Abstract
Objective
To introduce the Collaborative Ocular Tuberculosis Study (COTS) Calculator, an online clinical scoring system for initiating antitubercular therapy (ATT) in patients with ocular tuberculosis (TB).
Method
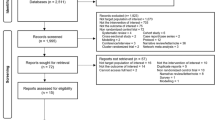
The COTS Calculator was derived from COTS Consensus (COTS CON) data, which has previously published consensus guidelines. Using a two-step Delphi method, 81 experts evaluated 486 clinical scenario-based questions, ranking their likelihood of initiating ATT in each specific scenario. Each scenario was a permutation of the results and/or availability of five following components—clinical phenotype, endemicity, two immunological (tuberculin skin test, interferon-γ release assay) and one radiological (chest X-Ray) test results—and a sixth component further stratifying three of the clinical phenotypes. The median scores and interquartile ranges (IQR) of each scenario were tabulated, representing the expert consensus on whether to initiate ATT in that scenario. The consensus table was encoded to develop the COTS Calculator.
Results
The COTS Calculator can be accessed online at: https://www.oculartb.net/cots-calc. The attending physician can select the conditions present in the patient, which will generate a median score from 1 to 5. 114 out of 486 scenarios (24%) deliberated had a median score of 5 indicating expert consensus to initiate ATT.
Conclusion
The COTS Calculator is an efficient, low-cost, evidence and experience-based clinical tool to guide ATT initiation. While it holds substantial promise in improving standard-of-care for ocular-TB patients, future validation studies can help to as certain its clinical utility and reliability.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are not publicly available. Nevertheless, interested researchers are invited to direct data access requests to the corresponding author.
References
World Health Organization. Global Tuberculosis Report. 2021. https://www.who.int/publications/i/item/9789240037021.
Bouza E, Merino P, Muñoz P, Sanchez-Carrillo C, Yáñez J, Cortés C. Ocular tuberculosis. A prospective study in a general hospital. Medicine 1997;76:53–61.
Biswas J, Badrinath SS. Ocular morbidity in patients with active systemic tuberculosis. Int Ophthalmol. 1995;19:293–8.
Basu S, Monira S, Modi RR, Choudhury N, Mohan N, Padhi TR, et al. Degree, duration, and causes of visual impairment in eyes affected with ocular tuberculosis. J Ophthalmic Inflamm Infect. 2014;4:3.
Shah JS, Shetty N, Shah SK, Shah NK. Tubercular uveitis with ocular manifestation as the first presentation of tuberculosis: a case series. J Clin Diagn Res. 2016;10:NR01–3.
Agrawal R, Gunasekeran DV, Raje D, Agarwal A, Nguyen QD, Kon OM, et al. For the Collaborative Ocular Tuberculosis Study Group; Global variations and challenges with tubercular uveitis in the collaborative ocular tuberculosis study. Investig Ophthalmol Vis Sci. 2018;59:4162–71.
Betzler BK, Gupta V, Agrawal R. Clinics of ocular tuberculosis: a review. Clin Exp Ophthalmol. 2021;49:146–60.
Gupta A, Sharma A, Bansal R, Sharma K. Classification of intra-ocular tuberculosis. Ocul Immunol Inflamm. 2015;23:7–13.
Lou SM, Montgomery PA, Larkin KL, Winthrop K, Zierhut M, Rosenbaum JT, et al. Diagnosis and treatment for ocular tuberculosis among uveitis specialists: the international perspective. Ocul Immunol Inflamm. 2015;23:32–9.
Lou SM, Larkin KL, Winthrop K, Rosenbaum JT, Uveitis Specialists Study Group. Lack of consensus in the diagnosis and treatment for ocular tuberculosis among uveitis specialists. Ocul Immunol Inflamm. 2015;23:25–31.
Gupta V, Gupta A, Rao NA. Intraocular tuberculosis—an update. Surv Ophthalmol. 2007;52:561–87.
Agrawal R, Gupta B, Gonzalez-Lopez JJ, Rahman F, Phatak S, Triantafyllopoulou I, et al. The role of anti-tubercular therapy in patients with presumed ocular tuberculosis. Ocul Immunol Inflamm. 2015;23:40–6.
Pefkianaki M, Westcott M, Liew G, Lee R, Pavesio C, et al. Diagnostic and therapeutic challenges. Retina. 2014;34:1247–52.
Agrawal R, Gunasekeran DV, Gonzalez-Lopez JJ, Cardoso J, Gupta B, Addison PKF, et al. Peripheral retinal vasculitis: analysis of 110 consecutive cases and a contemporary reappraisal of tubercular etiology. Retina. 2017;37:112–7.
Gupta V, Shoughy SS, Mahajan S, Khairallah M, Rosenbaum JT, Curi A, et al. Clinics of ocular tuberculosis. Ocul Immunol Inflamm. 2015;23:14–24.
Gupta A, Bansal R, Gupta V, Sharma A, Bambery P. Ocular signs predictive of tubercular uveitis. Am J Ophthalmol. 2010;149:562–70.
Ang M, Vasconcelos-Santos DV, Sharma K, Accorniti M, Sharma A, Gupta A, et al. Diagnosis of ocular tuberculosis. Ocul Immunol Inflamm. 2018;26:208–16.
Knecht PB, Papadia M, Herbort CP. Secondary choriocapillaritis in infectious chorioretinitis. Acta Ophthalmol. 2013;91:e550–5.
Agrawal R, Gunasekeran DV, Grant R, Agarwal A, Kon OM, Nguyen Q, et al. Clinical features and outcomes of patients with tubercular uveitis treated with antitubercular therapy in the Collaborative Ocular Tuberculosis Study (COTS)-1. JAMA Ophthalmol. 2017;135:1318–27.
Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al. A systematic review of rapid diagnostic tests for the detection of tuberculosis infection. Health Technol Assess. 2007;11:1–196.
Centers for Disease Control and Prevention. Updated guidelines for using interferon gamma release assays to detect mycobacterium tuberculosis infection—United States, 2010. MMWR Morb Mortal Wkly Rep. 2010;59:1–25.
Wang L, Turner MO, Elwood RK, Schulzer M, FitzGerald JM. A meta-analysis of the effect of Bacille Calmette Guérin vaccination on tuberculin skin test measurements. Thorax. 2002;57:804–9.
Centers for Disease Control and Prevention. Nationwide shortage of tuberculin skin test antigens: CDC recommendations for patient care and public health practice. MMWR Morb Mortal Wkly Rep. 2019;68:552–3.
Metcalfe JZ, Everett CK, Steingart KR, Cattamanchi A, Huang L, Hopewell PC, et al. Interferon-γ release assays for active pulmonary tuberculosis diagnosis in adults in low- and middle-income countries: systematic review and meta-analysis. J Infect Dis. 2011;204 Suppl 4:S1120–9.
Albini TA, Karakousis PC, Rao NA. Interferon-gamma release assays in the diagnosis of tuberculous uveitis. Am J Ophthalmol. 2008;146:486–8.
Kurup SK, Buggage RR, Clarke GL, Ursea R, Lim WK, Nussenblatt RB, et al. Gamma interferon assay as an alternative to PPD skin testing in selected patients with granulomatous intraocular inflammatory disease. Can J Ophthalmol. 2006;41:737–40.
Vasconcelos-Santos DV, Zierhut M, Rao NA. Strengths and weaknesses of diagnostic tools for tuberculous uveitis. Ocul Immunol Inflamm. 2009;17:351–5.
Jeong YJ, Lee KS. Pulmonary tuberculosis: up-to-date imaging and management. AJR Am J Roentgenol. 2008;191:834–44.
Sugita S, Ogawa M, Shimizu N, Morio T, Ohguro N, Nakai K, et al. Use of a comprehensive polymerase chain reaction system for diagnosis of ocular infectious diseases. Ophthalmology. 2013;120:1761–8.
Rosenbaum JT. To be or not TB? Br J Ophthalmol. 2014;98:999e1000.
Agarwal A, Agrawal R, Gunasekaran DV, Raje D, Gupta B, Agrawal K, et al. The Collaborative Ocular Tuberculosis Study (COTS)-1 Report 3: polymerase chain reaction in the diagnosis and management of tubercular uveitis: global trends. Ocul Immunol Inflamm. 2017;27:465–73.
Gunasekeran DV, Agrawal R, Agarwal A, Carreno E, Raje D, Aggarwal K, et al. The Collaborative Ocular Tuberculosis Study (COTS)-1: a multinational review of 251 patients with tubercular retinal vasculitis. Retina. 2019;39:1623–30.
Agrawal R, Gunasekeran DV, Agarwal A, Carreno E, Aggarwal K, Gupta B, et al. The Collaborative Ocular Tuberculosis Study (COTS)-1: a multinational description of the spectrum of choroidal involvement in 245 patients with tubercular uveitis. Ocul Immunol Inflamm. 2018;29:1–11.
Agrawal R, Testi I, Mahajan S, Yuen YS, Agarwal A, Rousselot A, et al. The Collaborative Ocular Tuberculosis Study (COTS) Consensus (CON) Group Meeting Proceedings. Ocul Immunol Inflamm. 2020. https://doi.org/10.1080/09273948.2020.171602.
Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311:376–80. https://doi.org/10.1136/bmj.311.7001.376.
McMillan SS, King M, Tully MP. How to use the nominal group and Delphi techniques. Int J Clin Pharm. 2016;38:655–62. https://doi.org/10.1007/s11096-016-0257-x.
Agrawal R, Testi I, Mahajan S, Yuen YS, Agarwal A, Kon OM, et al. Collaborative Ocular Tuberculosis Study consensus guidelines on the management of tubercular uveitis report 1: guidelines for initiating anti- tubercular therapy in tubercular choroiditis. Ophthalmology. 2021;128:266–76.
Agrawal R, Testi I, Bodaghi B, Barisani-Asenbauer T, Mccluskey P, Agarwal A, et al. Collaborative Ocular Tuberculosis Study Consensus Guidelines on the Management of Tubercular Uveitis Report 2: Guidelines for Initiating Antitubercular Therapy in Anterior Uveitis, Intermediate Uveitis, Panuveitis, and Retinal Vasculitis. Ophthalmology. 2021;128:277–87.
Derrick B, White P. Comparing two samples from an individual Likert question. Int J Math Stat. 2017;18:1–13.
Armstrong R. The midpoint on a five-point Likert-type scale. Percept Mot Skills. 1987;64:359–62. https://doi.org/10.2466/pms.1987.64.2.359.
The Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for sarcoidosis-associated uveitis. Am J Ophthalmol. 2021;228:142–51.
Collaborative Ocular Tuberculosis Study (COTS) Group. Standardization of Nomenclature for Ocular Tuberculosis—Results of Collaborative Ocular Tuberculosis Study (COTS) Workshop. Ocul Immunol Inflamm. 2019. https://doi.org/10.1080/09273948.2019.1653933.
Apgar V. A Proposal for a New Method of Evaluation of the Newborn Infant. Originally published in July 1953, volume 32, pages 250–259. Anesth Analg. 2015;120:1056–9.
Ibrahim LF, Hopper SM, Donath S, Salvin B, Babl FE, Bryant PA. Development and validation of a cellulitis risk score: the Melbourne ASSET score. Pediatrics. 2019;143:e20181420.
Ang M, Chee SP. Controversies in ocular tuberculosis. Br J Ophthalmol. 2017;101:6e9.
Gupta V, Gupta A, Rao NA. Intraocular tuberculosis—an update. Surv Ophthalmol. 2007;52:561e587.
Acknowledgements
All authors contributed to the intellectual development of this paper. RA and VG conceived and planned the study. ZL wrote the first draft of the paper. ZL and RA performed the literature review. RA, ZL, BB, IT, SM, AR, JHK, JRS, PM, QDN, CP and VG contributed to interpreting the results and provided critical feedback to the paper. The final version of the paper has been seen and approved by all authors.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
RA, ZL, BB, IT, SM, AR, JHK, JRS, PM, QDN, CP and VG report no competing interests, financial or propriety, in the subject matter or materials discussed in this paper. JHK is a consultant for Gilead Pharma, a company evaluating a treatment for non-infectious uveitis, and equity owner for Betaliq, a company developing an intraocular pressure-lowering treatment. RA is supported by a grant from the National Medical Research Council (NMRC) by Ministry of Health, Singapore, for the Clinician Scientist Award (CSA) from 2020 to 2023. He has not received funding for his work in this publication.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Agrawal, R., Ludi, Z., Betzler, B.K. et al. The Collaborative Ocular Tuberculosis Study (COTS) calculator—a consensus-based decision tool for initiating antitubercular therapy in ocular tuberculosis. Eye 37, 1416–1423 (2023). https://doi.org/10.1038/s41433-022-02147-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02147-7
This article is cited by
-
Infectious eye disease in the 21st century—an overview
Eye (2024)
-
Advanced drug delivery and therapeutic strategies for tuberculosis treatment
Journal of Nanobiotechnology (2023)