Abstract
Objectives
The choice of suture is an important consideration in entropion repair, with implications on wound strength, inflammation and scar formation. There is no consensus on the best suture material or gauge of suture at present. We aim to assess the long-term outcome of entropion repair using 8-0 polyglactin sutures, with specific focus on rates of recurrence, wound dehiscence, infection and scarring.
Methods
This retrospective case series included consecutive patients from two institutions (84 eyes) undergoing entropion repair using a subciliary incision and a lateral wedge resection. Patients were invited for follow up review and patient records were evaluated to assess for cosmetic and functional outcome, complications and patient satisfaction.
Results
The median follow-up time from surgery was 48 months (range 20–100). There were five cases of entropion recurrence (5.9%), taking place between 8 months to 4 years after surgery, two cases required further surgery, while three were conservatively treated. There was no wound dehiscence. Two cases (2.4%) of mild superficial wound infections occurred which were successfully treated with topical antibiotics, 1 case (1.2%) of mild lid notching, and 1 case (1.2%) of scarring were recorded. 97% of patients reported to be satisfied with the outcome of their surgery.
Conclusions
The use of 8-0 polyglactin suture in entropion repair has resulted in good aesthetic and functional outcome in this case series, with low rates of recurrence, complications, and no case of wound dehiscence, suggesting this suture provides sufficient tensile strength to enable wound closure and healing.
Similar content being viewed by others
Introduction
Lower eyelid entropion affects 2% of people over the age of 60 years old and is associated with significant ocular morbidity [1]. Most cases are involutional; the primary causal factors are horizontal eyelid laxity, lower lid retractor dehiscence and pretarsal overriding of the pre-septal orbicularis oculi [2,3,4].
Surgical repair is almost always indicated to prevent keratopathy, provide symptomatic relief and improve quality of life [5]. A wide range of different techniques for entropion repair is reported in the literature [6,7,8,9,10]. In practice, vertical laxity is usually addressed with Jones retractor plication, a Wies procedure or Quickert everting sutures. In most cases however, concurrently addressing horizontal laxity is associated with better success rates [11, 12]. This horizontal component is typically addressed using either a lateral tarsal strip (LTS) procedure or full-thickness eyelid wedge resection.
In our experience, the commonest cause of involutional entropion is generalised horizontal lid laxity as opposed to true lateral canthal tendon (LCT) laxity or dystopia. For many surgeons, the LTS has become the preferred procedure for addressing both LCT laxity and generalised horizontal eyelid laxity [12, 13]. In part, this may be due to the risk of an eyelid margin ‘notch’ after wedge resection and repair. While eyelid wedge repair is most commonly performed using 6-0 absorbable sutures, smaller gauge suture needles may facilitate more meticulous wedge repair with more precise suture placement and less tissue resistance. Smaller gauge suture material would also be expected to result in reduced focal inflammation [13]. Despite these likely benefits, it is unknown whether smaller gauge sutures are associated with an unacceptable risk of wound dehiscence, or entropion recurrence.
The aim of this study is to report on the outcomes of our modified approach to the correction of involutional entropion using 8-0 polyglactin 910 (Vicryl). This modified approach addresses retractor dehiscence by direct repair through a subciliary skin incision, as well as employing a lateral wedge resection and repair to address the horizontal component.
Surgical technique
All cases were performed under local anaesthesia without sedation with the following standard technique. Cases were performed using an operating microscope (HM), or 2.5× surgical loupes (BP).
Topical anaesthetic drops of tetracaine hydrochloride 0.5% were instilled in the lower conjunctival sac. Following povidone-iodine skin preparation, the lower eyelid is infiltrated with 1–2 ml of 2% lidocaine and 1:200,000 epinephrine anaesthetic solution via a transconjunctival approach. A 6-0 silk traction suture can be passed through the grey line to aid dissection. A subciliary skin incision is made 1–2 mm below the lash line extending from the crow’s feet at the lateral canthus along the length of the lower eyelid. A skin flap is dissected along the inferior edge of this incision, and the pre-septal orbicularis oculi fibres are divided to expose the underlying septum. Bipolar cautery is applied to the skin edges and orbicularis to achieve haemostasis. Next, a lateral wedge is resected using either a 30-degree blade or No. 15 Bard-Parker blade. The use of a knife to cut the eyelid as opposed to scissors is essential due to the crushing effect of scissors with a resultant distortion in anatomy and difficulty in aligning the tissues for repair. The first vertical incision is taken in a posterior-anterior direction through the full height of the tarsus 5–10 mm medial to the lateral canthus, while the eyelid is held securely away from the globe using micro St. Martin forceps. This will form the lateral edge of the wedge resection. The intended medial edge of the wedge resection is determined by using micro St. Martins forceps to pull the two bisected eyelid edges horizontally so that they overlap under the desired tension. The medial-most intersection point is marked by scoring the margin of the medial eyelid with the blade. Holding this medial (major) portion of the bisected eyelid securely and away from the globe using micro St. Martins forceps, a second vertical incision is made through the full height of the tarsus in a posterior-anterior direction at the marked point. The wedge resection is completed using Westcott scissors to make a horizontal cut through the posterior lamella and connecting the inferior ends of the previous vertical incisions. Bipolar cautery is applied to the cut edges to achieve good haemostasis. The tarsus is first repaired by placing three horizontal bites using 8-0 polyglactin 910 sutures on a half-circle spatulated needle (Vicryl™ S-22) through each edge of the bisected tarsus. Meticulous care is taken to approximate the edges of the tarsus. The sutures are placed and tied in turn from inferior to superior with a surgeon’s knot. It is important to place a suture through the cut ends of the orbicularis strap bridging the tarsal repair, just below the lid margin, tied with a surgeon’s knot. Two further sutures are placed through the orbicularis strap inferior to this cardinal suture. A grey line suture bridging the repair is placed and tied on the lid margin with a reef knot, with the ends cut short. The orbital septum is incised to reveal the lower eyelid fat pads and lower eyelid retractors. The retractors are mobilised by dissection. Two to three 8-0 polyglactin 910 (vicryl) sutures are each passed through the distal end of the retractors evenly spaced horizontally along the length of the eyelid. A bite of each suture is taken through the anterior surface of the tarsus at its inferior edge and tied with a surgeon’s knot. Each of these sutures should be evenly spaced across the lower eyelid but with particular attention to the medial portion to ensure good posterior positioning of the punctum. Typically, the medial-most suture is positioned just lateral to the punctum with the other two either side of the wedge repair. The subciliary skin incision is closed with interrupted 8-0 vicryl. Chloramphenicol 1% eye ointment is applied to the wound and the inferior fornix at the end of the procedure and three times daily for 2 weeks. The skin sutures and grey line suture can be removed 1–2 weeks post-operatively. Figure 1a–j demonstrates the steps undertaken during surgery, while Fig. 1k is the 2-week post-operative result of the same eye, showing minimal inflammation, and no evidence of notch formation.
a Pre-operative appearance of lower lid involutional entropion. b Identifying the lower lid retractors. c Wedge resection. d Beginning of wedge repair. e Progression of wedge repair. f Grey line suture. g Orbicularis strap. h Retractor repair. i Skin repair. j Completion of surgery. k Result at 2 weeks post-operative follow up. Minimal inflammation and no notching.
Study procedures
This study is a retrospective non-comparative case series. Patients were eligible for inclusion if they had undergone surgical correction for involutional entropion by one of two surgeons (HM and BP) using the described technique at one of two different centres prior to July 2019. All patients underwent routine post-operative follow-up at 1–2 weeks for removal of sutures, and any subsequent follow up as required. Eligible patients were then invited to participate in an additional review for this study between September 2020 and February 2021, thus ensuring a minimum of 12 months follow-up. Any post-operative recurrences, infections, wound dehiscence, eyelid notching or visible scarring were recorded according to a standardised assessment proforma. Regarding patient satisfaction with their surgery, patients were asked whether they were satisfied; neither satisfied nor dissatisfied; dissatisfied; unsure.
The study proposal and procedures were submitted to the research and development office at both sites, and permission was granted to conduct this study by both departments. Informed consent was obtained from all participants.
Results
In total 146 patients were identified as being eligible for study inclusion. Of these, 94 patients were operated at the Queen Alexandra Hospital, Portsmouth (by HM) and 52 patients were operated at the Royal Bournemouth Hospital (by BP). In total, 69 patients (39.5%) were lost to follow-up. Of these, 40 patients passed away before the study follow-up period, 25 patients were not contactable and 4 did not consent to participate (3 due to advanced dementia, and one due to traumatic brain injury). Of the 40 patients who passed away, available medical notes were reviewed, and the causes of death were due to other medical co-morbidities. None were related to, or attributed to their entropion repair surgery or any other eye condition, and no deaths occurred within 3 months after surgery.
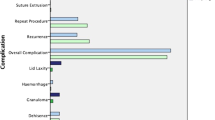
77 patients (84 eyes) were included in final analysis. Patient demographics are demonstrated in Table 1. Surgical outcomes are demonstrated in Table 2. One case was overcorrected due to excessive lid squeezing intraoperatively secondary to a dystonic disorder, which resulted in a difficult surgery. The ectropion was later corrected with one further surgery with good result, the patient is satisfied overall. Five cases of recurrence were recorded, occurring between 8 months to 4 years after the initial surgery. Risk of recurrence appears to increase steadily during this time with the risk of recurrence being 1.2% at 1 year post-operatively, 2.5% at 2 years and 4.4% at 3 years (Fig. 2). One case of recurrence was treated successfully with repeat surgery, one is planned for further surgery in the future, and the remaining three are mild and treated conservatively.
Two cases of mild superficial wound infections were observed, both were treated successfully with a short course of topical antibiotic with no further sequelae. A small notch was observed in one patient, and visible scarring observed in an additional one patient. Neither have required any surgical intervention. There were no cases of dehiscence or granuloma formation. Figure 2 demonstrates the cumulative risk of entropion recurrence post-surgery.
Discussion
The results of this study demonstrate that the exclusive use of 8-0 polyglycolic sutures in retractor plication via a subciliary approach combined with eyelid wedge resection achieved a high rate of surgical success, with few recurrences (5.9%). This supports the practice of using 8-0 absorbable suture for retractor repair, despite the faster absorption rate and reduced inflammatory reaction when compared with larger suture gauge.
The recurrence rate in this series is comparable to most longer-term studies on entropion repair reported in the medical literature. For example, Altieri et al. studied the 4-year outcome of entropion repair using Jones plication (using 5-0 Dexon sutures) compared with a modified plication method (with 6-0 Surgilene sutures), and the recurrence rate was 14.7% and 7.1% respectively, with all recurrences taking place over 3 years post-operatively [14]. Ranno et al. compared the recurrence rate after Jones plication alone (with 4-0 and 6-0 polyglactin sutures) versus Jones plication combined with a LTS (utilising 5-0, 6-0 and 7-0 polyglactin sutures), and their results show the rate of recurrence by 24 months was 16.5% and 3.5% respectively, with one case of suture granuloma which required re-exploration and re-suture [15]. Roberts et al. performed a combined full-thickness lid shortening with retractor plication on 42 eyes. The sutures used consisted of 5-0, 6-0 and 7-0 polyglactin, and after a mean follow up time of 14 months, 8% suffered a recurrence and granuloma was present in 5% [16].
Surgeons may be hesitant to use smaller gauge sutures due to concern over whether adequate tensile strength can be provided to maintain good wound closure, particularly in repairing eyelid wedge resection. 8-0 vicryl is comparatively weaker than 7-0 vicryl, and when kept in basic saline solution (to simulate the environment of human tissue), loses 11% of its tensile strength after 7 days [17]. Reassuringly however, in this series there were no cases of wound dehiscence. This supports the authors’ belief that 8-0 polyglactin suture provides sufficient tensile strength for eyelid wedge resection and repair, both in the immediate post-operative period and longer term.
In the authors’ view, the low rate of eyelid notching (1.2%), visible scarring and granuloma formation (1.2%) can be attributed to two factors that make smaller gauge 8-0 vicryl preferable to larger gauge alternatives: firstly, smaller gauge suture facilitates more refined and meticulous alignment of tissue (particularly the tarsal plate); secondly, smaller gauge suture is known to be associated with appreciably less granulomatous reaction. Cartmill et al. conducted an in-vivo eyelid study in 2004, comparing the tissue reaction caused by 5-0 and 7-0 vicryl. All 37 histological specimens analysed showed granuloma formation, and the size of the granuloma was positively correlated for the size of the suture, where the 5-0 suture elicited granulomas which were approximately twice the size of the 7-0 suture [18]. Suture induced granulomatous inflammation is likely initiated by adherence of metalloproteinases to the suture surface, which activates an inflammatory cascade leading to aggregation of histiocytes, foreign body giant cells, lymphocytes and eosinophils, resulting in the formation of a fibrous capsule around the infiltrate[19]. It has also been postulated that multifilament sutures evoke a stronger inflammatory response, as individual filaments will break off from the main body of the suture and cause a separate reaction [20]. These are important considerations, as more aggressive inflammation is associated with worsened scarring [21], reduced wound strength in the immediate post-operative period and increased risk of wound infection [22, 23].
While this study was not designed as a cost analysis, it should be considered that, as of December 2021, 8-0 polyglactin (W9560, double armed, Vicryl™, Ethicon) cost 126.95 GBP per box of 12 sutures, while 6-0 polyglactin (W9552, double armed, Vicryl™, Ethicon) cost 109.70 GBP per box. Related to cost (and operating time), another observation of note is that many (two-thirds) of the cases in this series were performed using an operating microscope, which is consistent with the individual surgeon’s preference (HM). The use of an operating microscope is not essential, and both the feasibility and cost implication of this will depend on local availability. Indeed, the remainder of cases in this series were performed using surgical loupes (BP). For many oculoplastic surgeons, an operating microscope will be readily accessible within their department and does offer improved surgical visualisation. Most surgeons will be familiar with the microscope’s use and while there is a learning curve associated with undertaking oculoplastic surgery under the microscope, with practice there is no appreciable delay in operating time.
Limitations of this study arise due to its retrospective nature. This has unfortunately resulted in many of patients being lost to study follow up, and concurrently there will be recall bias from the patients who were followed up during their reviews. A large proportion of patients who were lost to follow up (40 out of 69) unfortunately passed away prior to the follow up period of this study due to the study population’s age, medical co-morbidities and, in some cases, long follow-up period (up to 100 months). However, this retrospective design has allowed for a longer review period than is typically reported in many other prospective studies. In the initial days to months post-operatively, it is known that the polyglactin sutures will breakdown by hydrolysis and absorb [24, 25], and invariably some degree of inflammatory granulomatous reaction will occur. The critical point to consider at this stage, when assessing whether these reactions will ultimately result in negative surgical outcomes, is whether the patient will develop long term functional or aesthetic problems.
A further limitation is that cases in this study were performed by two consultant oculoplastic surgeons, and the results might not be directly comparable for more junior surgeons, e.g. trainees. It is acknowledged that the use of 8-0 sutures might have a steeper learning curve compared with wider gauge suture material. That said, both surgeons have found success in training juniors in employing the described technique. The authors also acknowledge that many surgeons will consider that entropion repair with 6-0 Vicryl often results in adequate outcomes. In our hands, it is our view that the use of 8-0 Vicryl is far superior to the outcomes we have observed with our own use of 6-0 Vicryl in the past. In particular, better surgical approximation of tissue planes can be achieved, with reduced scar formation, faster healing, and improved cosmesis. It is a limitation of this study that direct objective comparison cannot be made. That said, the baseline characteristics of the participants do appear to be comparable to other studies reported in the literature. While skin type was not formally recorded in this study it is certainly an important consideration as the propensity for scar formation can be affected by skin type and pigmentation. Both the study centres serve a predominantly Caucasian population, and whether these results translate into other skin types is not clear. Given the plethora of surgical techniques and preferred materials utilised for entropion repair, it would certainly be of great value to conduct a prospective, comparative study to further investigate this topic.
Conclusion
In striving for the optimal functional and aesthetic surgical result, suture material choice is an important consideration as the different materials, coating, and gauge of suture implanted will elicit a different reaction in human tissue. As yet, there is no consensus on the best suture type for entropion repair, the commonly used suture choices reported in the medical literature are vicryl, nylon and dexon sutures, with gauges typically between 5-0 and 7-0 [15, 16, 26,27,28]. This study demonstrates the safety of using 8-0 vicryl for entropion repair with wedge resection and retractor plication; There were no occurrences of wound dehiscence observed, and the rates of entropion recurrence and post-operative infection are favourable when compared with the existing literature. Indeed, the low rate of eyelid notching and scarring observed here highlights the potential advantages of using 8-0 absorbable suture compared with larger gauge alternatives.
Summary
What was known before
-
The choice of appropriate suture material and gauge is important in achieving good functional and aesthetic outcome from entropion repair surgery.
-
Large gauge sutures are associated with higher inflammatory response.
What this study adds
-
The use of 8-0 vicryl in involutional entropion repair resulted in minimal scarring or notching.
-
Good wound strength was achieved with this smaller gauge suture.
References
Damasceno R, Osaki M, Dantas P, Belfort R. Involutional Entropion and Ectropion of the Lower Eyelid: Prevalence and Associated Risk Factors in the Elderly Population. Ophthalmic Plast Reconstructive Surg. 2011;27:317–20.
Marcet M, Phelps P, Lai J. Involutional entropion. Curr Opin Ophthalmol. 2015;26:416–21.
Schulz CB, Fallico M, Rothwell A, Siah WF. Lower eyelid involutional entropion following cataract surgery. Eye (2021). https://doi.org/10.1038/s41433-021-01466-5.
Benger R, Musch D. A Comparative Study of Eyelid Parameters in Involutional Entropion. Ophthalmic Plast Reconstructive Surg. 1989;5:281–7.
Smith H, Jyothi S, Mahroo O, Shams P, Sira M, Dey S, et al. Patient-reported benefit from oculoplastic surgery. Eye. 2012;26:1418–23.
Collin J, Rathbun J. Involutional Entropion: a review with evaluation of a procedure. Arch Ophthalmol. 1978;96:1058.
Altieri M, Iester M, Harman F, Bertagno R, Capris P, Venzano D, et al. Comparison of Three Techniques for Repair of Involutional Lower Lid Entropion: a three-year follow-up study. Ophthalmologica. 2003;217:265–72.
Ho S, Pherwani A, Elsherbiny S, Reuser T. Lateral Tarsal Strip and Quickert Sutures for Lower Eyelid Entropion. Ophthalmic Plast Reconstruct Surg. 2005;21:345–8.
Jang S, Choi S, Jang J, Kim S, Choi H. Long-term surgical outcomes of Quickert sutures for involutional lower eyelid entropion. J Cranio-Maxillofac Surg. 2014;42:1629–31.
Lee H, Takahashi Y, Ichinose A, Kakizaki H. Comparison of surgical outcomes between simple posterior layer advancement of lower eyelid retractors and combination with a lateral tarsal strip procedure for involutional entropion in a Japanese population. Br J Ophthalmol. 2014;98:1579–82.
Danks J, Rose G. Involutional lower lid entropion. Ophthalmology. 1998;105:2065–7.
Scheepers M, Singh R, Ng J, Zuercher D, Gibson A, Bunce C, et al. A Randomized Controlled Trial Comparing Everting Sutures with Everting Sutures and a Lateral Tarsal Strip for Involutional Entropion. Ophthalmology. 2010;117:352–5.
Denniston A, Murray P. Oxford handbook of ophthalmology. 4th ed. Oxford: Oxford University Press; 2018. p. 166–7.
Altieri M, Kingston A, Bertagno R, Altieri G. Modified retractor plication technique in lower lid entropion repair: a 4-Year follow-up study. Can J Ophthalmol. 2004;39:650–5.
Ranno S, Sacchi M, Gilardi D, Lembo A, Nucci P. Retractor Plication versus Retractor Plication and Lateral Tarsal Strip for Eyelid Entropion Correction. Eur J Ophthalmol. 2014;24:141–6.
Roberts M, Baddeley P, Sinclair N, Lane C. The Lower Lid Diamond. Ophthalmic Plast Reconstruct Surg. 2012;28:44–6.
Brauner S, Berry J, Pye J, Lee E, Rhee D. Effect of Saline Conditions on the Tensile Strength of Ophthalmic Sutures. Ophthalmic Surg, Lasers Imaging Retin. 2011;42:148–51.
Cartmill B, Parham D, Strike P, Griffiths L, Parkin B. How Do Absorbable Sutures Absorb? A Prospective Double-Blind Randomized Clinical Study of Tissue Reaction to Polyglactin 910 Sutures in Human Skin. Orbit. 2014;33:437–43.
Setzen G, Williams E. Tissue Response to Suture Materials Implanted Subcutaneously in a Rabbit Model. Plast Reconstructive Surg. 1997;100:1788–95.
Postlethwait R. Long-Term Comparative Study of Nonabsorbable Sutures. Ann Surg. 1970;171:892–8.
DeLee J, Smith M, Green D. The reaction of nerve tissue to various suture materials: a study in rabbits. J Hand Surg. 1977;2:38–43.
Everett W. Sutures, incisions, and anastomoses. Ann R Coll Surg Engl. 1974;55:31–8.
Edlich R, Panek P, Rodeheaver G, Kurtz L, Edgerton M. Surgical sutures and infection: a biomaterial evaluation. J Biomed Mater Res. 1974;8:115–26.
J408G | Ethicon [Internet]. Ethicon.com. 2021 [cited 26 August 2021]. https://www.ethicon.com/na/epc/code/j408g?lang=en-default.
Weitzul S, Taylor RS. Suturing Technique and Other Closure Materials. In Surgery of the Skin. Elsevier Inc. 2005. p. 225–244. https://doi.org/10.1016/B978-0-323-02752-6.50021-3.
Boboridis K, Bunce C, Rose G. A comparative study of two procedures for repair of involutional lower lid entropion. Ophthalmology 2000;107:959–61.
Hedin A. Senile entropion - cure rate by retractor tightening and horizontal shortening. Acta Ophthalmologica Scandinavica. 2009;75:443–6.
Leibovitch I. Lateral Wedge Resection: A Simple Technique for Repairing Involutional Lower Eyelid Entropion. Dermatologic Surg. 2010;36:1412–8.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s concept and design, the collection and interpretation of data and preparation of the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, Y., Chihaia, M., Schulz, C.B. et al. 8-0 polyglactin 910 suture in entropion repair: long term follow up and rates of recurrence. Eye 37, 618–623 (2023). https://doi.org/10.1038/s41433-022-01997-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-01997-5