Abstract
Background
In 2020, routine cataract surgery was halted in most countries due to the COVID-19 pandemic in order to reduce transmission. With a consequent lack of theatre space, we developed a safe cataract pathway in outpatient department clean rooms to minimize patient exposure and time spent in hospital using a sterile laminar air flow device. We describe our initial experiences of restarting elective cataract surgery in the UK outpatient setting, outside of the operating theatre environment.
Methods
This was a prospective consecutive study of our clinical practice. A sterile air zone unit, the Toul Meditech Operio Mobile device, was used to create a sterile surgical site in three separate outpatient clean rooms from May 2020 to December 2021 in different geographical locations within Herefordshire, UK. Observations of the time spent in the department and a formal patient satisfaction survey were carried out for the initial 100 patients. All patients were followed up to assess development of post-operative complications.
Results
1269 patients were included in the study. No patients sustained post-operative infection (n = 0/1269, 0%). For the initial 100 patients, the average time spent within the department was 74.3 min (unilateral cases, range 45–115 min) and 93.1 min (bilateral, 55–135 min). Patient satisfaction was high.
Conclusion
Initial results demonstrate a safe, efficient and effective cataract surgery pathway with high patient satisfaction by converting outpatient clean rooms into ophthalmic operating theatres using the Toul Meditech Operio Mobile.
Similar content being viewed by others
Introduction
The Coronavirus disease 2019 (COVID-19) global pandemic has had an unprecedented effect on healthcare across the world. In an effort to reduce transmission of the highly contagious SARS-Cov2 virus responsible for the disease, all NHS elective and non-urgent care was cancelled or postponed [1] in 2020. Over the 12-week period between March and May 2020, globally an estimated 28,000,000 routine surgeries were cancelled. In the UK this equated to a weekly cancellation rate of roughly 43,000 surgeries [2]. Deferring these surgeries has had its own consequences, resulting in worsening of patients’ conditions and adding risk to the eventual surgery [3]. With the duration of the COVID pandemic uncertain, there was understandably a desire to restart routine surgery as safely as possible.
We aim to describe our innovative experience of restarting elective cataract surgery in the UK during the COVID-19 pandemic using an air-flow device. Following the recommendations of the Royal College of Ophthalmologists, we describe a pathway that allowed us to minimise the total time patients spend in the hospital, reduce contact with staff and eliminate the use of a waiting area [4]. We used mobile paging devices, which allowed patients to leave the department after insertion of a mydriatic device. Converting an outpatient clean room into an operating theatre allowed us to perform cataract surgery in the outpatient setting at a time where theatre space was limited. In order to do this, we used a mobile sterile air zone unit, the Toul Meditech Operio Mobile (shown in Supplementary Fig. 1). Bacteria, skin scales and lint particulate matter from the air in the operating room are thought to be a source of infection in sterile surgery [5]. Modern operating theatres have ventilation systems that are designed to reduce this risk. The Toul Meditech Operio Mobile device produces a filtered ultra-clean air flow that can be directed over the surgical site and sterile instruments to maintain sterility [6]. Air is cleaned by passing it through a high efficiency particulate air (HEPA) filtration system that has been shown to filter particulates of sizes less than 0.18 µm. This creates a zone of clear air measuring 20 inches in width, 47 inches in length and 15 inches in height within which the operating field is positioned. The SARS-Cov2 virus is known to have a size of approximately 0.1 µm and therefore the Toul Meditech Operio Mobile device has also been recommended as a possible solution to reduce the transmission of COVID-19 in an operating environment but so far there is paucity of data on its use in cataract surgery. These papers aim to describe our initial experiences and service evaluation of the Toul Meditech Operio Mobile device in cataract surgery.
Materials and methods
Initially, the first 100 patients undergoing cataract surgery between May and July 2020 under five senior surgeons were studied in detail. In order to provide accurate data on the time spent in the department for consultant-delivered routine cataract surgery, patients undergoing combined procedures (e.g., phaco + istents, oculoplastics) and all patients on such mixed lists, and those undertaken by trainee surgeons were excluded.
All patients were contacted via telephone pre-operatively to discuss the risks of COVID-19 by a consultant surgeon. At the time of booking, all patients were asked COVID-19 screening questions. All patients had initially completed stage one of the consent process with a doctor at the clinic/listing stage.
All staff were required to have their temperature taken daily and to wear surgical masks at all times while in the department (prior to UK government directive mandating universal wearing).
An outpatient style flow through the department was created to ensure patients were in the hospital for the shortest possible time with staggered arrival times. In line with NHS England directives [4], as the patients were all treated as outpatients, patients were not required to undergo a two-week isolation period prior to surgery, nor did they undergo PCR swabbing for SARS-Cov2. On arrival, they had their temperature checked and COVID-19 screening questions were again asked. Once they had been booked into the department and initial checks were completed, a Mydriasert mydriatic device (Thea Pharmaceuticals) was inserted into the inferior fornix of the relevant eye(s) to be operated and the patient was asked to wait outside the department, often in their car, until pupil dilation was complete. Mydriasert is an insoluble ophthalmic insert for mydriasis that gradually releases its active ingredients of 0.25 mg tropicamide and 5.4 mg phenylephrine over up to a two-hour period, however, sufficient dilatation is typically achieved in 40 min [7]. The patients were then paged using a cleanable series of remote buzzer/pager devices to come back to the department to complete consent with the surgeon and then taken directly into surgery. This eliminated the use of a waiting area, as well as reducing time spent in the department.
The Toul Meditech Operio Mobile medical device was used in the clean room in order to filter the air and provide a sterile area within which to carry out cataract surgery, in line with Royal College of Ophthalmologists guidelines [8]. A representative from Toul advised on the positioning of the device. The risk of infection was further reduced by ensuring the door was kept closed for the duration of the surgery and that there was minimal talking while operating, with all staff wearing masks. Instruments were laid out in the clean room under the Toul Meditech Operio Mobile filter rather than in a separate room. The number of people in the room was minimised using one surgeon, one surgical assistant, one scrub nurse and usually one theatre support worker. Phacoemulsification was carried out using the Bausch & Lomb Stellaris, using 2.2 mm and 2.85 mm incisions, with copious dispersive viscoelastic on the cornea during surgery. All surgery was carried out with two-stage povidone iodine cleaning, careful draping and intracameral antibiotics.
The use of the clean room for surgery, in conjunction with the Toul Meditech Operio Mobile, was agreed with the local infection control team.
Patients’ various arrival and departure times were all collected prospectively. The initial 100 patients were contacted by telephone two weeks after cataract surgery to answer a short questionnaire regarding any post-operative complications, development of COVID symptoms and satisfaction (using a Likert scale). Departmental records regarding attendance with post-operative endophthalmitis were also interrogated.
After the initial 100 patients, another 215 consecutive patients underwent surgery in the same clean room, with all patients undergoing follow-up with local optometrists. The same equipment was then procured to reproduce the operating environment in two other geographic locations in Herefordshire, within outpatient clean rooms elsewhere. Using the same protocols as above, a further 954 consecutive patients underwent routine phacoemulsification surgery, with all using the Bausch & Lomb Stellaris and 2.2 mm incisions. All of these 954 patients were followed up in person by the operating surgeon in every case.
Results
In total, 1269 patients were included in the study.
The initial 100 cases
The first 100 patients to undergo treatment with this pathway were studied in detail. Of these, the average age was 74.48 (range 39–89) with 51% male (n = 51) (Table 1). The axial length of the operated eye ranged between 20.40 and 28.00 mm with an average of 23.73 mm (Table 1). A range of patients with varying surgical difficulty was included with 22 % diabetic (n = 22), 10% glaucoma (n = 10), 1% with previous uveitis (n = 1) and 1% with pseudoexfoliation syndrome (n = 1). Vision blue was used in 10%, (n = 10), adjuncts for pupil expansion (iris hooks, Malyugin ring) in 0% (n = 0) and capsular tension rings in 1%, (n = 1). 4% (n = 4) of patients had other co-morbidities such as age-related macular degeneration, 3% (n = 3) had previous vitrectomies, and 5% (n = 5) were high myopes.
Of the initial 100 cases, the majority received topical anesthesia (81%, n = 81) with one surgeon opting for anesthesia via sub-Tenon injection (19%, n = 19). Similarly, the majority (79%) were performed with a 2.2 mm incision (79%, n = 79) with one surgeon extending incisions to 2.85 mm (20%, n = 20) and 1% (n = 1) at 3 mm section length. No intra-operative complications were noted. Patients spent on average 74.3 min (range 45–115) in the department (Table 2). This was broken down into the initial booking-in time and insertion of Mydriasert that took 9.2 min on average (range 5–15) and the time for examining the patient, completing consent, performing the operation and explaining the post-operative drops and care (65.1 min (range 40–100)).
One surgeon undertook bilateral cataract surgeries, which were analysed separately (Table 2). The average time spent in the department for bilateral surgeries was 93.1 min (range 55–135) with the initial insertion of dilator lasting 8.5 min on average (range 5–15) and time for consent, bilateral surgery and post-op care 84.7 min on average (range 50–120).
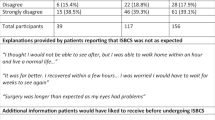
The results of the post-operative questionnaire at 2 weeks showed 0/100 (0%) of patients developed post-operative complications. No patient reported a reduction in vision or pain consistent with endophthalmitis and there were no visits to our emergency ophthalmology service with suspected or confirmed endophthalmitis in this period. No patients had developed any symptoms of COVID-19 at 2 weeks postoperatively. No staff developed any symptoms of COVID-19. The Likert–scale used for patient satisfaction showed that most patients were very satisfied with the cataract service (average 9.54 (range 4–10)). All patients felt the service ran efficiently and appreciated the experience of being the only patient in the department at the time.
Remaining 1169 cases
Of the further 215 consecutive patients, who underwent surgery in the same clean room with the same equipment, 0/215 patients (0%) developed postoperative endophthalmitis. Of the further 954 consecutive patients, who then underwent routine phacoemulsification using the same equipment and protocols in two other clean rooms in Herefordshire, 0/954 patients (0%) developed postoperative endophthalmitis. In total, therefore, 0/1269 (0.0%) consecutive patients developed postoperative endophthalmitis. No patient or staff member developed symptoms of COVID-19 infection from any location.
Discussion
This is the first service evaluation of the safety of cataract surgery using the Toul Meditech Operio Mobile device in an outpatient clean room, outside of an operating theatre environment. Of the 1269 consecutive patients, no cases of intraocular infection occurred and no patients or staff developed COVID-19. Our preliminary data show that cataract surgery appears to be safe and efficient in a clean room using the Toul Meditech Operio Mobile unit creating a sterile field. For the initial 100 patients, the mean time spent in the outpatient setting was significantly less than Royal College of Ophthalmologist guidelines (90 min) [4] and patients were very satisfied with the service.
The use of the Toul Meditech Operio Mobile device in surgery in general is not novel and it has been licensed for use in intravitreal injections as well as cataract surgery [6, 9,10,11,12]. Despite this, there is very little data investigating its use in clinical settings of cataract surgery. Laminar air flow models have been investigated since the 1960s and have been shown to significantly reduce the incidence of devastating surgical site infections [13]. A study undertaken in Hudiksvall Hospital in August 2015 investigated whether the use of the Toul Meditech Operio Mobile device during general surgery reduced the air-borne bacterial colony forming units (CFU) near the surgical site and over instruments [14]. They investigated two hernia surgeries and one colon surgery and measured the CFU levels and particulates in the air by using a CFU sampler and sterile agar plates. A maximum of 7 people were present in the room and ensured good door discipline similar to our operating procedure [15]. They found a significant difference in CFU (mean value 1) in the critical zone covered by the device when compared to the ambient air (mean value 29.5) used as a reference producing air over 50 times cleaner for the device.
The use of Toul Meditech Operio Mobile for safety during intravitreal injections has also been assessed at a Swedish eye department [16]. They assessed the air CFU levels at the surgical site during 23 injections and found a significant difference with a mean CFU of 1 at the critical zone versus a mean of 48 in the ambient air. Similarly, the use of the device in a simulated setting for intravitreal injections showed a safer procedural environment with reduction in particulate matter in the ambient air [12] and a case series of 39 small joint arthroplasty surgeries showed no significant difference in the rate of infections, intraoperative or post-operative complications over a 12 month follow up [17]. More recently Osher et al used the Toul Meditech Operio Mobile to detect the number of particulate matter and lint fibres in the sterile surgical field and found a statistically significant reduction in these particles with 0% lint fibres falling onto the sterile field [18]. They report relative paucity of data of the use of the device in clinical practice for cataract surgery. Our study is the first to investigate its use in cataract surgery at this scale.
The Royal College of Ophthalmologists produces guidelines to ensure minimum standards in ventilation in operating theatres, however, ventilation systems used can vary in airflow patterns and cleaning efficiency may not be uniform. The filters used may become obstructed and need regular maintenance, or be blocked by surgical equipment [18]. The Toul Meditech Operio Mobile device creates a small uniform sterile field that we have shown to be safe. Its portable and mobile nature circumvents these disadvantages of larger ventilation systems, allowing the safe conversion of an outpatient clinic rooms into a sterile operating theatre.
We found productivity to be equivalent to a standard operating theatre, with the ability to complete the same number of cases on a list and the National Health Service Getting It Right First Time (GIRFT) standard of one cataract per 30 min is easily achievable even with only one Toul Meditech Operio Mobile device. The suppliers often advise the purchase of two machines, which therefore allows for sterile laying up for the next case by a third party, which should then further improve productivity. With the set-up used within the NHS setting described, training continued in much the same way as in a standard operating theatre, with no extra difficulties experienced. The ability to further increase productivity could be an important factor to relieve some of the pressures of recovery post pandemic.
Our results are consistent with the studies discussed above showing no post-operative complications or infections in a consecutive group of 1269 patients undergoing routine phacoemulsification surgery. No patients and staff developed any symptoms of COVID-19. The incidence of endophthalmitis in the developed world is low at 0.01–0.08% and 0.14% in the UK determined from the British Ophthalmological Surveillance Unit (BOSU) study [19]. We acknowledge that, as postoperative endophthalmitis is a rare event, these data do not prove the safety of the system described, nevertheless the data do show a level of postoperative infection comparable to existing national standards. Further data from future BOSU studies with a larger sample size (exact numbers to be determined by statistical analysis beyond the scope of this paper) may help provide further confirmation of safety. Our initial experiences with the Toul Meditech Operio Mobile appear to show that it offers a safe, air-filtered environment for cataract surgery, within the outpatient setting described facilitating an excellent, patient-centred and efficient use of resources and time.
Summary
What was known before
-
Due to the lack of theatre space during the COVID-19 pandemic and growing demands to the cataract surgery service, there is a need to develop safe and efficient surgical pathways to meet this demand. Air-flow devices have been used to create sterile surgical environments in specialities such as orthopaedics as well as in ophthalmology for intravitreal injections but there is limited data for its use in cataract surgery.
What this study adds
-
We describe the first use of a novel laminar airflow device in cataract surgery, allowing safe and efficient use of an outpatient cataract pathway for the first time. The findings from our study would allow many units in this country and worldwide to continue to provide safe cataract surgery while adapting and expanding their practice.
Data availability
All data generated or analysed during this study are included in this published article (and its supplementary information files).
References
Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: A systematic review. PLoS One. 2012;7:35797. https://doi.org/10.1371/journal.pone.0035797.
COVIDSurgCollaborative. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;395:1022. https://doi.org/10.1002/bjs.11746.
Myles PS, Maswime S. Mitigating the risks of surgery during the COVID-19 pandemic. Lancet. 2020;396:2–3. https://doi.org/10.1016/S0140-6736(20)31256-3.
The Royal College of Ophthalmologists. Guidance on the Resumption of Cataract Services during COVID.; 2020. https://www.rcophth.ac.uk/wp-content/uploads/2021/01/Resumption-of-Cataract-Services-COVID-August-2020-2.pdf (last accessed 30th October 2022)
Lidwell OM, Lowbury EJL, Whyte W, Blowers R, Stanley SJ, Lowe D. Airborne contamination of wounds in joint replacement operations: the relationship to sepsis rates. J Hosp Infect. 1983;4:111–31. https://doi.org/10.1016/0195-6701(83)90041-5.
Sossai D, Dagnino G, Sanguineti F, Franchin F. Mobile laminar air flow screen for additional operating room ventilation: Reduction of intraoperative bacterial contamination during total knee arthroplasty. J Orthop Traumatol. 2011;12:207–11. https://doi.org/10.1007/s10195-011-0168-5.
Shah A, Johal S, Lee N. Mydriasert pupillary dilation for cataract surgery: An economic and clinical study Cataract and refractive surgery. BMC Ophthalmol. 2015;15:56. https://doi.org/10.1186/s12886-015-0042-y.
Guidance OS Theatre facilities and equipment. R Coll Ophthalmol. Published online 2018. https://www.rcophth.ac.uk/wp-content/uploads/2021/01/Theatre-facilities-equipment-Copy.pdf (last accessed 30th October 2022)
Friberg S, Ardnor B, Lundholm R, Friberg B. The addition of a mobile ultra-clean exponential laminar airflow screen to conventional operating room ventilation reduces bacterial contamination to operating box levels. J Hosp Infect. 2003;55:92–97. https://doi.org/10.1016/S0195-6701(03)00143-9.
Nilsson KG, Lundholm R, Friberg S. Assessment of horizontal laminar air flow instrument table for additional ultraclean space during surgery. J Hosp Infect. 2010;76:243–6. https://doi.org/10.1016/j.jhin.2010.05.016.
von Vogelsang AC, Förander P, Arvidsson M, Löwenhielm P. Effect of mobile laminar airflow units on airborne bacterial contamination during neurosurgical procedures. J Hosp Infect. 2018;99:271–8. https://doi.org/10.1016/j.jhin.2018.03.024.
Lapid-Gortzak R, Traversari R, van der Linden JW, Lesnik Oberstein SY, Lapid O, Schlingemann RO. Mobile ultra-clean unidirectional airflow screen reduces air contamination in a simulated setting for intra-vitreal injection. Int Ophthalmol. 2017;37:131–7. https://doi.org/10.1007/s10792-016-0236-1.
McHugh SM, Hill ADK, Humphreys H. Laminar airflow and the prevention of surgical site infection. More harm than good? Surgeon. 2015;13:52–8. https://doi.org/10.1016/j.surge.2014.10.003.
Toul Meditech. The use of the air zone unit Operio and the instrument table SteriStay over critical zone and instruments to reduce air-borne contamination at hernia and colon cancer surgery. Published online 2015.
Smith EB, Raphael IJ, Maltenfort MG, Honsawek S, Dolan K, Younkins EA. The effect of laminar air flow and door openings on operating room contamination. J Arthroplast. 2013;28:1482–5. https://doi.org/10.1016/j.arth.2013.06.012.
Toul Meditech. The use of Operio at intravitreal injections. Published online 2015. https://www.toulmeditech.com/us/clinical#hide45 (last accessed 30th October 2022).
Nisar A, Shah Z, Pendse A, Chakrabarti I. Day case total joint arthroplasty in the hand: Results in a district general hospital. J Hand Surg Eur Vol. 2009;34:367–70. https://doi.org/10.1177/1753193408102117.
Osher RH, Figueiredo GB, Schneider JG, Kratholm J. Purifying air over the operating field with a new mobile laminar airflow device to reduce the possibility of airborne contamination. J Cataract Refract Surg. 2021;47:1327–32. https://doi.org/10.1097/j.jcrs.0000000000000613.
Kamalarajah S, Silvestri G, Sharma N, Khan A, Foot B, Ling R, et al. Surveillance of endophthalmitis following cataract surgery in the UK. Eye. 2004;18:580–7. https://doi.org/10.1038/sj.eye.6700645.
Author information
Authors and Affiliations
Contributions
RP, BW and SM- conceptualisation, methodology, analysis of data. All authors (RP, BW, SM, AS, JD, SS, GM, GW) contributed to data collection, development of manuscript and approved final manuscript.
Corresponding author
Ethics declarations
Competing interests
No conflicts of interest. GPW is a consultant for Thea Pharmaceuticals. SNM is a consultant for Thea Pharmaceuticals and Alcon UK. No other financial interests or relationships to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Patel, R.P., While, B., Smith, A. et al. Initial experiences of cataract & lens surgery in 1269 patients in outpatient clean rooms using a portable laminar air flow device. Eye 37, 2212–2215 (2023). https://doi.org/10.1038/s41433-022-02317-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02317-7