Abstract
Purpose
The aim of the study was to present the rates of corneal transplant rejection from 2018 to 2022 at both Moorfields Eye Hospital UK, and Ospedali Privati Forli (OPF) “Villa Igea”, Italy and evaluate the purported association between COVID-19 vaccination and rejection.
Methods
We performed a retrospective review of rejection cases presenting to the two units. Monthly rates were correlated against regional vaccination programme rates. At OPF, conditional Poisson regression model was employed to estimate the incidence risk ratio (IRR) of graft rejection following COVID-19 vaccination risk period compared with the control period.
Results
Between January 2018 and March 2022, there were 471 (Moorfields), 95 (OPF) episodes of rejection. From the start of vaccination programme in the UK in late January 2021, the median number of graft rejections per month at Moorfields was 6 (range: 5–9), which was not significantly different to post-lockdown, pre-vaccination programme (March 2020–January 2021), p = 0.367. At OPF, the median rates of rejection before and after initiation of the vaccination programme were not significantly different (p = 0.124). No significant increase in incidence rate of rejection in the risk period following COVID-19 vaccination was found (IRR = 0.53, p = 0.71).
Conclusion
No notable increase in rates of transplant rejection was noted in year 2021 when COVID-19 vaccination was broadly implemented. The apparent temporal relationship between COVID-19 vaccination and corneal graft rejection highlighted in several case reports may not represent a causative association.
Similar content being viewed by others
Introduction
COVID-19 caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has, as of May 2022, resulted in excess of 15 million deaths worldwide, notwithstanding the morbidity burden caused by long term effects of infection and curtailment of personal freedoms imposed on many populations by their national governments in public health measures to restrict the replication of the virus [1].
However, the development of a number of vaccines has led to a reduction in the morbidity and mortality of this novel infection and in many countries have had significant benefits on alleviating pressures on healthcare systems and reducing imposed limitations on personal freedoms. Phase Ill clinical trials from various manufacturers have confirmed the high efficacy of vaccines against serious COVID-19 infection with low incidence rates of major adverse events [2, 3]. However, the relatively limited sample sizes and follow-up durations of phase III clinical trials inherently restrict the ability to detect rare and serious adverse vaccine-associated outcomes.
Since the inception of various nation-based vaccination programmes, ophthalmologists have identified and sought to publish cases of corneal transplant rejection with a temporal association to the SARS-CoV-2 vaccine and many such case reports have been published to date [4,5,6,7,8,9,10,11,12,13,14,15,16]. However, case reports are low level evidence which can be subject to observer, reporting and publication bias. As physicians, we have the duty to offer our patients sound medical advice based on the best available evidence and to not unnecessarily contribute to vaccine hesitancy, if unwarranted.
In order to evaluate whether national SARS-CoV-2 vaccine programmes have had an impact on the incidence of immunological rejection of corneal transplants we conducted an observational retrospective cohort study to investigate the rates of graft rejection presenting to the Emergency Department at Moorfields Eye Hospital, City Road, London, UK and Ospedali Privati Forlì “Villa Igea”, Italy both before and after the national SARS-CoV-2 vaccination programme. Moorfields Eye is responsible for over 20% of all corneal graft surgery nationally (A Rahman, Eye Bank Manager, Moorfields Lion Eye Bank, email communication, July, 2020) and provides specialised tertiary level ophthalmic care to the greater London area including running 24-h 7 days a week walk-in ophthalmic emergency department (ED), which prior to the pandemic would welcome on average over 1900 attendances per week. On the other hand, Ospedali Privati Forlì “Villa Igea” is tertiary care eye centre seeing 200–300 cornea cases weekly and performing over 10% of corneal transplants performed in Italy (D Ponzin, Fondazione Banca degli Occhi del Veneto Onlus, personal communication, March 2022).
Methods
This multicentre retrospective cohort study was approved as a Clinical Audit report by the Clinical Audit Committee at Moorfields Eye Hospital (London, UK) and Institutional review board/ ethics Committee approval was obtained from the Comitato Etico Ospedali Privati Forlì (Forlì, Italy). The study was performed in accordance with the tenets of the Declaration of Helsinki.
We performed a retrospective review of cases presenting to the cornea and external disease service at Moorfields Eye Hospital, City Road and Ospedali Privati Forlì “Villa Igea” (OPF) from January 2018 to March 2022. Inclusion criteria included all patients 18 years or older with a clinical diagnosis of graft rejection. At Moorfields, the case notes of all included cases were then reviewed by two independent observers experienced in cornea in order to perform a final confirmation of the diagnosis with the benefit of medical notes from subsequent follow up in the corneal service. All cases presenting at Ospedali Privati Forlì “Villa Igea” were seen by a cornea specialist. Graft rejection was defined as patients who developed an epithelial rejection line, subepithelial or stromal infiltrates, keratic precipitates or anterior chamber cell reaction with or without clinically apparent increase in stromal thickness or clarity.
Data analysis
All data had been collected prospectively and entered into the patient’s electronic medical records from the Moorfields Electronic Patient Record (EPR) System (OpenEyes, Apperta Foundation CIC, Sunderland, UK), which mandates recording.
Using the Moorfields dataset, we statistically compared new case presentations using non-parametric independent group Mann–Whitney U pre- and post- lockdown (March 2020), and pre- and post-vaccination roll out (February 2021). Similarly, data from the electronic database of OPF were also analysed. Vaccine status was ascertained among patients who developed corneal graft rejection. Conditional Poisson regression analysis was used to evaluate whether the association exists between COVID-19 vaccination and corneal graft rejection. Incidence risk ratio (IRR) of corneal graft rejection was calculated to compare the COVID-19 vaccination risk period, defined as the interval between vaccination and 60 days from the last dose with the control period defined as the observation period excluding risk period.
Furthermore, we obtained cumulative regional vaccination statistics from the Public Health England open-source data set to undertake a regression analysis to ascertain the effect of the UK COVID-19 vaccine programme on new case presentations [17]. A p value less than 0.05 was considered clinically significant.
Results
Moorfields Eye Hospital
Between January 2018 and March 2022, there were 471 corneal graft rejection episodes with a median rate of 9 patients per month (Range 3–18) at Moorfields Eye Hospital. 62% were male (n = 292), and the average age was 56 (range 18–97).
In the 26 months prior to national lockdown from January 2018 to February 2020 the median number of corneal graft rejections per month was 12 (range 8–18), which was significantly different to post lock down (March 2020–March 2022, median 6 cases per month, p = 0.001). From the start of vaccination programme in the United Kingdom late January 2021, the median number of corneal graft rejections per month was 6 (Range 5–9), which was not significantly different to post-lockdown, pre-vaccination programme (March 2020–January 2021), p = 0.367.
In total, 44 million received the first dose, 41 million people have had the second dose, and 32 million have received the third (booster) dose of the COVID-19 vaccine in England (as of March 2022). The cumulative percentage uptake of the COVID-19 vaccine in London was reported to be 70%, 65%, 46% for first, second and third dose respectively (Fig. 1). Regression analysis did not demonstrate a significant relationship between regional cumulative percentage vaccination uptake (first, second or third dose) and the number of corneal graft rejection episodes per month following vaccination roll out (r2 = 0.09, p = 0.667).
Blue line - number of immune mediated graft rejection in Emergency Department, Moorfields Eye Hospital, City Road, London. Orange line - cumulative percentage uptake of COVID vaccination in London (first dose). Grey line - cumulative percentage uptake of COVID vaccination in London (second dose). Orange line - cumulative percentage uptake of COVID vaccination in London (third dose).
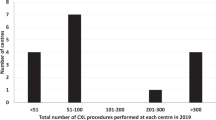
Ospedali Privati Forlì
During the same time period, 95 episodes of corneal graft rejection were diagnosed at OPF with a median rate of 2 per month. Of the 95 cases, 82 (86%) patients had received COVID-19 vaccination, compared to 85% of the overall population. The median rates of rejection before and after initiation of the vaccination programme were not significantly different (p = 0.124). Figure 2 shows the uptake of the COVID-19 vaccines in Emilia-Romagna, Italy and frequency of rejection episodes diagnosed over the same time period. No notable increase was noted when COVID-19 vaccination was broadly implemented.
Using conditional Poisson regression analysis of rejection episodes between January 2018 and March 2022, we found no significant increase in incidence rate of rejection between COVID-19 vaccination and 60 days from the last vaccine dose (IRR = 0.53, p = 0.71).
Discussion
Before the national lockdown in March 2020, Moorfields ED saw an average of 12 corneal graft rejections a month. From the start of the UK national vaccination programme the average number was 6 rejections per month. Regression analysis found no significant effect on vaccines on the number of presentation of rejections (r2 = 0.09, p = 0.667). Similarly, no increase in rejection cases were observed at OPF, Italy. If SARS-CoV-2 vaccines were associated with even a slight association of risk of corneal graft rejection, then one would expect that by vaccinating the majority of the population in the space of a few months there would have been an increase in the number of rejection episodes presenting at both centres. Given that the risk of rejection persists throughout the lifetime of the corneal graft even without an identifiable trigger, background incidence can account for rejection episodes that expectedly occur at any time over any given period following keratoplasty. We, therefore, suggest that based on our routinely collected longitudinal data using standard case definitions and methods of ascertainment, our data do not lend support to an association between COVID-19 vaccination and corneal graft rejection. This is further supported as this finding is replicated across two large European centres, each of which provide a large proportion of their national corneal transplantation workload.
Our results are in keeping with the only other two publications we are aware of which have evaluated the risk of rejection associated with vaccines. The Corneal Preservation Time Study group found that vaccines within the previous three months were not a significant factor associated with corneal graft rejection in Descemet stripping automated endothelial keratoplasty [18]. Equally, a Wills Eye Hospital prospective case–control study evaluating trigger factors for penetrating keratoplasty rejection did not find an association with recent vaccinations in their 22 rejection patients compared with controls (immunisation exposure equally prevalent in both groups) [19]. Both of the above studies occurred prior to COVID vaccinations.
There are a number of methodological issues with a study of this nature. We examined the monthly rates of corneal transplant rejections but did not characterise these clinically. At Moorfields, the vaccine status of corneal graft rejection patients presenting during this time frame was not rigorously recorded, but at OPF the conditional Poisson regression analysis did not find a significant increase in incidence rate of rejection between COVID-19 vaccination and 60 days from the last vaccine dose.
At Moorfields we observed a reduction in the rate of rejection which occurred in keeping with the first national lockdown. It is well recorded that healthcare seeking behaviours were affected by the pandemic. Face-to-face attendances at Moorfields ED did reduce by over 50% in the early phase of the first national lockdown in March–April 2020 [20]. However, the case mix and severity of conditions also shifted. Prior to the pandemic, blepharitis was the most common cause for presentation, after the onset of the pandemic it became acute anterior uveitis [20]. Hence to some extent, the reduction in attendances would have been skewed against more minor conditions, and may have had less of an effect on severe conditions, although it is well documented that rates of presentations of rhegmatogenous retinal detachments reduced during the first lockdown [20, 21].
A reduction in recent corneal transplant rates may have had an impact on rates of corneal graft rejection as 50% of corneal rejection episodes may occur during the first twelve months after surgery [18]. On average, approximately 4,000 corneal transplants are performed in the UK each year, however, this would have been significantly less in the 12 months prior to the vaccination programme. There was a 92% reduction in corneal elective work at Moorfields Eye Hospital during the first national lockdown [22]. Services were likewise significantly reduced in OPF Italy [23]. In OPF patients were not advised to increase their topical steroid dose at the time of vaccine. At Moorfields, where there are more than ten corneal consultants, management may have been more heterogenous. Nevertheless, there is no available evidence to support increasing topical steroids around the time of vaccination, this practice is speculative.
Our real world data reflects overall trends during a unique time period with inherent limitations on the use of more complex analytic methods requiring more granular information to account for potential confounding variables such as care at other sites, self quarantining, self treatment, untreated rejections, etc. Both Moorfields and OPF continued ophthalmic services for urgent care throughout the pandemic (indeed Moorfields continued to offer a 24/7 emergency service while other smaller London units closed). While both centres observed a sharp decline in healthcare utilisation in March–April 2020, there was a recovery of numbers after this period.
Despite the clear limitations of this study, we advocate that if there was a true association between the SARS-CoV-2 vaccine and corneal graft rejection then the effects of vaccinating nearly the entire population over a period of a few months would have impacted in a visible way upon the number of presentations.
In the future, it may be more helpful to perform a matched case-control study through large transplant registries to identify in a more robust way whether there may be any association not detected by this study in both centres.
In summary, national vaccination programmes in the UK and Italy for SARS-CoV-2 has not seen an associated increase in the incidence of corneal graft rejection which may be expected if there were an association.
Summary
What was known before
-
In the last 2 years many case reports or case series have questioned an association between SARS-CoV-2 vaccine and corneal transplant rejection.
What this study adds
-
This paper demonstrates that 2 major corneal centres, Moorfields in London UK and Ospedali Privati Forli “Villa Igea”, Italy did not see an increase in the rate of rejection presentations during the national vaccination campaigns, strongly indicating a lack of evidence for any association.
Data availability
Data available upon written request to the corresponding author.
References
World Health Organization Technical Advisory Group for COVID-19 Mortality Assessment. https://www.who.int/news/item/05-05-2022-14.9-million-excess-deaths-were-associated-with-the-covid-19-pandemic-in-2020-and-2021. Accessed May 20, 2022.
Voysey M, Clemens SAC, Madhi SA, Weckx LY, Folegatti PM, Aley PK. et al. Articles safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021;397:99–111.
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N. Engl J Med. 2020;383:2603–15.
Balidis M, Mikropoulos D, Gatzioufas Z, de Politis PB, Sidiropoulos G, Vassiliadis V. Acute corneal graft rejection after anti-severe acute respiratory syndrome-coronavirus-2 vaccination: A report of four cases. Eur J Ophthalmol. 2021:11206721211064033. https://doi.org/10.1177/11206721211064033. Online ahead of print.
Abousy M, Bohm K, Prescott C, Bonsack JM, Rowhani-Farid A, Eghrari AO. Bilateral EK rejection after COVID-19 vaccine. Eye Contact Lens. 2021;47:625–8.
Yu S, Ritterband DC, Mehta I. Acute corneal transplant rejection after severe acute respiratory syndrome coronavirus 2 mRNA-1273 vaccination. Cornea. 2022;41:257–9.
Parmar DP, Garde PV, Shah SM, Bhole PK. Acute graft rejection in a high-risk corneal transplant following COVID-19 vaccination: A case report. Indian J Ophthalmol. 2021;69:3757–8.
Phylactou M, Li J-PO, Larkin DFP. Characteristics of endothelial corneal transplant rejection following immunisation with SARS-CoV-2 messenger RNA vaccine. Br J Ophthalmol. 2021;105:893–6.
Rallis KI, Ting DSJ, Said DG, Dua HS. Corneal graft rejection following COVID-19 vaccine. Eye. 2021. ePub ahead of print.
Nioi M, d’Aloja E, Fossarello M, Napoli PE. Dual corneal-graft rejection after mRNA vaccine (BNT162b2) for COVID-19 during the first six months of follow-up: case report, state of the art and ethical concerns. Vaccines (Basel). 2021;9:1274.
Molero-Senosiain M, Houben I, Savant S, Savant V. Five cases of corneal graft rejection after recent COVID-19 vaccinations and a review of the literature. Cornea. 2022;41:669–72.
Simão MF, Kwitko S. Corneal graft rejection after inactivated SARS-CoV-2 vaccine: case report. Cornea. 2022;41:502–4.
Wasser LM, Roditi E, Zadok D, Berkowitz L, Weill Y. Keratoplasty rejection after the BNT162b2 messenger RNA vaccine. Cornea 2021;40:1070–2.
Shah AP, Dzhaber D, Kenyon KR, Riaz KM, Ouano DP, Koo EH. Acute corneal transplant rejection after COVID-19 vaccination. Cornea. 2022;41:121–4.
Rajagopal R, Priyanka TM. Stromal rejection in penetrating keratoplasty following COVID-19 vector vaccine (Covishield)—A case report and review of literature. Indian J Ophthalmol. 2022;70:319–21.
Ravichandran S, Natarajan R. Corneal graft rejection after COVID-19 vaccination. Indian J Ophthalmol. 2021;69:1953–4.
Vaccinations in United Kingdom (2021). httpscoronavirus.data.gov.ukdetailsvaccinations.
Stulting RD, Lass JH, Terry MA, Benetz BA, Cohen NJ, Ayala AR, et al. Factors associated with graft rejection in the cornea preservation time study. Am J Ophthalmol. 2018;196:197–207.
Miedziak AI, Tambasco F, Lucas Glass TC, Rapuano CJ, laibsan PR, Cohen E. Evaluation of triggers for corneal graft rejection. Ophthalmic surgery, lasers and imaging. Retina. 1999;30:133–9.
Wickham L, Hay G, Hamilton R, Wooding J, Tossounis H, da Cruz L, et al. The impact of COVID policies on acute ophthalmology services-experiences from Moorfields Eye Hospital NHS Foundation Trust. Eye. 2020;34:1189–92.
Akram H, Dowlut MS, Karia N, Chandra A. Emergency retinal detachment surgery during Covid-19 pandemic: a national survey and local review. Eye. 2021;35:2889–90.
Din N, Phylactou M, Fajardo-Sanchez J, Watson M, Ahmad S. The impact of COVID-19 on acute and elective corneal surgery at Moorfields Eye Hospital London. Clin Ophthalmol. 2021;15:1639–45.
Busin M, Yu AC, Ponzin D. Coping with COVID-19: an italian perspective on corneal surgery and eye banking in the time of a pandemic and beyond. Ophthalmology. 2020;127:e68–9.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND Drafting the work or revising it critically for important intellectual content; AND Final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
HR has undertaken paid consultancy work for Alcon Inc (Fort Worth, TX, USA) in the past 36 months and has received honoraria from Thea Pharmaceuticals Ltd (Keele, UK). The other authors have no financial interest to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Roberts, H.W., Wilkins, M.R., Malik, M. et al. A lack of an association between COVID-19 vaccination and corneal graft rejection: results of a large multi-country population based study. Eye 37, 2316–2319 (2023). https://doi.org/10.1038/s41433-022-02341-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02341-7
This article is cited by
-
Risk of Corneal Transplant Rejection Following COVID-19 Vaccination: A Systematic Review and Meta-analysis
Ophthalmology and Therapy (2024)