Abstract
Background
To test the hypothesis that elevated plasma levels of homocysteine (Hcy) and lipoprotein (a) (LPA) contribute to diabetic retinopathy (DR) associated with dysregulated lipid profile, dyslipidaemia, and kidney function.
Methods
A total of 83 patients with type 2 diabetes mellitus (T2DM) were enrolled in this prospective case-control study. Patients were categorized into those with no DR (DM), non-proliferative DR (NPDR), and proliferative DR (PDR). Age and sex-matched individuals with no diabetes were included in the control group. Biochemical tests, including fasting blood glucose (FBG), glycated hemoglobin (HbA1c), Hcy, LPA, lipid profile, and urine microalbumin (UMA), were evaluated.
Results
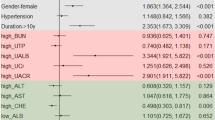
Hcy was negatively correlated with high-density lipoprotein-cholesterol (HDL-C) (p < 0.05), but positively correlated with [total cholesterol (TC)-HDL-C)/HDL-C] (p < 0.05), low-density lipoprotein cholesterol (LDL-C)/HDL-C (p < 0.05), and UMA (p < 0.05). Traditional risk factors, Hcy, arteriosclerosis-associated plasma indices, and UMA, resulted as the independent risk factors for the occurrence of DM and DR. After controlling for age, sex, duration of DM, and FBG, a multiple ordinal logistic regression model showed that LPA [OR = 2.90, 95% confidence interval (95% CI) 1.16–7.23, p = 0.023)], LDL-C (OR = 4.28, 95% CI 1.24–14.79, p = 0.021), and (TC-HDL-C)/HDL-C (OR = 1.92, 95% CI 1.05–3.53, p = 0.035) were risk factors for DM and DR.
Conclusions
Hcy and LPA contributed to DM and DR. Hcy was positively correlated with kidney dysfunction and the ratios of lipid profiles, and negatively with HDL-C, LPA, LDL-C, and (TC-HDL-C)/HDL-C resulted as predictors of the occurrence of DM and severity of DR.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
van Reyk DM, Gillies MC, Davies MJ. The retina: oxidative stress and diabetes. Redox Rep. 2003;8:187–92.
Zoungas S. Advance in context: The benefits, risks and feasibility of providing intensive glycaemic control based on gliclazide modified release. Diabetes Obes Metab. 2020;22:5–11.
Chico A, Pérez A, Córdoba A, Arcelús R, Carreras G, de Leiva A, et al. Plasma homocysteine is related to albumin excretion rate in patients with diabetes mellitus: a new link between diabetic nephropathy and cardiovascular disease? Diabetologia. 1998;41:684–93.
Nardulli M, Durlach V, Pepe G, Anglés-Cano E. Mechanism for the homocysteine-enhanced antifibrinolytic potential of lipoprotein(a) in human plasma. Thromb Haemost. 2005;94:75–81.
Zhang L, Li Z, Xing C, Ma X, Xu R. The protective mechanism of folic acid on hyperhomocysteinemia-related arterial injury in spontaneously hypertensive rats: Folic acid against arterial inflammation. Vascular. 2021. https://doi.org/10.1177/17085381211036549.
Zhang XY, Qiu BJ, Wang QY, Sivaprasad S, Wang YH, Zhao L, et al. Dysregulated serum lipid metabolism promotes the occurrence and development of diabetic retinopathy associated with upregulated circulating levels of VEGF-A, VEGF-D, and PlGF. Front Med. 2021. https://doi.org/10.3389/fmed.2021.779413.
Wells JA, Glassman AR, Ayala AR, Jampol LM, Bressler NM, Bressler SB, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema: two-year results from a comparative effectiveness randomized clinical trial. Ophthalmology. 2016;123:1351–9.
Bressler SB, Ayala AR, Bressler NM, Melia M, Qin H, Ferris FL 3rd, et al. Persistent macular thickening after ranibizumab treatment for diabetic macular edema with vision impairment. JAMA Ophthalmol. 2016;134:278–85.
National cholesterol education program (NCEP) expert panel on detection e, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421.
Sacco RL, Adams R, Albers G, Alberts MJ, Benavente O, Furie K, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline. Circulation. 2006;113:e409–449.
Anderson TJ, Grégoire J, Pearson GJ, Barry AR, Couture P, Dawes M, et al. 2016 canadian cardiovascular society guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol. 2016;32:1263–82.
Brazionis L, Rowley K, Itsiopoulos C, Harper CA, O’Dea K. Homocysteine and diabetic retinopathy. Diabetes Care. 2008;31:50–56.
Pushpakumar S, Kundu S, Sen U. Endothelial dysfunction: the link between homocysteine and hydrogen sulfide. Curr Med Chem. 2014;21:3662–72.
Austin RC, Lentz SR, Werstuck GH. Role of hyperhomocysteinemia in endothelial dysfunction and atherothrombotic disease. Cell Death Differ. 2004;11:56–64.
Yan TT, Li Q, Zhang XH, Wu WK, Sun J, Li L, et al. Homocysteine impaired endothelial function through compromised vascular endothelial growth factor/Akt/endothelial nitric oxide synthase signalling. Clin Exp Pharm Physiol. 2010;37:1071–7.
Moore P, El-sherbeny A, Roon P, Schoenlein PV, Ganapathy V, Smith SB. Apoptotic cell death in the mouse retinal ganglion cell layer is induced in vivo by the excitatory amino acid homocysteine. Exp Eye Res. 2001;73:45–57.
Liao D, Tan H, Hui R, Li Z, Jiang X, Gaubatz J, et al. Hyperhomocysteinemia decreases circulating high-density lipoprotein by inhibiting apolipoprotein A-I protein synthesis and enhancing HDL cholesterol clearance. Circ Res. 2006;99:598–606.
Devlin AM, Lentz SR. ApoA-I: a missing link between homocysteine and lipid metabolism? Circ Res. 2006;98:431–3.
Qujeq D, Omran TS, Hosini L. Correlation between total homocysteine, low-density lipoprotein cholesterol and high-density lipoprotein cholesterol in the serum of patients with myocardial infarction. Clin Biochem. 2001;34:97–101.
Momin M, Jia J, Fan F, Li J, Dou J, Chen D, et al. Relationship between plasma homocysteine level and lipid profiles in a community-based Chinese population. Lipids Health Dis. 2017;16:54.
Wang T, Wang Q, Wang Z, Xiao Z, Liu L. Diagnostic value of the combined measurement of serum hcy, serum cys C, and urinary microalbumin in type 2 diabetes mellitus with early complicating diabetic nephropathy. ISRN Endocrinol. 2013. https://doi.org/10.1155/2013/407452.
Zoccali C, Jager KJ. Hyperhomocysteinemia: a renal and cardiovascular risk factor? Nat Rev Nephrol. 2010;6:695–6.
Fairweather D. Sex differences in inflammation during atherosclerosis. Clin Med Insights Cardiol. 2014;8:49–59.
Abdella NA, Mojiminiyi OA, Akanji AO, Moussa MA. Associations of plasma homocysteine concentration in subjects with type 2 diabetes mellitus. Acta Diabetol. 2002;39:183–90.
Kim J, Ahn CW, Fang S, Lee HS, Park JS. Association between metformin dose and vitamin B12 deficiency in patients with type 2 diabetes. Medicine. 2019. https://doi.org/10.1097/md.0000000000017918.
Chapman LE, Darling AL, Brown JE. Association between metformin and vitamin B(12) deficiency in patients with type 2 diabetes: a systematic review and meta-analysis. Diabetes Metab. 2016;42:316–27.
Elhadd T, Ponirakis G, Dabbous Z, Siddique M, Chinnaiyan S, Malik RA. Metformin use is not associated with B(12) deficiency or neuropathy in patients with type 2 diabetes mellitus in Qatar. Front Endocrinol. 2018;9:248.
Lauriola M, D’Onofrio G, Ciccone F, Germano C, Cascavilla L, Paris F, et al. Relationship of homocysteine plasma levels with mild cognitive impairment, alzheimer’s disease, vascular dementia, psychobehavioral, and functional complications. J Alzheimers Dis. 2021;82:235–48.
Liu M, Fan F, Liu B, Jia J, Jiang Y, Sun P, et al. Joint effects of plasma homocysteine concentration and traditional cardiovascular risk factors on the risk of new-onset peripheral arterial disease. Diabete Metab Synd Ob. 2020;13:3383–93.
Qin X, Huo Y. H-Type hypertension, stroke and diabetes in China: opportunities for primary prevention. J Diabetes. 2016;8:38–40.
Chori BS, Danladi B, Inyang BA, Okoh MP, Nwegbu MM, Alli AL, et al. Hyperhomocysteinemia and its relations to conventional risk factors for cardiovascular diseases in adult nigerians: the REMAH study. BMC Cardiovasc Disor. 2021;21:102.
de Groot PG, Willems C, Boers GH, Gonsalves MD, van Aken WG, van Mourik JA. Endothelial cell dysfunction in homocystinuria. Eur J Clin Invest. 1983;13:405–10.
Kostner KM, März W, Kostner GM. When should we measure lipoprotein (a)? Eur Heart J. 2013;34:3268–76.
Chopra R, Saramma JG, Mary J, Rebecca A. Lipoprotein(a) as a risk factor for diabetic retinopathy in patients with type 2 diabetes mellitus. Indian J Ophthalmol. 2007;55:195–8.
Tu WJ, Liu H, Liu Q, Cao JL, Guo M. Association between serum lipoprotein(a) and diabetic retinopathy in han Chinese patients with type 2. diabetes J Clin Endocr Metab. 2017;102:2525–32.
Chandni R, Ramamoorthy KP. Lipoprotein(a) in type 2 diabetic subjects and its relationship to diabetic microvascular complications. World J Diabetes. 2012;3:105–9.
Gazzaruso C, Coppola A, Montalcini T, Baffero E, Garzaniti A, Pelissero G, et al. Lipoprotein(a) and homocysteine as genetic risk factors for vascular and neuropathic diabetic foot in type 2 diabetes mellitus. Endocrine. 2012;41:89–95.
Funding
This work was supported by the National Natural Science Foundation of China [Grant 81570850 and 82070988] and the Ministry of Science and Technology Foundation of China [Grant 2016YFC1305604].
Author information
Authors and Affiliations
Contributions
XZ contributed to conception and design of the study, drafted and revised the manuscript and perform statistical analysis. XC and YN organized the database, performed the experiments and statistical analysis and drafted the manuscript. ZG, AF and XC performed the statistical analysis. QW, BQ, RX and YW helped to enroll patients. All authors contributed to manuscript revision, read, and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, X., Zhang, X., Nie, Y. et al. Circulating level of homocysteine contributes to diabetic retinopathy associated with dysregulated lipid profile and impaired kidney function in patients with type 2 diabetes mellitus. Eye 37, 1383–1389 (2023). https://doi.org/10.1038/s41433-022-02144-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02144-w