Abstract
Background
To examine risk factors for development of glaucoma in a large cohort of subjects with uveitis and scleritis.
Methods
Retrospective review of subjects diagnosed with uveitis or scleritis between 2006 and 2019 at Auckland District Health Board. Subjects were excluded if they had glaucoma due to another cause. Main outcome measure was development of glaucoma. Data for local steroid use was not available.
Results
3462 eyes of 2414 subjects were included in the study. Mean follow-up was 5.7 years (total follow-up time 19,897 eye years). Median age was 44.3 years and 1189 (49.3%) were female. Glaucoma developed in 222 eyes (6.3%) during the follow-up. Five-year cumulative risk of glaucoma was 6.2% (CI 5.0–7.5%) for anterior uveitis, 5.4% (CI 3.2–9.0%) for intermediate uveitis, 1.6% (CI 0.4–6.7%) for posterior uveitis, 8.7% (CI 6.5–11.7%) for panuveitis, and 3.2% (CI 1.0–9.5%) for scleritis. Five-year cumulative risk of glaucoma was lowest in HLA-B27 uveitis at 0.9% (CI 0.4–2.1%) and highest in viral uveitis 15.1% (CI 10.1–22.3%), sarcoidosis 9.9% (CI 6.1–15.9%) and tuberculosis 9.7% (CI 5.4–17.0%). On multivariate analysis, risk factors for development of glaucoma were older age at presentation, higher presenting intraocular pressure, chronic inflammation, and cystoid macular oedema.
Conclusions
Glaucoma is a common complication of uveitis and scleritis and was more frequent in older subjects, high presenting IOP, chronic inflammation and those with cystoid macular oedema. Local steroid therapy contributes to this, but is not quantifiable in this study. Targeted screening is required to avoid irreversible progression of glaucomatous optic neuropathy.
Similar content being viewed by others
Introduction
Raised intraocular pressure (IOP) of ≥21 mmHg is reported to occur in 14.4% of non-infectious uveitis patients per year [1]. The cause of raised IOP in uveitis and scleritis is frequently multifactorial. The pathological mechanisms can be broadly divided into: open angle, iatrogenic and angle closure. In open angle mechanisms, there is initially trabecular meshwork (TM) obstruction by inflammatory protein, cells and debris. Chronic inflammation leads to TM scarring and fibrovascular membrane formation over the TM [2]. Iatrogenic glaucoma can occur in patients treated with corticosteroids as these result in morphological and biochemical changes at the TM resulting in decreased aqueous outflow. Elevation of IOP develops in approximately one third of patients [3] on corticosteroid eye drops. The third pathological mechanism, secondary angle closure, can be chronic from the development of inflammatory peripheral anterior synechiae, or acute as a result of 360 degree posterior synechiae and subsequent pupil block with iris bombé [4]. Infrequently inflammatory oedema can result in anterior rotation of the ciliary body and subsequent secondary angle closure [2].
Uveitic glaucoma (UG) is a sight threatening complication of ocular inflammation that occurs in approximately 10% of all uveitis patients [2, 5]. Conversion from ocular hypertension to glaucoma may be rapid in subjects with uveitis, with a recent study reporting a median time from diagnosis of ocular hypertension to glaucoma of 1.2 years [6]. Vision loss due to UG is reported to be as high as 12% of all causes of vision loss [7], second only to cataract [8], but if detected early the risk of vision loss is modifiable. In a study of 1799 eyes with uveitis, glaucoma caused moderate vision loss in 0.4% and severe vision loss in 0.4% of all uveitis patients [9].
This study’s primary aim is to establish the rate and characteristics of patients who develop UG in Auckland, New Zealand. Analysis of these characteristics will also allow identification of risk factors which can be used to target screening of uveitis patients for UG.
Methods
Subject selection
This study adhered to the Declaration of Helsinki and was approved and monitored by the institutional review board of the University of Auckland. Patients with UG were identified from a database of all patients with uveitis and scleritis seen in Uveitis Clinic at Auckland District Health Board from tertiary uveitis clinics (JS and RN) and from initial presentations to the Acute Clinic between 2008 and 2019 (Ethics approval A + 1339). Subjects were excluded if they had a diagnosis of non-uveitic glaucoma by a glaucoma subspecialist. These were most commonly pre-existing diagnoses of glaucoma or other causes of secondary glaucoma clearly not related to ocular inflammation.
Data collection
Demographic data such as age at onset of inflammation, ethnicity and sex were gathered for all patients. Location of uveitis and disease pattern were classified as per the SUN guidelines. Thus, chronic anterior uveitis (CAU) was defined as persistent anterior uveitis characterised by prompt relapse (in <3 months) after discontinuation of therapy [10]. Best corrected visual acuity (VA) and IOP data at the onset of inflammation was collected as well as uveitis diagnosis. Snellen best corrected visual acuity (BCVA) was converted to logarithm of the minimum angle of resolution (LogMAR) for the purposes of analysis. For BCVA of counting fingers or worse, the following conversion was used: counting fingers, 2.0 LogMAR; hand movements, 2.3 LogMAR; light perception, 2.6 LogMAR; and no light perception, 2.9 LogMAR [11]. Time from onset of inflammation to diagnosis of glaucoma as well as total follow-up time was recorded. Glaucomatous optic neuropathy was diagnosed by a glaucoma subspecialist. This was exclusively in the setting of current or historic elevated IOP (≥24 mmHg) with optic nerve and/or visual field changes consistent with glaucoma. As per the UKGTS, a glaucomatous VF defect was defined as a reproducible reduction of sensitivity compared to the normative database in reliable tests at either: two or more contiguous locations with P < 0.01 loss or more, three or more contiguous locations with P < 0.05 loss or more, or a 10-dB difference across the nasal horizontal midline at two or more adjacent locations in the total deviation plot. A reliable VF was defined as having fewer than 15% false positive responses and fewer than 20% fixation losses [12]. Optic nerve head changes were evaluated using a combination of direct observation, stereo disc photography and Optical Coherence Tomography (OCT) of the retinal nerve fibre layer (RNFL) and ganglion cell complex. These were interpreted with caution as active inflammation is known to confound RNFL measurements [13]. Documented optic nerve damage over time or optic nerve changes on presentation that were corroborated by visual fields or clinical course confirmed the diagnosis of UG.
Patients were not included if they had ocular hypertension (≥24 mmHg) but no evidence of glaucomatous optic neuropathy. Damage to the optic nerve head was defined as a cup-to-disc ratio of ≥0.7, focal narrowing of the neural rim, or both as per the UKGTS [12].
Due to the tertiary nature of the uveitis clinic, data regarding local and topical steroid was incomplete and hence omitted.
Statistical analysis
Data was entered into an Excel spreadsheet and analysed in STATA version 15 (StataCorp 2017, College Station, TX). Categorical variables are presented as n (%) and continuous variables are presented as median (interquartile range [IQR]) or mean ± standard deviation, as appropriate. Five-year rates of glaucoma are reported with 95% confidence intervals (CI). Multivariate analysis of risk factors for glaucoma were calculated using a marginal Cox regression model with a robust sandwich estimate to allow for correlations between eyes. A p value of <0.05 was considered significant.
Results
Thirty-nine eyes were excluded due to glaucoma not related to ocular inflammation. This included 26 eyes with primary open angle glaucoma, 5 eyes with normal tension glaucoma, 3 eyes with pseudoexfoliative glaucoma, 2 eyes with pigment dispersion glaucoma, and 3 eyes with primary angle closure glaucoma.
3462 eyes of 2414 subjects were included for analysis. Mean follow-up was 5.7 years (median 3.6 years). Total follow-up time was 19,897 eye years. Five-year follow-up was available for 1398 eyes (39.9%) and 10-year follow-up was available for 615 eyes (17.6%). Subject demographics are reported in Table 1. Aetiology of uveitis is reported in Table 2. Uveitis was infectious in 710 (20.5%) and non-infectious in 2752 (79.5%).
During the follow-up 222 eyes (6.3%) developed glaucoma. Only 16 eyes (0.5%) had UG at presentation, the rest developed during the follow-up period. Five-year cumulative risk of glaucoma was 6.1% (CI 5.2–7.2%) and 10-year cumulative risk was 10.1% (CI 8.6–11.8%). Five-year cumulative risk of glaucoma for the most frequent diagnoses (n > 50) is reported in Table 3. Syphilis was not included in this table as the follow-up was relatively short compared to the other conditions and so 5-year risk was unable to be calculated. Comparing anatomical location of uveitis, 5-year cumulative risk of glaucoma was 6.2% (CI 5.0–7.5%) for anterior uveitis, 5.4% (CI 3.2–9.0%) for intermediate uveitis, 1.6% (CI 0.4–6.7%) for posterior uveitis, 8.7% (CI 6.5–11.7%) for panuveitis, and 3.2% (1.0–9.5%) for scleritis.
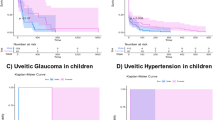
Risk factors for development of glaucoma are reported in Table 4. On univariate analysis, age, chronic inflammation, infectious aetiology, cystoid macular oedema and presenting IOP were all associated with an increased risk of developing glaucoma. On multivariate analysis, only age, chronic inflammation, presenting IOP, and cystoid macular oedema were associated with higher risk of glaucoma. Cumulative risk of glaucoma in chronic compared to acute recurrent disease is reported in Fig. 1. The cumulative risk of developing UG in subjects with chronic inflammation was 5.0% (95% CI 3.9–6.5%) at 1 year, 12.6% (95% CI 10.6–15.0%) at 5 years and 19.2% (95% CI 16.0–23.0%) at 10 years. In subjects with acute recurrent inflammation the cumulative risk of developing UG was 0.5% (95% CI 0.3–1.0%) at 1 year, 2.0% (95% CI 1.4–3.0%) at 5 years, and 4.6% (95% CI 3.3–6.5%) at 10 years.
Discussion
In our cohort, 6.3% of all uveitis patients developed UG over a mean follow-up period of 5.7 years. This is comparable to similar international studies in which the rate of UG in uveitis patients ranges between 6.8 and 9.6% [14,15,16,17]. For chronic uveitis, the cumulative hazard of UG (5.0% at 1 year, 12.6% at 5 years and 19.2% at 10 years) closely matched that of Neri et al. (6.6% at 1 year, 11.2% at 4 years and 22.7% at 10 years). However, for acute and recurrent uveitis our cumulative hazard of UG (0.5% at 1 year) was lower than that of Neri et al. (7.6% at 1 year). This may be due to differing aetiologies of acute uveitis patients as Neri et al. had a high rate of idiopathic uveitis (32/54, 59%) and a low rate of HLA-B27 uveitis (1/54, 1.9%) compared with our population [5].
Our analysis suggests that viral uveitis (HSV, HZV and CMV uveitis) had the highest cumulative 5-year risk of UG (15.1%) when compared to other causes. Herpes simplex virus (HSV) keratouveitis is well recognised as causing TM inflammation and a subsequent IOP rise. Merayo-Lloves et al. had a similar finding in their cohort; 23% of subjects with herpetic keratouveitis also had UG and it was the diagnosis with the highest proportion of UG in all diagnoses including over ten patients [17]. The proportion of herpetic keratouveitis patients that develop UG varies greatly in the literature between 10 and 28% [17, 18].
Chronic granulomatous uveitis had the second highest risk of UG; sarcoid uveitis 9.9% and tuberculosis (TB) 9.7% at 5 years. In fact, overall, chronic inflammation was the strongest risk factor associated with the development of UG in both univariate (HR 4.5) and multivariate (HR 3.2) regression analyses. Not only can chronic inflammation lead to structural damage resulting in raised IOP, but the increased need for chronic steroid treatment also plays a role in development of UG. Several studies have noted significantly higher rate of OHT in chronic uveitis compared with acute uveitis [16, 19].
Interestingly, idiopathic uveitis was also associated with a relatively high (5.8%) 5-year risk of UG. Given the diagnostic difficulty in diagnosing chronic granulomatous uveitis entities such as TB and sarcoid uveitis, we speculate that this may be due to a population of undiagnosed granulomatous uveitis within our ‘idiopathic’ group. HLA-B27 associated uveitis had a low 5-year risk of UG (0.9%) which is corroborated by Daniel et al. who found a low risk of OHT in HLA-B27 positive patients also [1].
Age (HR 1.02, p < 0.001) and presenting IOP (HR 1.06, p < 0.001) were associated with statistically significant but modest increased risks of developing UG in both univariate and multivariate regression analyses. With advancing age, the TM undergoes a decrease in cellularity and an increase in trabecular beam thickness and these are hypothesised to reduce aqueous outflow [20, 21]. Age has been significantly correlated with developing OHT in a population of uveitis patients in a previous study [16].
To our knowledge, our study was the first to show an association with CMO and UG [15, 16]. CMO is frequently an indicator of more severe inflammation, which may predispose subjects to UG. In addition, the treatment for CMO will often involve local steroid therapy, which may also increase the risk of developing UG. A more specific study looking at timing, dose and administration route of local steroid amongst a subset of these patients may be useful in clarifying the mechanism of this association.
A recent study by Liu et al. also suggests that glaucoma in the setting of uveitis has a higher rate of progression compared to glaucoma alone [22]. Visual field progression rates in subjects classified as having both uveitis and primary open angle glaucoma (−0.49 dB/year) were significantly higher than those with primary open angle glaucoma alone (−0.37 dB/year, p < 0.01). Subjects with uveitis were also more likely to be “rapid progressors” and on average had a worse baseline visual field mean deviation.
This study was limited by the retrospective analysis, and the absence of information on local steroid treatment and steroid-associated IOP elevation. The strengths of the study are that the subjects were drawn from both tertiary uveitis clinics and acute presentations, making the findings more generalisable, and the large population with a long follow-up period.
UG is a common complication of uveitis and scleritis, occurring in 6.3% of our patients over a median follow-up period of 43 months. In a multivariate analysis the following risk factors were identified for development of UG: age, high presenting IOP, chronic inflammation and cystoid macular oedema. With these factors in mind, we can target screening for uveitis patients to establish a diagnosis of UG early. All subjects with uveitis should receive a baseline IOP measurement and documentation of optic nerve appearance (preferably with optic nerve imaging including OCT in higher risk subjects). IOP should be monitored closely in subjects with acute inflammation or on steroid treatment and for those with stable disease we recommend that a yearly glaucoma check should be performed including IOP, gonioscopy and documentation of the optic nerve to enable early detection of glaucoma and more aggressive management.
Summary
What was known before
-
Glaucoma is an important cause of vision loss in subjects with glaucoma.
What this study adds
-
This study examines specific risk factors for development of glaucoma in subjects with uveitis and calculates the 5-year rate of glaucoma for different uveitis entities.
-
Glaucoma was more frequent in older subjects, those with high presenting IOP, chronic inflammation and those with cystoid macular oedema.
References
Daniel E, Pistilli M, Kothari S, Khachatryan N, Kaçmaz RO, Gangaputra SS, et al. Risk of ocular hypertension in adults with noninfectious uveitis. Ophthalmology. 2017;124:1196–208.
Siddique SS, Suelves AM, Baheti U, Foster CS. Glaucoma and uveitis. Surv Ophthalmol. 2013;58:1–10.
Becker B. Intraocular pressure response to topical corticosteroids. Investig Ophthalmol Vis Sci 1965;4:198–205.
Betts TD, Sims JL, Bennett SL, Niederer RL. Outcome of peripheral iridotomy in subjects with uveitis. Br J Ophthalmol. 2020;104:8–10.
Neri P, Azuara-Blanco A, Forrester JV. Incidence of glaucoma in patients with uveitis. J Glaucoma. 2004;13:461–5.
Ma T, Sims J, Bennett S, Chew S, Niederer RL. High rate of conversion from ocular hypertension to glaucoma in subjects with uveitis. Br J Ophthalmol. 2021;1–4.
Al-Ani HH, Sims JL, Tomkins-Netzer O, Lightman S, Niederer RL. Vision loss in anterior uveitis. Br J Ophthalmol. 2020;104:1652–7.
Yeo TK, Ho S, Lim W, Teoh S. Causes of visual loss associated with uveitis in a singapore tertiary eye center. Ocul Immunol Inflamm. 2013;21:1652–7.
Tomkins-Netzer O, Talat L, Bar A, Lula A, Taylor SRJ, Joshi L, et al. Long-term clinical outcome and causes of vision loss in patients with uveitis. Ophthalmology. 2014;121:2387–92.
Standardization of Uveitis Nomenclature for Reporting Clinical Data. Results of the first international workshop. Am J Ophthalmol. 2005;140:509–16.
Lange C, Feltgen N, Junker B, Schulze-Bonsel K, Bach M. Resolving the clinical acuity categories “hand motion” and “counting fingers” using the Freiburg Visual Acuity Test (FrACT). Graefes Arch Clin Exp Ophthalmol. 2009;247:137–42.
Garway-Heath DF, Crabb DP, Bunce C, Lascaratos G, Amalfitano F, Anand N, et al. Latanoprost for open-angle glaucoma (UKGTS): a randomised, multicentre, placebo-controlled trial. Lancet. 2015;385:1295–304.
Moore DB, Jaffe GJ, Asrani S. Retinal nerve fiber layer thickness measurements: uveitis, a major confounding factor. Ophthalmology. 2015;122:511–7.
Bodaghi B, Cassoux N, Wechsler B, Hannouche D, Fardeau C, Papo T, et al. Chronic severe uveitis: etiology and visual outcome in 927 patients from a single center. Medicine. 2001;80:263–70.
Heinz C, Koch JM, Zurek-Imhoff B, Heiligenhaus A. Prevalence of uveitic secondary glaucoma and success of nonsurgical treatment in adults and children in a tertiary referral center. Ocul Immunol Inflamm. 2009;17:243–8.
Herbert HM, Viswanathan A, Jackson H, Lightman SL. Risk factors for elevated intraocular pressure in uveitis. J Glaucoma. 2004;13:96–9.
Merayo-Lloves J, Power WJ, Rodriguez A, Pedroza-Seres M, Foster CS. Secondary glaucoma in patients with uveitis. Ophthalmologica. 1999;213:300–4.
Falcon MG, Williams HP. Herpes simplex kerato-uveitis and glaucoma. Trans Ophthalmol Soc UK. 1978;98:101–4.
Sharon Y, Friling R, Luski M, Campoverde BQ, Amer R, Kramer M. Uveitic glaucoma: long-term clinical outcome and risk factors for progression. Ocul Immunol Inflamm. 2017;25:740–7.
Alvarado J, Murphy C, Polansky J, Juster R. Age-related changes in trabecular meshwork cellularity. Investig Ophthalmol Vis Sci. 1981;21:714–27.
McMenamin PG, Lee WR, Aitken DAN. Age-related changes in the human outflow apparatus. Ophthalmology. 1986;93:194–209.
Liu X, Kelly SR, Montesano G, Bryan SR, Barry RJ, Keane PA, et al. Evaluating the impact of uveitis on visual field progression using large-scale real-world data. Am J Ophthalmol. 2019;207:144–50.
Author information
Authors and Affiliations
Contributions
RN was responsible for study design, data collection, statistical analysis, interpretation and paper writing and review. AW was responsible for analysis, paper writing and review. TM, SC and JS all contributed to collection and review of data and paper review.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Niederer, R.L., Wong, A.B.C., Ma, T. et al. Predictors of glaucoma in patients with uveitis and scleritis. Eye 37, 1254–1257 (2023). https://doi.org/10.1038/s41433-022-02101-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02101-7