Abstract
Objectives
To determine spherical equivalent (SE) progression among children in the Shahroud School Children Eye Cohort Study.
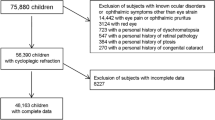
Methods
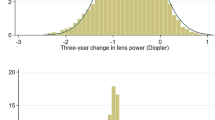
A prospective cohort study recruited children aged 6 to 12 years in 2015 (baseline) with a follow-up in 2018. Cycloplegic autorefraction and axial length (AL) measurements were included. SE progression over 3 years was analysed in non-myopic (SE ≥ + 0.76 D), pre-myopic (PM; SE between +0.75 D and –0.49 D), low myopic (LM; SE between −0.5 D and −5.99 D), and high myopic (HM; SE ≤ − 6 D) eyes. Age, sex, near work, outdoor time, living place, parental myopia, mother’s education, and baseline SE were evaluated as risk factors for SE progression (≤ −0.50 D).
Results
Data were available for 3989 children (7945 eyes). At baseline, 40.3% (n = 3205), 3.4% (n = 274) and 0.1% (n = 7) eyes had PM, LM and HM, respectively. At the 3-year follow-up, 40.5% (n = 3216), 7.5% (n = 599) and 0.2% (n = 15) eyes had PM, LM, and HM, respectively. SE progression in eyes with LM and HM was −1.08 ± 0.76 D and −1.60 ± 1.19 D, respectively. SE progression was associated with age at baseline (Odds Ratio [OR] = 1.14; 95% confidence interval [CI], 1.08–1.21), female sex (OR = 1.80; 95% CI: 1.48–2.18), near work (OR = 1.08; 95% CI: 1.02–1.14), parental myopia (OR = 1.20; 95% CI: 1.01–1.42) and baseline SE (OR = 2.28; 95% CI: 1.88–2.78).
Conclusion
A myopic shift was associated with older age, female sex, near work, parental myopia and greater myopic baseline SE. These results help identifying children at risk of progression that may benefit from treatment and lifestyle counselling.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P. et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–42. https://doi.org/10.1016/j.ophtha.2016.01.006.
Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, Smith W. et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115:1279–85. https://doi.org/10.1016/j.ophtha.2007.12.019.
He M, Xiang F, Zeng Y, Mai J, Chen Q, Zhang J. et al. Effect of time spent outdoors at school on the development of myopia among children in China. JAMA. 2015;314:1142. https://doi.org/10.1001/jama.2015.10803.
Ip JM, Saw SM, Rose KA, Morgan IG, Kifley A, Wang JJ. et al. Role of near work in myopia: findings in a sample of Australian school children. Investig Opthalmology Vis Sci. 2008;49:2903. https://doi.org/10.1167/iovs.07-0804.
Nickels S, Hopf S, Pfeiffer N, Schuster AK. Myopia is associated with education: Results from NHANES 1999-2008. PLoS One. 2019;14:e0211196 https://doi.org/10.1371/journal.pone.0211196.
Wong TY, Ferreira A, Hughes R, Carter G, Mitchell P. Epidemiology and disease burden of pathologic myopia and myopic choroidal neovascularization: an evidence-based systematic review. Am J Ophthalmol. 2014;157:9–25.e12. https://doi.org/10.1016/j.ajo.2013.08.010.
Polling JR, Klaver C, Tideman JW. Myopia progression from wearing first glasses to adult age: the DREAM Study. Br J Ophthalmol. 2021; https://doi.org/10.1136/bjophthalmol-2020-316234.
Fan DS, Lam DS, Lam RF, Lau JT, Chong KS, Cheung EY. et al. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Investig Opthalmology Vis Sci. 2004;45:1071. https://doi.org/10.1167/iovs.03-1151.
Tricard D, Marillet S, Ingrand P, Bullimore MA, Bourne RRA, Leveziel N. Progression of myopia in children and teenagers: a nationwide longitudinal study. Br J Ophthalmol. 2021. https://doi.org/10.1136/bjophthalmol-2020-318256.
Donovan L, Sankaridurg P, Ho A, Naduvilath T, Smith EL A, Holden B. Myopia progression rates in urban children wearing single-vision spectacles. Optom Vis Sci. 2012;89:27–32. https://doi.org/10.1097/OPX.0b013e3182357f79.
Yam JC, Jiang Y, Tang SM, Law AKP, Chan JJ, Wong E. et al. Low-concentration atropine for myopia progression (LAMP) study: a randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025%, and 0.01% atropine eye drops in myopia control. Ophthalmology. 2019;126:113–24. https://doi.org/10.1016/j.ophtha.2018.05.029.
Yen MY, Liu JH, Kao SC, Shiao CH. Comparison of the effect of atropine and cyclopentolate on myopia. Ann Ophthalmol. 1989;21:180–2, http://www.ncbi.nlm.nih.gov/pubmed/2742290.
Yi S, Huang Y, Yu SZ, Chen XJ, Yi H, Zeng XL. Therapeutic effect of atropine 1% in children with low myopia. J Am Assoc Pediatr Ophthalmol Strabismus. 2015;19:426–9. https://doi.org/10.1016/j.jaapos.2015.04.006.
Wang Y, Bian HL, Wang Q. Atropine 0.5% eyedrops for the treatment of children with low myopia. Med (Baltim). 2017;96:e7371 https://doi.org/10.1097/MD.0000000000007371.
Chua WH, Balakrishnan V, Chan YH, Tong L, Ling Y, Quah BL. et al. Atropine for the treatment of childhood myopia. Ophthalmology. 2006;113:2285–91. https://doi.org/10.1016/j.ophtha.2006.05.062.
Ma Y, Zou H, Lin S, Xu X, Zhao R, Lu L. et al. Cohort study with 4-year follow-up of myopia and refractive parameters in primary schoolchildren in Baoshan District, Shanghai. Clin Exp Ophthalmol. 2018;46:861–72. https://doi.org/10.1111/ceo.13195.
Pärssinen O, Lyyra AL. Myopia and myopic progression among schoolchildren: a three-year follow-up study. Invest Ophthalmol Vis Sci. 1993;34:2794–802. http://www.ncbi.nlm.nih.gov/pubmed/8344801.
Loh KL, Lu Q, Tan D, Chia A. Risk factors for progressive myopia in the atropine therapy for myopia study. Am J Ophthalmol. 2015;159:945–9. https://doi.org/10.1016/j.ajo.2015.01.029.
Fotouhi A, Hashemi H, Khabazkhoob M, Mohammad K. The prevalence of refractive errors among schoolchildren in Dezful, Iran. Br J Ophthalmol. 2007;91:287–92. https://doi.org/10.1136/bjo.2006.099937.
Norouzirad R, Hashemi H, Yekta A, Nirouzad F, Ostadimoghaddam H, Yazdani N. et al. The prevalence of refractive errors in 6- to 15-year-old schoolchildren in Dezful, Iran. J Curr Ophthalmol. 2015;27:51–55. https://doi.org/10.1016/j.joco.2015.09.008.
Emamian MH, Hashemi H, Khabazkhoob M, Malihi S, Fotouhi A. Cohort Profile: Shahroud Schoolchildren Eye Cohort Study (SSCECS. Int J Epidemiol. 2019;48:27–27f. https://doi.org/10.1093/ije/dyy250.
Cruickshank FE, Logan NS. Optical ‘dampening’ of the refractive error to axial length ratio: implications for outcome measures in myopia control studies. Ophthalmic Physiol Opt. 2018;38:290–7. https://doi.org/10.1111/opo.12457.
Hyman L. Relationship of age, sex, and ethnicity with myopia progression and axial elongation in the correction of myopia evaluation trial. Arch Ophthalmol. 2005;123:977. https://doi.org/10.1001/archopht.123.7.977.
Jong M, Jonas JB, Wolffsohn JS, Berntsen DA, Cho P, Clarkson-Townsend D. et al. IMI 2021 yearly digest. Investig Opthalmology Vis Sci. 2021;62:7 https://doi.org/10.1167/iovs.62.5.7.
Jones-Jordan LA, Sinnott LT, Chu RH, Cotter SA, Kleinstein RN, Manny RE. et al. Myopia progression as a function of sex, age, and ethnicity. Invest Ophthalmol Vis Sci. 2021;62:36. https://doi.org/10.1167/iovs.62.10.36.
Chamberlain P, Peixoto-de-Matos SC, Logan NS, Ngo C, Jones D, Young G. A 3-year randomized clinical trial of MiSight lenses for myopia control. Optom Vis Sci. 2019;96:556–67. https://doi.org/10.1097/OPX.0000000000001410.
Breslin KMM, O’Donoghue L, Saunders KJ. A prospective study of spherical refractive error and ocular components among Northern Irish schoolchildren (The NICER study). Investig Opthalmology Vis Sci. 2013;54:4843. https://doi.org/10.1167/iovs.13-11813.
Khor WB, Aung T, Saw SM, Wong TY, Tambyah PA, Tan AL. et al. An outbreak of Fusarium keratitis associated with contact lens wear in Singapore. JAMA. 2006;295:2867–73. https://doi.org/10.1001/jama.295.24.2867.
Saw SM, Tong L, Chua WH, Chia KS, Koh D, Tan DT. et al. Incidence and progression of myopia in Singaporean school children. Investig Opthalmology Vis Sci. 2005;46:51. https://doi.org/10.1167/iovs.04-0565.
Jones-Jordan LA, Sinnott LT, Cotter SA, Kleinstein RN, Manny RE, Mutti DO. et al. Time outdoors, visual activity, and myopia progression in Juvenile-onset myopes. Investig Opthalmology Vis Sci. 2012;53:7169. https://doi.org/10.1167/iovs.11-8336.
Saw SM, Nieto FJ, Katz J, Schein OD, Levy B, Chew SJ. Factors related to the progression of myopia in Singaporean children. Optom Vis Sci. 2000;77:549–54. http://www.ncbi.nlm.nih.gov/pubmed/11100893.
Li SM, Li H, Li SY, Liu LR, Kang MT, Wang YP. et al. Time outdoors and myopia progression over 2 years in Chinese children: the anyang childhood eye study. Investig Opthalmology Vis Sci. 2015;56:4734. https://doi.org/10.1167/iovs.14-15474.
Wu PC, Tsai CL, Wu HL, Yang YH, Kuo HK. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology. 2013;120:1080–5. https://doi.org/10.1016/j.ophtha.2012.11.009.
Saxena R, Vashist P, Tandon R, Pandey RM, Bhardawaj A, Gupta V, et al. Incidence and progression of myopia and associated factors in urban school children in Delhi: The North India Myopia Study (NIM Study). PLoS One. 2017;12:e0189774 https://doi.org/10.1371/journal.pone.0189774.
Zhou WJ, Zhang YY, Li H, Wu YF, Xu J, Lv S. et al. Five-year progression of refractive errors and incidence of myopia in school-aged children in western China. J Epidemiol. 2016;26:386–95. https://doi.org/10.2188/jea.JE20140258.
Lee SS, Lingham G, Sanfilippo PG, Hammond CJ, Saw SM, Guggenheim JA. et al. Incidence and progression of myopia in early adulthood. JAMA Ophthalmol. 2022;140:162–9. https://doi.org/10.1001/jamaophthalmol.2021.5067.
Funding
This work was supported by the Noor Ophthalmology Research Centre and Shahroud University of Medical Sciences (Grant Number: 960351).
Author information
Authors and Affiliations
Contributions
CL and MHE contributed to the conception and design of the study. CL and MHE performed the data analyses. CL wrote the manuscript. Manuscript revision: YL, MK, HH, AG, SSM and AF. Final approval of the manuscript: all authors.
Corresponding author
Ethics declarations
Competing interests
YLW is an employee of Essilor International, Singapore. Other authors have no conflict of interests to declare.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lanca, C., Emamian, M.H., Wong, Y.L. et al. Three-year change in refractive error and its risk factors: results from the Shahroud School Children Eye Cohort Study. Eye 37, 1625–1632 (2023). https://doi.org/10.1038/s41433-022-02219-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02219-8