, consent forms, and return postage directly to each proband’s and each relative’s residence and stored each individual’s contact information in the REDCap database.31
Family member recruitment was an iterative process. After establishing a proband’s sample as a positive control, the proband’s parents and siblings were tested first if available; if not, other close relatives were tested. VUS status results from these relatives often informed which additional relatives were next recruited and tested as the pattern of VUS inheritance became clear. Probands consulted with study staff via phone and email about potential informativeness of relatives, but the exact pattern of testing varied and was decided by probands.
We designed study protocols to minimize the potential for coercion of relatives to participate in the study. Each proband and relative individually provided written informed consent regarding the use of his/her saliva sample and genetic data. Relatives could choose for the study to disclose VUS status results to themselves and/or the proband, or to keep the VUS status results undisclosed. Consent forms were available for relatives in English and Spanish.
Study staff requested tumor samples from various pathology laboratories after receiving appropriate documentation from the individual or legal representative, including documentation of identity or of next-of-kin relationship to a deceased individual and written permission for the study to request a specific tumor sample. Information on genotyping and sequencing of saliva and tumor samples is in Supplementary Materials and Methods.
During enrollment and at multiple times during the study, probands were informed that they had ownership of their personal variant classification activities. Probands could consult study staff to discuss next steps and the likelihood of gaining information about a variant by genotyping additional relatives; delegate any or all study activities to a relative or other surrogate; and pause or end their participation at any point without justification. If a proband or surrogate had not contacted the study in at least three months, study staff attempted to contact the individual to ascertain interest in the study. After three attempts at contact without response, the family was put on administrative pause and not recontacted.
Results disclosure
The study genetic counselor returned VUS status results (positive or negative for each VUS) to each individual by phone and email if requested (see example text in Supplementary Materials and Methods). Probands and relatives who tested positive for a reclassified likely pathogenic or pathogenic variant through the study received individual written reclassification reports and genetic counseling by phone. For likely benign or benign variants, only the proband received a written reclassification report and genetic counseling; relatives received written reports and counseling upon request. If a VUS was not reclassified when a proband decided to stop study efforts, no written report was issued, but probands received genetic counseling during their exit discussion. Due to inherent statistical limitations of variant analysis, nearly all reclassification reports included a disclaimer stating that this study could not rule out low-level risk (less than approximately twofold disease risk).
Cosegregation analysis
We used the publicly available cosegregation analysis web tool Analyze.MyVariant.org, which we developed,36 to calculate cosegregation likelihood ratios18 for variants in the following genes: ATM, BRCA1, BRCA2, CHEK2, MEN1, MLH1, MSH2 (with EPCAM), MSH6, and PMS2. We used the Analyze.MyVariant.org backend software and developed penetrance matrixes from published literature for additional genes (BRIP1, ENG, RAD51C, and TP53). 19 Although we welcomed clinical documentation of phenotypes, self-reported phenotype was the norm. When a thorough laboratory or clinical workup such as specific laboratory testing, targeted physical examination, or colonoscopy was necessary to diagnose a phenotype, we considered all individuals who did not report having the required clinical workup as having unknown phenotypes. For example, in family 1014 and 1091 we considered all individuals under 50 without documented MEN1 workups to have unknown phenotype.
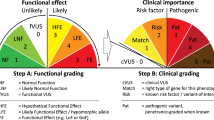
VUS reclassification
During the study, we used International Association of Cancer Registries (IARC) guidelines for Bayesian variant classification32 when quantitative analysis was possible and American College of Medical Genetics and Genomics/Association for Molecular Pathology (ACMG/AMP) 2015 guidelines6 for rule-based classification when quantitative analysis was not feasible. VUS were analyzed iteratively over a two-year period from February 2016 to May 2018 as new information was acquired. For this manuscript, we reevaluated all classifications using Tavtigian’s unified framework, which facilitates combining Bayesian analysis with ACMG/AMP guidelines.33 We considered absence from population databases (ExAC and/or gnomAD browsers)34 to be supporting rather than moderate evidence for pathogenicity, as most yet-to-be-observed extremely rare variants in the genes evaluated are predicted to be benign.1,3,9,34 For VUS in MLH1, MSH2, and MSH6, we used the computational prior from Thompson’s study.35 For other genes we used 0.19 as a prior probability because this was the proportion of variants we observed as pathogenic/likely pathogenic in our study. This is near the center of the permissible range suggested by Tavtigian and colleagues.36 Because defining the prior with the existing study data is somewhat circular, we performed sensitivity analysis for the prior by evaluating variants using priors of 0.1 and 0.32, at the extremes of the permissible range.33 We also assessed computational data using the Polyphen-2, SIFT, and Align-GVGD programs.37,38,39
Evaluation of sources of information about VUS reclassification
We tabulated sources of variant information gathered during the course of this study. Categories of information included publicly available population frequency,34 computational37,38,39 and functional data, as well as information available from careful analysis of clinical and genetic information of family members such as quantitative cosegregation,19,36 qualitative phenotype assessment, and parent-of-origin data including de novo status, maternal or paternal inheritance for imprinted genes, and haplotype information (Table 2, Table S1). Information was also available from other laboratories, from clinical variant databases at the University of Washington Department of Laboratory Medicine, or from ancillary functional analysis by collaborating researchers. Several detailed examples of specific variant classification pathways are presented as Supplementary Data. See Table S1 for variant-specific references and analysis.
Outcomes and VUS reclassification rates
VUS reclassification was the major outcome of this observational study. Because each reclassification pathway was unique, quantitative summaries of this outcome are problematic. Appropriate denominators are difficult to assign because some families enrolled recently and others are still involved in variant reclassification activities more than two years after enrollment. To describe the variety of outcomes, we plotted a summary of each family’s variant classification pathway (Fig. 1). We also evaluated classification as an outcome using a variety of descriptive statistics: (1) proportion of variants reclassified for probands enrolled for at least 12 months in the study, (2) median length of time from enrollment until reclassification, (3) number of relatives enrolled and submitting samples per family, and (4) proportion of variants reclassified in low or moderate penetrance genes versus high penetrance genes. Because some recently enrolled participants had not yet contacted many relatives, we reported outcomes for those involved in the study for at least one year and for the entire study cohort separately.
This study was approved by the University of Washington Institutional Review Board (#50616). All personal demographic, health, and genetic information available to the study was kept confidential unless explicit permission was given to share information.
Results
Study sample
Demographics
One hundred and eight self-selected participants who contacted the study between the beginning of February 2016 and the end of March 2018 were sent study materials. Of these, 92 completed the consent process and enrolled in the study. Demographic data of enrolled participants were obtained by self-report and are listed in Table 1. All 92 enrolled participants reported ancestry, gender, and birth date. Eighty-six enrolled participants reported additional demographic information such as marital status, parenthood status, education level, insurance status, and household income (Table 1). While most participants chose to lead recruitment and coordinate sample collection for their families, six participants (7%) delegated the study tasks to a relative surrogate with more time and/or interest. Ninety-one participants provided their original genetic testing report; most variants (90%) were reported after the public releases of the ClinVar and ExAC databases (Table 1). Almost all participants had VUS in cancer risk genes (Table S1).
Patient-driven family recruitment
Across 92 families, the total number of relatives invited was 500 (5.4 per proband) and the total number of samples returned by relatives was 347 (69% of invited relatives). The median number of relatives invited per proband was 4 (range 0 to 21) and the median number enrolled per proband was 3 relatives (range 0 to 14). There is a clear pattern of relative enrollment 2 weeks to 6 months after proband enrollment, with 82% of all relatives enrolling in this early time period. The timing of subsequent phases of relative enrollment varied between families (Fig. 1). Tumor samples from deceased relatives were also counted as enrolled relatives.
Variant study pathway and outcomes
For 50 probands who were enrolled in the study for at least one year, 335 relatives were invited to participate (mean 6.7 per proband) and 223 returned samples (67%). Of 62 variants, 38 were reclassified (61%), with 32 reclassified as benign/likely benign (84%) and 6 reclassified as pathogenic/likely pathogenic (16%). For those enrolled at least one year, 9 probands decided to end their participation with one or more variants still classified as a VUS and 3 probands were put on administrative pause after they did not respond to study contact attempts (Fig. 1).
A total of 112 variants were analyzed from February 2016 to May 2018. Fifty-six variants (50%) were reclassified (Table S1, Fig. 2). Reclassifications took a median of 298 days with a minimum of 8 days (Fig. 1). Classifications changed to pathogenic (n = 6, 11%), likely pathogenic (n = 5, 9%), likely benign (n = 39, 70%), and benign (n = 6, 11%) (Table S1, Fig. 2). Of 56 reclassified variants, 41 (73%) were considered to have high penetrance for a specific phenotype and 15 (27%) had low, moderate, or undefined penetrance (Table S1).
Sources of information about VUS reclassification
Public data were the most common source of information contributing to variant analysis (Table 2). Population data34 were informative for 62 variants (55%). Computational information37,38,39 was informative for 95 variants (85%). Functional studies contributed to assessment of 10 variants (9%). Public data from literature and public databases such as ClinVar24 aided in assessment of 49 variants (44%). Twenty variants (18%) could have been reclassified with only public data: 15 as likely benign, 2 as benign, and 3 as likely pathogenic (Table S1).
Family data were necessary to reclassify 29 variants (26%): 21 as likely benign, 3 as benign, 3 as likely pathogenic, and 2 as pathogenic. Family data added to further refinement of classifications for several variants, moving one variant that would have been likely pathogenic to pathogenic and one variant from likely benign to benign. Overall, family data were available and contributed in some form to understanding 93 variants (83%) (Table S1). Quantitative cosegregation analysis was performed for 62 variants (55%), of which 33 provided evidence for pathogenicity and 29 provided evidence against pathogenicity (Table S1). This evidence provided from cosegregation analysis was similar to the evidence expected based on simulation studies of three-generation families.40
In addition to quantitative cosegregation, detailed family analysis revealed several other sources of information (Table 2, Table S1). Qualitative phenotype assessment in relatives contributed evidence for 27 variants (24%) when quantitative cosegregation was not available. We sometimes considered this qualitative information to be moderate or strong evidence (e.g., individuals in their 80s with no polyps on colonoscopy indicate that an APC variant is unlikely to cause clinically actionable risk of polyposis). However, qualitative assessments are more subjective than cosegregation calculations. Parent-of-origin information helped classify three variants (3%). Tumor data were available from six relatives (5%). Other information such as molecular phenotype of tumors and allelic information in relatives contributed to variant assessment in ten families (9%).
For a subset of cases (n = 31, 28%), we also utilized information from our analysis of the proband’s variant that was independent of family data and not publicly available. This data included proband tumor and molecular phenotype data (7 variants), RNA analysis (5 variants), evaluation of our database of patients tested at the University of Washington or communications with other clinical laboratories (8 variants), and cases where a different variant explained the phenotype (11 variants) (Table 2, Table S1).
Discussion
We have shown that with active participation, it is possible to classify a meaningful proportion of VUS in a relatively small timeframe. One study on VUS reclassification in BRCA1 and BRCA2 reports offering testing to 2.3 relatives per proband and receiving responses from a quarter of those invited (0.55 genotyped individuals per proband).25 In contrast, we offered testing for VUS in any gene with a well-defined phenotype to an unlimited number of relatives at risk of having the variant, although probands often consulted study staff about who to test next. For families participating in our study for over one year, 6.7 relatives were invited by the proband per family and 67% of relatives returned samples (4.5 genotyped individuals per proband). This response rate contributed to reclassification of 61% of VUS. We did not perform a controlled comparison, so we cannot fully explain the observed eightfold increase in participation over past published studies. However, these results suggest that active patient participation may improve family member enrollment compared with previously published protocols for family studies of VUS. Additionally, our enrollment strategy is likely to have enriched for motivated patients with VUS in autosomal dominant cancer risk genes. It is possible that these families were more motivated to clarify VUS due to the availability of medical management recommendations and clinical genetic testing. It is also possible that there is lower stigma for cancer risk compared with other conditions. These factors, among others, may bias the rates of family participation and VUS reclassification in our study.
Family cosegregation analysis is an effective way to generate evidence supporting benign classification. About 80% of VUS reclassified in this study were benign or likely benign. VUS in genes that have lower penetrance result in lower likelihood ratios on cosegregation analysis and are less likely to be classified than VUS in genes known to have higher penetrance.36,40 We generated cosegregation evidence for 11 VUS in ATM and CHEK2, but we were only able to reclassify VUS in these two genes when functional data were available (Table S1). Because of this limitation, we included a disclaimer on nearly every reclassification report stating that this study could not rule out low-level risk (less than approximately twofold risk). Similarly, current models of cosegregation analysis require an assumed penetrance, which can be a limitation for hypomorphic variants. For example, with TP53 VUS we used penetrance estimates from the Li–Fraumeni literature. Reports for non-Li–Fraumeni TP53 variants were nuanced, indicating that the family analysis was not consistent with a Li–Fraumeni syndrome variant, but that substantially elevated cancer risk could not be ruled out (see Table S1).
While quantitative cosegregation data were valuable in many cases (55%), we were surprised to find that additional data to reclassify VUS were present in many families. Family data unexpectedly revealed de novo events (family 1082) and phase variants (family 1075 and 1085) and showed patterns consistent or inconsistent with imprinting (family 1011) (see Supplementary Data and Table S1). Family-based genotyping also identified relatives with phenotypes either highly specific (family 1091) or incompatible with the variant in question (family 1077) (see Supplementary Data and Table S1). These all provided information above and beyond the information that was available from quantitative cosegregation. Occasionally we uncovered a surprising amount of meaningful information from a small number of individuals or with minimal effort. For example, we found that nine individuals in family 1107 had received clinical variant testing from at least two different laboratories and that immunohistochemical (IHC) data were available for three tumors (see Supplementary Data). For this family, variant analysis was rapid (Fig. 1) and receiving consent forms was the limiting factor.
One major limitation of this study was self-selection. Participants in this study were predominantly educated white women with relatively high income. The patient-driven approach may or may not be as successful in other demographic groups. However, self-selection and a personal desire for information may be a larger factor than race, gender, or socioeconomic status with regard to participation. We did not note differences in relative participation rate with regard to these factors, but our sample was too small to analyze this systematically. A more diverse cohort of self-selected individuals may yield a richer data set. Another limitation is the self-reporting of clinical phenotypes. This limitation may have had minimal impact on analysis of variants in genes that lead to obvious diagnoses such as breast cancer, but may have had a greater impact in genes where phenotypes are more difficult to diagnose, such as MEN1 and COL3A1.
Previous studies in cancer and cardiac settings have shown that patient-driven research can positively affect treatment outcomes and improve clinical assessments.28,29 Our findings suggest that broader use of patient-driven family studies may be an effective way to shorten the time and increase the rate of VUS reclassification. One clinic observed that 44% of breast cancer patients received a VUS reclassification anywhere from 0 to 9 years after initial testing.3 Another reported that 56% of VUS were reclassified after a median of 39 months.15 Another found that 11% of VUS were reclassified at the end of approximately 4 years of follow up.9 In contrast, our patient-driven framework for family studies resulted in reclassification of approximately 60% of variants after at least one year of study enrollment. These results are promising, although some of these differences may be due to our research thresholds for reclassification being lower than those of clinical laboratories.
Given access to familial testing and educational materials, motivated families can contribute valuable and often elusive information to successful VUS reclassification even with limited family size. As family analysis can contribute information supporting both benign and pathogenic classifications, laboratories may consider expanding the availability of family studies for VUS reclassification and more systematically include unaffected relatives in genetic assessments and analyses. Although more work is needed, our study illustrates that active engagement of families in genetic follow up of family-specific variants may be an ideal example of personalized, participatory genomic medicine.
References
Shirts BH, Pritchard CC, Walsh T. Family-specific variants and the limits of human genetics. Trends Mol Med. 2016;22:925–934.
Moreno L, Linossi C, Esteban I, et al. Germline BRCA testing is moving from cancer risk assessment to a predictive biomarker for targeting cancer therapeutics. Clin Transl Oncol.2016;18:981–987.
Murray ML, Cerrato F, Bennett RL, Jarvik GP. Follow-up of carriers of BRCA1 and BRCA2 variants of unknown significance: variant reclassification and surgical decisions. Genet Med. 2011;13:998–1005.
Welsh JL, Hoskin TL, Day CN, et al. Clinical decision-making in patients with variant of uncertain significance in BRCA1 or BRCA2 genes. Ann Surg Oncol.2017;24:3067–3072.
Macklin SK, Jackson JL, Atwal PS, Hines SL. Physician interpretation of variants of uncertain significance. Fam Cancer. 2018 May 2; https://doi.org/10.1007/s10689-018-0086-2[Epub ahead of print].
Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med.2015;5:30.
National Cancer Comprehensive Network. Genetic/familial high risk assessment: colorectal version 3.2017. 2017. http://www.nccn.org. Accessed 11 May 2018.
National Cancer Comprehensive Network. Genetic/familial high risk assessment: breast and ovarian version 1.2018. 2017. http://www.nccn.org. Accessed 11 May 2018.
Macklin S, Durand N, Atwal P, Hines S. Observed frequency and challenges of variant reclassification in a hereditary cancer clinic. Genet Med. 2018;20:346–350.
Petrucelli N, Lazebnik N, Huelsman KM, Lazebnik RS. Clinical interpretation and recommendations for patients with a variant of uncertain significance in BRCA1 or BRCA2: a survey of genetic counseling practice. Genet Test. 2002;6:107–113.
Eccles BK, Copson E, Maishman T, Abraham JE, Eccles DM. Understanding of BRCA VUS genetic results by breast cancer specialists. BMC Cancer. 2015;15:936.
Culver JO, Brinkerhoff CD, Clague J, et al. Variants of uncertain significance in BRCA testing: evaluation of surgical decisions, risk perception, and cancer distress. Clin Genet. 2013;84:464–472.
van Dijk S, van Asperen CJ, Jacobi CE, et al. Variants of uncertain clinical significance as a result of BRCA1/2 testing: impact of an ambiguous breast cancer risk message. Genet Test. 2004;8:235–239.
Vos J, Otten W, van Asperen C, Jansen A, Menko F, Tibben A. The counsellees’ view of an unclassified variant in BRCA1/2: recall, interpretation, and impact on life. Psychooncology.2008;17:822–830.
Garcia C, Lyon L, Littell RD, Powell CB. Comparison of risk management strategies between women testing positive for a BRCA variant of unknown significance and women with known BRCA deleterious mutations. Genet Med.2014;16:896–902.
Teng J, Risch N. The relative power of family-based and case-control designs for linkage disequilibrium studies of complex human diseases. II. Individual genotyping. Genome Res. 1999;9:234–241.
Thornton T, McPeek MS. Case-control association testing with related individuals: a more powerful quasi-likelihood score test. Am J Hum Genet.2007;81:321–337.
Shirts BH, Jacobson A, Jarvik GP, Browning BL. Large numbers of individuals are required to classify and define risk for rare variants in known cancer risk genes. Genet Med.2013;19:187.
Thompson D, Easton DF, Goldgar DE. A full-likelihood method for the evaluation of causality of sequence variants from family data. Am J Hum Genet. 2003;73:652–655.
Mohammadi L, Vreeswijk MP, Oldenburg R, et al. A simple method for co-segregation analysis to evaluate the pathogenicity of unclassified variants; BRCA1 and BRCA2 as an example. BMC Cancer.2009;9:211.
Jarvik GP, Browning BL. Consideration of cosegregation in the pathogenicity classification of genomic variants. Am J Hum Genet. 2016;98:1077–1081.
Gong G, Hannon N, Whittemore AS. Estimating gene penetrance from family data. Genet Epidemiol.2010;34:373–381.
Garrett LT, Hickman N, Jacobson A, et al. Family studies for classification of variants of uncertain classification: current laboratory clinical practice and a new web-based educational tool. J Genet Couns. 2016;25:1146–1156.
Landrum MJ, Lee JM, Riley GR, et al. ClinVar: public archive of relationships among sequence variation and human phenotype. Nucleic Acids Res.2014;42 Database issue:D980–985.
Eggington JM, Bowles KR, Moyes K, et al. A comprehensive laboratory-based program for classification of variants of uncertain significance in hereditary cancer genes. Clin Genet.2014;86:229–237.
Ramos E, Weissman SM. The dawn of consumer-directed testing. Am J Med Genet C Semin Med Genet.2018;178:89–97.
Solomon I, Harrington E, Hooker G, et al. Lynch syndrome limbo: patient understanding of variants of uncertain significance. J Genet Couns. 2017;26:866–877.
Xian Y, O’Brien EC, Fonarow GC, et al. Patient-centered research into outcomes stroke patients prefer and effectiveness research: implementing the patient-driven research paradigm to aid decision making in stroke care. Am Heart J.2015;170:36–45.
Barocas DA, Alvarez J, Resnick MJ, et al. Association between radiation therapy, surgery, or observation for localized prostate cancer and patient-reported outcomes after 3 years. JAMA. 2017;317:1126–1140.
University of Washington. FindMyVariant.org. 2015. https://findmyvariant.org/. Accessed 26 April 2018.
Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381.
Plon SE, Eccles DM, Easton D, et al. Sequence variant classification and reporting: recommendations for improving the interpretation of cancer susceptibility genetic test results. Hum Mutat.2008;29:1282–1291.
Tavtigian SV, Greenblatt MS, Harrison SM, et al. Modeling the ACMG/AMP variant classification guidelines as a Bayesian classification framework. Genet Med. 2018 Jan 4; https://doi.org/10.1038/gim.2017.210[Epub ahead of print].
Lek M, Karczewski KJ, Minikel EV, et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature. 2016;536:285–291.
Thompson BA, Goldgar DE, Paterson C, et al. A multifactorial likelihood model for MMR gene variant classification incorporating probabilities based on sequence bioinformatics and tumor characteristics: a report from the Colon Cancer Family Registry. Hum Mutat.2013;34:200–209.
Rañola JMO, Liu Q, Rosenthal EA, Shirts BH. A comparison of cosegregation analysis methods for the clinical setting. Fam Cancer.2018;17:295–302.
Adzhubei IA, Schmidt S, Peshkin L, et al. A method and server for predicting damaging missense mutations. Nat Methods. 2010;7:248–249.
Ng PC, Henikoff S. SIFT: predicting amino acid changes that affect protein function. Nucleic Acids Res. 2003;31:3812–3814.
Tavtigian SV, Deffenbaugh AM, Yin L, et al. Comprehensive statistical study of 452 BRCA1 missense substitutions with classification of eight recurrent substitutions as neutral. J Med Genet.2006;43:295–305.
Rosenthal EA, Ranola JMO, Shirts BH. Power of pedigree likelihood analysis in extended pedigrees to classify rare variants of uncertain significance in cancer risk genes. Fam Cancer.2017;16:611–620.
Acknowledgements
We thank the many families who participated actively as partners in this work. We also thank the undergraduate students who assisted in genotyping: Kimberly Krupa, Sarah Upham, Yijun Sim, Lisa Williamson, Nela Novákova, and Sarah Helfen. We thank Eric Konnick, Moon Chung, David Fareti, Jailanie Kaganovsky, and Gynevill Villanueva for their assistance in processing samples. This study was supported by grants from the Damon Runyon Cancer Research Foundation (DRR-33-15), the National Human Genome Research Institute (NHGRI) (R21HG008513), and the Fred Hutch/University of Washington Cancer Consortium (NCI 5P30 CA015704-39).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare no conflicts of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Tsai, G.J., Rañola, J.M.O., Smith, C. et al. Outcomes of 92 patient-driven family studies for reclassification of variants of uncertain significance. Genet Med 21, 1435–1442 (2019). https://doi.org/10.1038/s41436-018-0335-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-018-0335-7
Keywords
This article is cited by
-
Stepwise ABC system for classification of any type of genetic variant
European Journal of Human Genetics (2022)
-
Clinical impact of rare variants associated with inherited channelopathies: a 5-year update
Human Genetics (2022)
-
How I faced my prostate cancer: a molecular biologist’s perspective
npj Precision Oncology (2021)
-
Clinical Implications of the Genetic Architecture of Dilated Cardiomyopathy
Current Cardiology Reports (2020)