Abstract
Geographic atrophy (GA) is currently an untreatable condition. Emerging evidence from recent clinical trials show that anti-complement therapy may be a successful treatment option. However, several trials in this therapy area have failed as well. This raises several questions. Firstly, does complement therapy work for all patients with GA? Secondly, is GA one disease? Can we assume that these failed clinical trials are due to ineffective interventions or are they due to flawed clinical trial designs, heterogeneity in GA progression rates or differences in study cohorts? In this article we try to answer these questions by providing an overview of the challenges of designing and interpreting outcomes of randomised controlled trials (RCTs) in GA. These include differing inclusion-exclusion criteria, heterogeneous progression rates of the disease, outcome choices and confounders.
摘要
地图样萎缩 (Geographic atrophy, GA) 是一种目前尚无法治愈的疾病。最近来自临床试验的新兴证据表明, 抗补体治疗可能成为一种有效的治疗方式。然而, 基于该治疗方式的几项试验都失败了。这就提出了几个问题。首先, 补体治疗是否适用于所有GA患者? 其次, GA是一种疾病吗? 我们是否可以提出几个假设: 这些临床试验失败是因为干预措施无效还是因为临床试验设计有缺陷? GA进展率是否具有异质性或研究队列内是否存在差异? 在本文中, 我们总结了这些GA随机对照试验 (RCT) 在试验设计和结果解读中面临的挑战, 其中包括不同的纳入-排除标准、疾病的异质性进展率、结局选择和混杂因素, 并试图以此来回答这些问题。
Similar content being viewed by others
Introduction
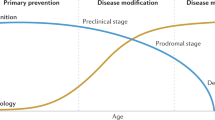
Geographic atrophy (GA) is currently transitioning from an untreatable condition to a disease area of major interest owing to emerging evidence from clinical trials that therapies can reduce its growth rate over time [1]. However, several pivotal trials on the same class of therapies have failed. For example, complement pathway in AMD has been researched substantially over the last fifteen years and recently, anti-complement agents have shown some evidence of success in reduction of growth rate of GA lesion compared to sham in pivotal trials [2]. However, other complement inhibitors have failed all together or after promising results in early phase trials [3]. This begs the question: Is GA one disease? To put it in another way, are the investigational products only biologically effective in certain GA subtypes and if so, is it by chance that these subtypes represent a larger cohort in some trials and not others? There is no doubt that both basic and clinical research have increased our understanding of the pathogenesis and progression rates of GA. However, the results of clinical trials highlight gaps in our knowledge. Can we assume that failed clinical trials in GA are due to ineffective interventions? Or should we dwell deeper into the subtlety in clinical trial designs, heterogeneity in GA progression rates or differences in study cohorts?
We aimed to study these differences by examining some of the recent Phase II/III clinical trials on GA and provide a perspective on each question raised.
Methods
Clinical trials reporting on GA progression and factors associated with GA progression were identified via a PubMed literature search and clinical trials.gov using the terms “geographic atrophy,” “atrophy,” “macular degeneration,” “progression,” “enlargement,” and “growth”. Primary literature search on PubMed for GA, also included search terms “complement cascade, “complement inhibitors”, “gene therapy” in age-related macular degeneration. All searches were collated and sorted for relevance. We excluded review articles, case studies, pilot studies (defined as N < 16), papers reporting on macular atrophy in neovascular AMD, diseases other than AMD, preclinical studies, pathophysiology/histology of GA and non-English articles.
Results
Details of the interventions for geographic atrophy that are currently being investigated in clinical trials or are in the pipeline are shown in Table 1. Clinical trials on these agents, if available, show variations in eligibility criteria. These include lesion characteristics, disease state of the fellow eye, visual function, age range of included patients and their genetic disposition. In addition, mode of delivery and mechanisms of actions of interventions and primary outcome measures differed.
Discussion
Eligibility criteria
GA lesion characteristics
One of the key inclusion criteria for clinical trials is the lesion size of GA. Most trials include GA sizes ranging between ≥2.5 and ≤17.5 mm2. However, Elamipretide (ReCLAIM2, NCT03891875, Stealth Bio) is being evaluated on a cohort with smaller GA size ≥0.05 and ≤10.16 mm2 while FOCUS trial (GT005, NCT03846193, Gyroscope) on gene therapy have included a wider range of lesion sizes from ≥1.25 and ≤17.5 mm2 [4, 5]. When comparing outcomes of GA trials, it is important to note these differences [6, 7]. It may be that when the intervention does not require frequent intravitreal dosing or may be self-administered, the trial design may focus on earlier disease or extrafoveal GA or those with smaller lesion sizes. Therefore, the outcomes of these patients will differ to those of fovea-involving large lesions. It is understandable that a safety or dose response study such as FOCUS that is evaluating a subretinal delivery of a recombinant non-replicating adeno-associated viral (AAV) vector encoding a human complement factor would require a wider range of lesion sizes [5, 8]. However, trials that include large range of lesion sizes can result in wider standard deviations in progression rates and results of a study cohort may be more difficult to decipher [9]. In these studies, homogeneous smaller cohorts or individual outcomes may need to be identified to understand the effect of the intervention.
GA growth rates
Although the median growth rate of GA is about 1.78 mm2/year, there are significant variability in individual enlargement rates in the natural history study by Sunness et al. [10,11,12]. In fact, only a small proportion of lesion sizes fell within the average range of growth rate [12]. Fleckenstein et al. reviewed the annualised growth rate and highlighted the inter and intraindividual variations in enlargement rates when only the baseline lesion size is considered [13]. As there are several well-characterised GA cohorts that include multimodal imaging, it may be appropriate to pool them and identify homogeneous cohorts with similar growth rates. These cohorts can include natural history studies and sham arms and, in some cases, the failed intervention arms. As an example, Mones and Biarnes demonstrated three GA phenotypes with different progression rates at ≥6 months based on data driven cluster analysis of GA lesions in 77 eyes [14]. With new reports on OCT classification of atrophy, it is now timely to re-visit heterogeneity of GA progression rates to inform future clinical trials [12, 15, 16]. In addition, for trials that have shown some success in reducing growth rates compared to the natural history, an opportunity is provided to identify ‘super responders’ in terms of reduced growth rate lesser than the lowest 95% confidence interval of the rates observed in the sham group.
Another consideration is the focality of lesions: Multifocal GA lesions progress faster than unifocal GA [17, 18]. The DERBY/ OAKS (APL-2, NCT03525613, Apellis), FILLY (APL-2, NCT02503332, Apellis) and GATHER-1 (Zimura, NCT02686658, IVERIC Bio) recruited multifocal GA lesions, with at least one focal lesion being at least 1.25 mm2 (0.5 disc areas) [1, 19, 20]. Many other on-going trials have not included information on this inclusion criterion in clinical trials.gov. Unless stratified by lesion size and focality, these do have implications [18]. Another lesion characteristic that may influence growth rate is the presence of perilesional fundus autofluorescence (FAF) [21, 22]. This may represent lipofuscin accumulation in sick RPE cells or heaped RPE cells at the expanding rim of GA [23, 24]. This sign is a predictor of faster growth compared to lesions without this sign. The DERBY and OAKS (APL-2, NCT03525613, Apellis), FILLY (APL-2, NCT02503332, Apellis) and GATHER-1 (Zimura, NCT02686658, IVERIC Bio) included this sign as an eligibility criterion but this is not a universal requirement for GA trials [1, 19, 20]. Another consideration is the proportion of foveal and non-foveal involving GA in each trial cohort [25]. For example, DERBY and OAKS (APL-2, NCT03525613, Apellis) included both groups while GATHER-1 (Zimura, NCT02686658, IVERIC Bio) focused on non-foveal involving GA. Non-foveal, unifocal GA is likely to represent early disease while foveal involvement indicate long-standing disease [18, 26]. As both C3 and C5 inhibition appeared to be more effective in reducing growth rate of non-foveal involving lesions, it raises the question whether complement activation is more relevant in early disease than late disease, or whether established GA does not grow as fast hence more difficult to see a treatment effect. Non-foveal GA that extends towards the periphery grow faster than those that grow towards the fovea [27]. Therefore, these directional growths may need to be considered when correlating growth rates and functional changes in GA trials [28, 29]. Taken together, if there are two eyes with similar sized GA lesions, but one is multifocal, non-foveal and has perilesional hyperautofluorescence, it is likely to progress faster than the eye with a unifocal, foveal involving without any rim hyperautofluorescence. Therefore, considering stratifying by baseline lesion size alone may not be sufficient. If these lesion characteristics are imbalanced between the sham and intervention arm, these may affect the primary outcome of lesion growth. Other lesions that have not been considered in clinical trials to date is the stratification of arms based on the presence of subretinal drusenoid deposits (SDD) [30]. These are associated with rod intercept delays suggesting rod photoreceptor dysfunction [31, 32]. These lesions may also represent irreversible functional losses despite its association with GA progression rates [33].
Fellow-eye features
All GA trials have ensured exclusion of any current or prior choroidal neovascularisation (CNV) in the study eyes at baseline. However, including patients with prior or current neovascular AMD in the fellow eye increases the risk of developing CNV in the study eye while being treated with the investigational product for GA [34]. The FILLY study included eyes with neovascular AMD in fellow eye [6]. The study showed a higher rate of new-onset CNV in the intervention (Pegcetacoplan, APL-2) arm compared to sham [35]. The question is whether this is due to the intervention or is this the expected natural history of neovascular AMD? A dose related increase in CNV was also seen in GATHER-1 study (Zimura, C5 inhibitor) but the incidence of CNV was lower (9.0–9.6%) compared to that of APL-2 (8.9–20.9%). The reason for this difference in CNV rates between a C3 and C5 inhibitor remains unclear. It may be that C5 inhibition is further downstream in the alternative pathway, which may minimize the disturbance of the C3-mediated complement homeostasis. However, if the FILLY intervention arm included those with no neovascular AMD in fellow eye in a subanalysis, the rate of CNV development in FILLY and GATHER-1 are similar [2]. In the GATHER-1 study on Zimura, the incidence of CNV in the untreated fellow eye was 11 patients (3.8%), and in the study eye, it was 3 patients (2.7%) in the sham control group, 2 patients (7.7%) in the Zimura 1 mg group, 8 patients (11.9%) in the Zimura 2 mg group, and 13 patients (15.7%) in the Zimura 4 mg group [20]. It is also interesting to note that the rate of CNV in DERBY/OAKS (APL-2, NCT03525613, Apellis) were lower than in the FILLY trial (Phase 2 trial of the same intervention), despite no differences in eligibility criteria between these Phase 2 and 3 trials on APL-2 in clinical trials.gov. These conflicting figures challenge our current understanding of the effect of complement inhibitors on onset of CNV.
The pivotal Phase 3 trials of both these agents (DERBY and OAKS (C3 Inhibitor, NCT03525613) and GATHER-2 (C5 inhibitor, NCT04435366) have retained eyes that converted to neovascular AMD during the study while being treated for GA, instead of censoring them from the analysis [19, 36]. Although it adds value to maintain the power of the study, development of CNV leads to reduction of drusen and the reporting of GA growth rate may be confounded by the influence of CNV related atrophy and anti-VEGF therapy.
Another point to consider is that GA progression rates in these eyes with neovascular AMD in fellow eye are slower than those with bilateral GA [11, 37, 38]. As such, the disease status in the fellow eye must also be considered if GA growth rate is the primary outcome. GA eyes with intermediate AMD in the fellow eye show slower GA growth rates compared to eyes with bilateral GA [38].
Visual function
Most trials whether focussed on both foveal and non-foveal GA or only on non-foveal GA had an eligibility criterion of ≥24 ETDRS letters (Snellen 20/320) [2]. However, Elamipretide trial (ReCLAIM2, NCT03891875, Stealth Bio) included only GA eyes with ≥55 ETDRS letters, emphasizing that the eligibility criteria of this trial differ from the pivotal complement trials to date [4]. In addition, the FOCUS trial (GT005, NCT03846193, Gyroscope) have included those with GA and BCVA ≤ 50 letters in cohorts 1to 3 and ≥34 letters in cohorts 4–6 [5]. As BCVA shows no correlation to GA growth, these differences in BCVA criteria are unlikely to influence primary outcome of GA growth reduction [26, 39]. However, as the primary aim of any intervention is to improve patient related outcomes and visual function, secondary outcome on preventing vision loss may differ between trials due to the BCVA inclusion-exclusion criteria.
Natural history studies have shown that GA is associated with low luminance visual acuity losses [18]. In addition, low luminance deficit is a marker of future visual loss [40]. Low luminance visual acuity losses are best highlighted in non-fovea involving GA and the progression of non-foveal GA may partly explain the worsening of this visual function [41, 42]. In addition, subretinal drusenoid deposits are strongly associated with low luminance deficit and likely signify rod dysfunction and these eyes also have a faster progression rate [41]. These findings suggest that a GA subtype with subretinal drusenoid deposits may represent a more irreversible end of the spectrum.
As BCVA does not correspond directly to GA lesion enlargement due to possible foveal sparing, alternative assessments are being explored to capture the relationship between anatomic progression and visual function decline, including microperimetry, reading speed assessments, and patient-reported outcomes need to be explored further [43,44,45]. A recent report from Holz group have shown how if GA involves the nasal side of fovea, it is likely to affect reading speed more than the right side [46, 47]. However, the Food and Drug Administration (FDA) does not currently accept this endpoint and further studies are required on functional changes in GA.
Age of patients
Some GA trials included patients aged 50 years or above while others have gone to as high as 65 years or above at baseline (AAVCAGsCD59, NCT0314499, J&J and Hemera) [48]. In addition, the age range is large in most trials extending from 50 to late 90 s. It is unclear whether age at recruitment is by itself an independent risk factor or whether younger age groups are likely to have non-foveal GA or earlier disease compared to participants in their late 90 s. Although local age-related differences in C3 and C5 are not well-defined, circulating C5 increases with age in contrast to age related decrease in factor D and C3 [49]. This may be an area worth further investigation. Prior growth rate of GA also determines future growth rate.
Genetic variants
Genetic factors account for approximately 71–80% of the risks in prediction models of advanced AMD [50,51,52]. The common genetic variants of CFH, CFI, C3, and C2/CFB in the alternative complement pathway, may account for 57% of known disease risk variants [52].
However, the CHROMA and SPECTRI studies on lampalizumab (Factor D inhibitor) showed that the progression rates of GA lesions in carriers of the complement factor I (CFI) risk allele did not differ significantly to their CFI-negative counterparts [3]. Based on the CFI inhibition studies alone, it seems irrelevant at present to include genetic variants as eligibility criteria for GA treatment trials. However, other studies are needed to further inform this decision [3].
Intervention types
When we consider complement inhibitors, there are GA trials that inhibit C3, C1q, C5, Factor B (IONIS-FB-LRx, NCT03815825, Ionis) and Factor D [1, 36, 53, 54]. Some have showed efficacy, and some have not. The aim of C5 inhibitors is to block C5 cleavage to decrease formation of pro-inflammatory drive by C5a and MAC formation and NLRP3 inflammasome. However, we have two failed trials on C5 inhibition and one with early promising result [20, 36, 53]. The trial on intravitreal LFG316 or Tesidolumab (NCT01527500, Novartis) a fully-human, high affinity C5 antibody showed no anatomical or visual acuity effect compared to sham at 18 months [55]. Similarly, eculizumab is another C5 monoclonal antibody that was administered intravenously every other month for 6 months in GA patients and followed up for another 6 months but failed to show any difference in GA progression rates compared to sham [53]. However, Zimura, also a C5 inhibitor is a chemically synthesized aptamer (oligonucleotide-based ligand) and showed positive Phase 2b/3 results with a reduction of mean rate of GA growth over 12 months by 27.38% (p = 0.0072) for the Zimura 2 mg group and 27.81% (p = 0.0051) for the Zimura 4 mg group compared to the corresponding sham control group [20]. Can the results be explained by differences in GA lesion characteristics or are there other explanations? The failure of intravenous eculizumab may be explained by low drug concentration at target tissue, such as retinal pigment epithelial cells (RPE) due to systemic delivery. However, one would expect a monoclonal antibody (LFG316) to have meaningful vitreous half-life and we could assume that the pre-clinical data would have shown significant drug level at RPE before progressing to clinical trials. So, is it possible that pegylation is more advantageous than monoclonal antibodies as both APL-2 and Zimura are pegylated. Could aptamers be more stable than monoclonal antibody, although there is no evidence that is the case?
Primary endpoints
The primary endpoint of most of the GA trials is the change in total area of GA lesions as measured by FAF. However, the time points differ: APL-2 (NCT02503332) −12 months; GT005 (NCT03846193) − 48 months; NGM621 (NCT04014777) − 48 months; IONIS-FB-LRX (NCT03815825) − 49 months; HMR59–24 months (NCT04358471) and RG6147 (NCT03295877) 72 weeks [8, 19, 48, 54, 56, 57]. Both Zimura and ALK-001 studies have mean rate of change in GA on FAF as the primary endpoint [20, 58]. Recently, under special protocol assessment by the FDA, the GATHER 2 primary endpoint has been changed from mean rate of change of GA area over 12 months (considering 3 timepoints -baseline, 6 and 12 months) to mean rate of growth (slope) in at least these three timepoints. This amended analysis assumes a constant rate of growth of GA lesions over the study period [59]. This may apply to the primary outcome of all future pivotal GA trials.
When we consider visual function outcomes, BCVA change is a co-primary for ALK-001 at 48 weeks while elamipretide has chosen low luminance visual acuity as an endpoint at 48 weeks. In the FILLY study, C3 inhibitor did not show any significant change in BCVA or LLVA between arms and in GATHER studies that included only non-foveal GA, the higher dose of C5 inhibitor (4 mg) showed similar BCVA outcome to sham at 12 and 18 months despite a reduction of GA growth rate of 27.81% and 29.97% versus sham at these timepoints [1, 20]. Reduction of growth rate does not equate to visual function benefit, but these results question the lesion characteristics included in these arms. Was the GA growth to periphery reduced more profoundly? Alternatively, it might take longer before the effect on visual acuity is shown by delaying foveal involvement.
An in-depth analysis of the criteria used in GA trials highlights the major need to refine and improve patient selection. GA modelling studies should be able to differentiate fast versus slow progressors based on multiple lesion characteristics and not only lesion size. Predictors of direction of growth rate may add value to selecting the patient cohort. Although functional changes may not be appreciated in short term trials of 12–18 months duration, post-approval studies may be designed to confirm functional benefit as well as the subgroup that would benefit most from an intervention.
Conclusion
Here, we provide an overview of the challenges of designing and interpreting outcomes of randomised controlled trials (RCTs) in GA. These include differing inclusion-exclusion criteria, heterogeneous progression rates of the disease, outcome choices and confounders. Given the need for as many drugs to be approved for GA, it is important to encourage simple anatomical endpoints for drug approval. Although drugs should be evaluated on generalisable population, broad study eligibility criteria might lead to an effective drug failing to meet its primary endpoint and not obtaining approval. Pathway specific inclusion/exclusion criteria might lead to more positive study results. Outcomes of RCTs generally represent the average treatment effects across all included patients. A neutral average effect may represent benefit in some patients and not others and a beneficial average effect may differ in magnitude across subgroups. The risk of adverse events may also vary based on type of route of intervention albeit the drugs being of the same mechanisms of actions.
Use of these drugs in routine clinical practice and acquiring good real-world datasets with multimodal imaging will aid in understanding these GA subtypes and subtype-based interventions. In particular, one major unanswered question from these clinical trial results is whether GA is one disease entity? Having had mixed success with anti-complement trials, does it inform us that not all GAs are complement dependent? There may be GA lesions that may be explained by other pathogenesis such as lipofuscin overload resembling late onset Stargardt disease. These may likely respond more to A2E/ lipofuscin inhibitors than complement inhibitors. Eyes with GA and SDD did adversely in the LEAD trial, and they are associated with delayed rod intercept time due to rod loss [60, 61]. Would neuroprotection be a better option for eyes with SDD and/or outer nuclear layer thinning? Or do these GA lesions occur secondary to impaired visual cycle or mitochondrial defect? Targeting these pathophysiological pathways might be rewarding. Some GA lesions are due to thick Bruch’s membrane resembling Sorsby Fundus Dystrophy [62]. A drug that can remove lipid from lipid laden Bruch’s membrane might be an option for these subtypes. Finally, chromosome 10 disease (ARMS2/HTRA1) is associated with retinal thinning and might need a different intervention.
The recent data from AREDS suggest that GA cannot easily be subtyped by genotypes or phenotypes and that genetic information added little to the high predictive value of baseline severity of AMD for disease progression [63, 64]. In contrast, the EYE-RISK Consortium showed a stronger genetic association with late AMD [65]. Is it possible that AREDS2 was a study of intermediate AMD with specific inclusion criteria that were biased towards drusen associated GA while the European study was population based and allowed more diverse population? In reality, all these pathophysiological pathways might play some role in an individual patient pointing towards a need for personalised medicine.
There remain several avenues of research to be conducted to better understand GA especially in disease stratification so that novel interventions may be evaluated more efficiently and effectively.
References
Liao DS, Grossi FV, El Mehdi D, Gerber MR, Brown DM, Heier JS, et al. Complement C3 inhibitor pegcetacoplan for geographic atrophy secondary to age-related macular degeneration: a randomized phase 2 trial. Ophthalmology. 2020;127:186–95.
Halawa OA, Lin JB, Miller JW, Vavvas DG. A review of completed and ongoing complement inhibitor trials for geographic atrophy secondary to age-related macular degeneration. J Clin Med. 2021;10:2580.
Holz FG, Sadda SR, Busbee B, Chew EY, Mitchell P, Tufail A, et al. Efficacy and safety of lampalizumab for geographic atrophy due to age-related macular degeneration: chroma and spectri phase 3 randomized clinical trials. JAMA Ophthalmol. 2018;136:666–77.
ReCLAIM-2 Study to evaluate safety, efficacy & pharmacokinetics of elamipretide in subjects with AMD with non-central GA. 2022; Available from: https://ClinicalTrials.gov/show/NCT03891875.
FocuS: First in human study to evaluate the safety and efficacy of GT005 administered in subjects with Dry AMD. 2022 10 January 2022; Available from: https://ClinicalTrials.gov/show/NCT03846193.
Steinle NC, Pearce I, Monés J, Metlapally R, Saroj N, Hamdani M, et al. Impact of baseline characteristics on geographic atrophy progression in the FILLY trial evaluating the complement C3 inhibitor pegcetacoplan. Am J Ophthalmol. 2021;227:116–24.
Shen LL, Sun M, Ahluwalia A, Young BK, Park MM, Del Priore LV. Geographic atrophy growth is strongly related to lesion perimeter: unifying effects of lesion area, number, and circularity on growth. Ophthalmol Retin. 2021;5:868–78.
Ellis S, Buchberger A, Holder J, Orhan e, Hughes J. GT005, a gene therapy for the treatment of dry age-related macular degeneration (AMD). Investigative Ophthalmol Vis Sci. 2020;61:2295.
Monés J, Biarnés M. The rate of progression of geographic atrophy decreases with increasing baseline lesion size even after the square root transformation. Transl Vis Sci Technol. 2018;7:40.
Sunness JS, Gonzalez-Baron J, Applegate CA, Bressler NM, Tian Y, Hawkins B, et al. Enlargement of atrophy and visual acuity loss in the geographic atrophy form of age-related macular degeneration. Ophthalmology. 1999;106:1768–79.
Sunness JS, Margalit E, Srikumaran D, Applegate CA, Tian Y, Perry D, et al. The long-term natural history of geographic atrophy from age-related macular degeneration: enlargement of atrophy and implications for interventional clinical trials. Ophthalmology. 2007;114:271–7.
Wang J, Ying GS. Growth rate of geographic atrophy secondary to age-related macular degeneration: a meta-analysis of natural history studies and implications for designing future trials. Ophthalmic Res. 2021;64:205–15.
Fleckenstein M, Mitchell P, Freund KB, Sadda S, Holz FG, Brittain C, et al. The progression of geographic atrophy secondary to age-related macular degeneration. Ophthalmology. 2018;125:369–90.
Monés J, Biarnés M. Geographic atrophy phenotype identification by cluster analysis. Br J Ophthalmol. 2018;102:388–92.
Sadda SR, Guymer R, Holz FG, Schmitz-Valckenberg S, Curcio CA, Bird AC, et al. Consensus definition for atrophy associated with age-related macular degeneration on OCT: classification of atrophy report 3. Ophthalmology. 2018;125:537–48.
Schmitz-Valckenberg S, Sadda S, Staurenghi G, Chew EY, Fleckenstein M, Holz FG, et al. GEOGRAPHIC ATROPHY: semantic considerations and literature review. Retina. 2016;36:2250–64.
Shen LL, Sun M, Grossetta Nardini HK, Del Priore LV. Progression of unifocal versus multifocal geographic atrophy in age-related macular degeneration: a systematic review and meta-analysis. Ophthalmol. Retina. 2020;4:899–910.
Holekamp N, Wykoff CC, Schmitz-Valckenberg S, Monés J, Souied EH, Lin H, et al. Natural history of geographic atrophy secondary to age-related macular degeneration: results from the prospective Proxima A and B Clinical Trials. Ophthalmology. 2020;127:769–83.
A Study to compare the efficacy and safety of intravitreal APL-2 therapy with sham injections in patients with geographic atrophy (GA) secondary to age-related macular degeneration. 2022 10 January 2022; Available from: https://ClinicalTrials.gov/show/NCT03525613.
Jaffe GJ, Westby K, Csaky KG, Monés J, Pearlman JA, Patel SS, et al. C5 inhibitor avacincaptad pegol for geographic atrophy due to age-related macular degeneration: a randomized pivotal phase 2/3 trial. Ophthalmology. 2021;128:576–86.
Holz FG, Bindewald-Wittich A, Fleckenstein M, Dreyhaupt J, Scholl HP, Schmitz-Valckenberg S, et al. Progression of geographic atrophy and impact of fundus autofluorescence patterns in age-related macular degeneration. Am J Ophthalmol. 2007;143:463–72.
Fleckenstein M, Schmitz-Valckenberg S, Martens C, Kosanetzky S, Brinkmann CK, Hageman GS, et al. Fundus autofluorescence and spectral-domain optical coherence tomography characteristics in a rapidly progressing form of geographic atrophy. Invest Ophthalmol Vis Sci. 2011;52:3761–6.
Rudolf M, Vogt SD, Curcio CA, Huisingh C, McGwin G JR, Wagner A, et al. Histologic basis of variations in retinal pigment epithelium autofluorescence in eyes with geographic atrophy. Ophthalmology. 2013;120:821–8.
Ach T, Huisingh C, McGwin G JR, Messinger JD, Zhang T, Bentley MJ, et al. Quantitative autofluorescence and cell density maps of the human retinal pigment epithelium. Invest Ophthalmol Vis Sci. 2014;55:4832–41.
Shen LL, Sun M, Khetpal S, Grossetta Nardini HK, Del Priore LV. Topographic variation of the growth rate of geographic atrophy in nonexudative age-related macular degeneration: a systematic review and meta-analysis. Invest Ophthalmol Vis Sci. 2020;61:2.
Schmitz-Valckenberg S, Sahel JA, Danis R, Fleckenstein M, Jaffe GJ, Wolf S, et al. Natural history of geographic atrophy progression secondary to age-related macular degeneration (Geographic Atrophy Progression Study). Ophthalmology. 2016;123:361–8.
Lindner M, Böker A, Mauschitz MM, Göbel AP, Fimmers R, Brinkmann CK, et al. Directional kinetics of geographic atrophy progression in age-related macular degeneration with foveal sparing. Ophthalmology. 2015;122:1356–65.
Lindner M, Kosanetzky S, Pfau M, Nadal J, Gördt LA, Schmitz-Valckenberg S, et al. Local Progression Kinetics of Geographic Atrophy in Age-Related Macular Degeneration Are Associated With Atrophy Border Morphology. Invest Ophthalmol Vis Sci. 2018;59:Amd12-18.
Uji A, Nittala MG, Hariri A, Velaga SB, Sadda SR. Directional kinetics analysis of the progression of geographic atrophy. Graefes Arch Clin Exp Ophthalmol. 2019;257:1679–85.
Marsiglia M, Boddu S, Bearelly S, Xu L, Breaux BE JR, Freund KB, et al. Association between geographic atrophy progression and reticular pseudodrusen in eyes with dry age-related macular degeneration. Invest Ophthalmol Vis Sci. 2013;54:7362–9.
Grewal MK, Chandra S, Gurudas S, Rasheed R, Sen P, Menon D, et al. Functional clinical endpoints and their correlations in eyes with AMD with and without subretinal drusenoid deposits-a pilot study. Eye (Lond), 2022;36:398–406.
Tan R, Guymer RH, Luu CD. Subretinal drusenoid deposits and the loss of rod function in intermediate age-related macular degeneration. Invest Ophthalmol Vis Sci. 2018;59:4154–61.
Spaide RF, Yannuzzi L, Freund KB, Mullins R, Stone E. Eyes with subretinal drusenoid deposits and no drusen: progression of macular findings. Retina. 2019;39:12–26.
Shen LL, Liu F, Grossetta Nardini HK, Del Priore LV. Fellow eye status is a biomarker for the progression rate of geographic atrophy: a systematic review and meta-analysis. Ophthalmol Retin. 2019;3:305–15.
Wykoff CC, Rosenfeld PJ, Waheed NK, Singh RP, Ronca N, Slakter JS, et al. Characterizing new-onset exudation in the randomized phase 2 FILLY trial of complement inhibitor pegcetacoplan for geographic atrophy. Ophthalmology. 2021;128:1325–36.
A Phase 3 Safety and Efficacy Study of Intravitreal Administration of Zimura (Complement C5 Inhibitor). 2022 10 January 2022; Available from: https://ClinicalTrials.gov/show/NCT04435366.
Grassmann F, Fleckenstein M, Chew EY, Strunz T, Schmitz-Valckenberg S, Göbel AP, et al. Clinical and genetic factors associated with progression of geographic atrophy lesions in age-related macular degeneration. PLoS ONE. 2015;10:e0126636.
Fleckenstein M, Schmitz-Valckenberg S, Adrion C, Visvalingam S, Göbel AP, Mössner A, et al. Progression of age-related geographic atrophy: role of the fellow eye. Invest Ophthalmol Vis Sci. 2011;52:6552–7.
Sunness JS, Rubin GS, Zuckerbrod A, Applegate CA. Foveal-sparing scotomas in advanced dry age-related macular degeneration. J Vis Impair Blind. 2008;102:600–10.
Sunness JS, Rubin GS, Broman A, Applegate CA, Bressler NM, Hawkins BS. Low luminance visual dysfunction as a predictor of subsequent visual acuity loss from geographic atrophy in age-related macular degeneration. Ophthalmology. 2008;115:1480–8.
Grewal MK, Chandra S, Gurudas S, Bird A, Jeffery G, Sivaprasad S, et al. Exploratory study on visual acuity and patient-perceived visual function in patients with subretinal drusenoid deposits. J Clin Med. 2020;9:2832.
Burguera-Giménez N, García-Lázaro S, España-Gregori E, Gallego-Pinazo R, Burguera-Giménez N, Rodríguez-Vallejo M, et al. Multimodal evaluation of visual function in geographic atrophy versus normal eyes. Clin Ophthalmol. 2020;14:1533–45.
Chaikitmongkol V, Tadarati M, Bressler NM. Recent approaches to evaluating and monitoring geographic atrophy. Curr Opin Ophthalmol. 2016;27:217–23.
Sunness JS, Applegate CA. Long-term follow-up of fixation patterns in eyes with central scotomas from geographic atrophy that is associated with age-related macular degeneration. Am J Ophthalmol. 2005;140:1085–93.
Lindblad AS, Clemons TE. Responsiveness of the National Eye Institute Visual Function Questionnaire to progression to advanced age-related macular degeneration, vision loss, and lens opacity: AREDS Report no. 14. Arch Ophthalmol. 2005;123:1207–14.
Lindner M, Pfau M, Czauderna J, Goerdt L, Schmitz-Valckenberg S, Holz FG, et al. Determinants of reading performance in eyes with foveal-sparing geographic atrophy. Ophthalmol Retin. 2019;3:201–10.
Künzel SH, Lindner M, Sassen J, Möller PT, Goerdt L, Schmid M, et al. Association of reading performance in geographic atrophy secondary to age-related macular degeneration with visual function and structural biomarkers. JAMA Ophthalmol. 2021;139:1191–9.
Treatment of Advanced Dry Age Related Macular Degeneration With AAVCAGsCD59. 2022 10 January 2022; Available from: https://ClinicalTrials.gov/show/NCT03144999.
Gaya da Costa M, Poppelaars F, van Kooten C, Mollnes TE, Tedesco F, Würzner R, et al. Age and sex-associated changes of complement activity and complement levels in a healthy caucasian population. Front Immunol. 2018;9:2664.
Seddon JM, Silver RE, Kwong M, Rosner B. Risk prediction for progression of macular degeneration: 10 common and rare genetic variants, demographic, environmental, and macular covariates. Invest Ophthalmol Vis Sci. 2015;56:2192–202.
Seddon JM, Cote J, Page WF, Aggen SH, Neale MC. The US twin study of age-related macular degeneration: relative roles of genetic and environmental influences. Arch Ophthalmol. 2005;123:321–7.
Fritsche LG, Fariss RN, Stambolian D, Abecasis GR, Curcio CA, Swaroop A. Age-related macular degeneration: genetics and biology coming together. Annu Rev Genomics Hum Genet. 2014;15:151–71.
Yehoshua Z, de Amorim Garcia Filho CA, Nunes RP, Gregori G, Penha FM, Moshfeghi AA, et al. Systemic complement inhibition with eculizumab for geographic atrophy in age-related macular degeneration: the COMPLETE study. Ophthalmology. 2014;121:693–701.
GOLDEN STUDY: A Study to Assess Safety and Efficacy of Multiple Doses of IONIS-FB-LRx in Participants With Geographic Atrophy Secondary to Age-Related Macular Degeneration (AMD). 2022 10 January 2022; Available from: https://ClinicalTrials.gov/show/NCT03815825.
P, Z., Complement C5 inhibition in AMD., in Angiogenesis, Exudation and Degeneration meeting. 2016: Miami, FL, USA.
Wykoff CC, Hershberger V, Eichenbaum D, Henry E, Younis HS, Chandra P, et al. Inhibition of complement C3 in geographic atrophy with NGM621: Phase 1 study results. Investigative Ophthalmol Vis Sci. 2021;62:1214.
Safety and Tolerability Study of RO7171009 in participants with geographic atrophy (GA) secondary to age-related macular degeneration (AMD). 2022 10 January 2022; Available from: https://ClinicalTrials.gov/show/NCT03295877.
Phase 3 Study of ALK-001 in Geographic Atrophy. 2022 10 January 2022]; Available from: https://ClinicalTrials.gov/show/NCT03845582.
Iveric Bio Receives FDA Agreement Under Special Protocol Assessment (SPA) for GATHER2 Phase 3 Clinical Trial of Zimura® in Geographic Atrophy Secondary to Age-Related Macular Degeneration. New York, USA.
Guymer RH, Wu Z, Hodgson L, Caruso E, Brassington KH, Tindill N, et al. Subthreshold nanosecond laser intervention in age-related macular degeneration: The LEAD Randomized Controlled Clinical Trial. Ophthalmology. 2019;126:829–38.
Guymer RH, Chen FK, Hodgson L, Caruso E, Harper CA, Wickremashinghe SS, et al. Subthreshold nanosecond laser in age-related macular degeneration: observational extension study of the LEAD Clinical Trial. Ophthalmol Retin. 2021;5:1196–203.
Anand-Apte B, Chao JR, Singh R, Stöhr H. Sorsby fundus dystrophy: Insights from the past and looking to the future. J Neurosci Res. 2019;97:88–97.
Chew EY. Age-related macular degeneration: nutrition, genes and deep learning-The LXXVI Edward Jackson Memorial Lecture. Am J Ophthalmol. 2020;217:335–47.
Peng Y, Keenan TD, Chen Q, Agrón E, Allot A, Wong WT, et al. Predicting risk of late age-related macular degeneration using deep learning. NPJ Digit Med. 2020;3:111.
Colijn JM, Meester-Smoor M, Verzijden T, de Breuk A, Silva R, Merle B, et al. Genetic risk, lifestyle, and age-related macular degeneration in Europe: The EYE-RISK Consortium. Ophthalmology. 2021;128:1039–49.
Funding
This study is supported by the NIHR Biomedical Research Centre at Moorfields Eye Hospital National Health Service (NHS) Foundation Trust and the University College London Institute of Ophthalmology. SC and SS are funded by the ORNATE-India research project grant (Ref: GCRF UKRI (MR/P207881/1).
Author information
Authors and Affiliations
Contributions
SS and VC- conceptualization; SC, JK and NK – methodology and literature review; SS and SC – writing (original draft preparation); SS and VC – writing (review and editing).
Corresponding author
Ethics declarations
Competing interests
VC: Employee of Janssen R&D LLC but this work is not part of Janssen employment, and not endorsed by Janssen. SS has received funding/fees from Bayer, Novartis, Allergan, Roche, Boehringer Ingelheim, Optos, Oxurion, Oculis, Biogen, Apellis and Heidelberg Engineering.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sivaprasad, S., Chandra, S., Kwon, J. et al. Perspectives from clinical trials: is geographic atrophy one disease?. Eye 37, 402–407 (2023). https://doi.org/10.1038/s41433-022-02115-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02115-1
This article is cited by
-
The influence of the topographic location of geographic atrophy on vision-related quality of life in nonexudative age-related macular degeneration
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)