Abstract
Objectives
To evaluate the effect of the COVID-19 pandemic restrictions on myopia progression (MP) in school age children.
Methods
A total of 115 children aged 8–17 years with a diagnosis of myopia who had been followed-up for at least three years, were included in this study with a retrospective and single-centre design. The subjects’ age, the history of myopia in the family, the time spent in front of a screen, the digital devices used during home education (computer, tablet, smartphone, television), the time spent in open air (hours/day), the refractive error (RE) (spherical equivalent value) detected before the home education period and the changes in the myopia over the years, were recorded.
Results
The mean age was 12.06 (±2.29) years. Only the right eyes were included. The glasses use duration was 3.57 (±0.74) years. The annual MP amount 0.49 (±0.26), 0.41 (±0.36) and 0.54 (±0.43) dioptres (D) for the 2017, 2018 and 2019 years before home education, respectively, (p > 0.05), and 0.71 (±0.46) D in 2020, during home education. The increase in MP amount in 2020 compared to the 2019 and 2018 years was statistically significant (p < 0.003). MP was statistically significantly less in children who participated in open-air activities for 2 h a day and those who lived in detached houses (p = 0.004, p = 0.006, respectively).
Conclusion
During home confinement, education programmes of school children should be designed while taking into account preventive measures for MP, in particular for allowing children to spend at least 2 h of outdoor time per day.
Similar content being viewed by others
Introduction
Myopia is an important health problem worldwide. The World Health Organisation (WHO) estimates that half of the world’s population will be myopic by 2050 [1]. Other estimates are that 5 billion people will be diagnosed with myopia and over 1 billion with myopia above 5 dioptres (D) by 2050 [1, 2]. Some authors have described the increase in myopia in the last decade as an epidemic [3]. The insufficient time spent on outdoor activities is now being considered as an important risk factor for myopia development [4]. The duration and intensity of close distance activities is also associated with myopia [5]. High myopia (−6 D and above) is associated with problems that seriously impair vision, such as retinal detachment, glaucoma, choroidal neovascularization and posterior staphyloma [6].
It has previously been suggested that the intensive use of digital and virtual learning using a screen, resulting from the closure of schools and the intensification of home quarantine during the COVID-19 pandemic, would increase the myopia rate [7]. This kind of myopia, which is also described ‘Quarantine myopia’, has increased during the COVID-19 pandemic [8]. According to the United Nations Educational, Scientific and Cultural Organisation, 1.1 billion children in over 140 countries have been exposed to digital devices due to pandemic restrictions and distance education during May 2020 [8, 9]. The schools were closed on March 2020 in Turkey and are still closed at the time this article was written (mid-January 2021) and home education continues.
After the WHO declared COVID-19 a pandemic in March 2020, face-to-face training was interrupted in Turkey, as in most countries, in order to restrict the spread of the virus. In addition to the negative physical and mental effects of school closures, the children were increasingly exposed to smartphones, tablets, computers and the television, during the home education process [10]. The increasing myopia within the last year has been described as ‘quarantine myopia’, however, the effect of the technological device used for this education on myopia progression has not yet been studied [11].
We aimed to evaluate the changes in the refractive error within the last year (during the home education period) in children diagnosed with myopia and the effect on this change of the technological devices they use to receive education, as well as the time they spent in daylight during the quarantine period.
Materials and methods
Children aged 8–17 years with a diagnosis of myopia who had presented to the Alanya Alaaddin Keykubat University’s Eye Clinic between August 2020 and December 2020, were included in this study, with a retrospective and single centre design. The spherical equivalent (SE) (the total of the spherical and cylindrical value, divided by 2) was calculated in all cases. Myopic progression in one year under 0.50 D was identified as mild, 0.50–1 D as moderate, and 1 D or more as severe [12].
The study inclusion criteria were the presence of 0.50 D or more of myopia, having been followed up at the same clinic for at least three years and the presence of cycloplegic refraction values in the refractive examinations. The study exclusion criteria were myopia under 0.5 D, presence of strabismus, amblyopia, retinal disease, a history of eye surgery, follow-up duration less than three years, the use of 0.01% atropine drops and the use of contact lenses.
Refractive data for 2016, 2017, 2018 and 2019 were extracted from medical records at the time of examination in 2020 and the SE values were noted. The age, gender, hand dominance (the hand used for writing), the subject’s mother’s educational level, the technological support device used for home education and the duration of its use, the presence and duration of outdoor activities and the type of house the patient lived in, were all queried by phone. The analysis of the data was conducted during the month of January 2021. The refractive measurements were performed with an Auto Kerato-refractometer (Nidek ARK1-S, Nidek, San Jose, CA, USA).
Patients and their families gave verbal informed consent in which ‘they accepted that their prescription data would be used for statistical purposes because of the pandemic, keeping their identity confidential’, following the precepts of the Helsinki Declaration. Ethics committee approval for this sectional study was obtained from the Alaaddin Keykubat University Faculty of Medicine’s Ethics Committee (Decision no: 2021/01-22).
Statistical analysis
The paired sample t test was used to compare the difference between the measurement values of the same individual from the different years. The Anova t test was used in order to show any difference between the behaviour of the group mean value when the normality and equal distribution assumptions were met, and the non-parametric methods of the Kruskal–Wallis H Test (group number >2) and Mann–Whitney U Test (group number = 2) were used when they were not. As the data did not have a normal distribution, the non-parametric Spearman’s Rank Correlation test was used in calculating the correlation of any two numerical variables. Statistical significance was determined as p = 0.05 for all cases. The IBM SPSS (Statistics Programme for Social Sciences for Windows, Version 21.0, Armonk, NY, IBM Corp.) software programme was used for the statistical analyses.
Results
Between August 2020 and December 2020, 135 patients met the study inclusion criteria. The family of 115 children could be reached and the study was completed with 115 participants. The mean age of the subjects was 12.06 ± 2.29 years and 75 (65.2%) were female. The glasses use duration was 3.57 ± 0.74 years.
A smartphone was the most common device used to attend the courses at 53%, the mean duration spent in front of the screen was 5.77 ± 1.34 h/day, and the educational level of the mother was primary school in 42.6%. The characteristics of the cases are presented in Table 1.
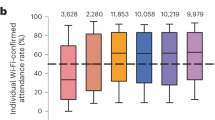
The mean SE of the refractive values was −1.14 ± 0.66 D in 2016, −1.47 ± 0.82 D in 2017, −0.45 ± 0.91 D in 2018, −1.99 ± 1.04 D in 2019 and −2.7 ± 1.21 D in 2020. Annual progression analysis revealed a myopic progression of 0.71 ± 0.46 D in 2020 and this value was significantly higher than in 2019 and 2018 (0.54 ± 0.43, p = 0.003; and 0.41 ± 0.36, p < 0.001, respectively) (Fig. 1). The comparison of the MP values based on the years is presented in Table 2.
Spending 2 h/day on outdoor activities and the type of housing were seen to have a statistically significant effect in the analysis of the factors influencing the MP in 2020 (Table 3). The mean myopic progression in the last year was 0.55 ± 0.42 D in children who spent time outside in the daylight for 2 h a day, and 0.82 ± 0.45 D in children who did not (p = 0.003, Mann–Whitney U Test). The mean myopic progression in the past year was similarly 0.5 ± 0.41 D in children living in detached houses and 0.79 ± 0.45 D in those living in apartments (p = 0.006, Mann–Whitney U Test).
The myopia progression in 2020 was slow (0.31 ± 0.2 D) in 49 subjects (42.6%), moderate (0.82 ± 0.14 D) in 45 (39.1%) and rapid (1.42 ± 0.29 D) in 21 of them (18.3%) (Table 4). No significant correlation was found between the 2020 progression and the daily digital display device use, age and glasses use duration (r = −0.094, p = 0.32; r = 0.018, p = 0.848; r = 0.033, p = 0.727, respectively).
The proportion of children taking breaks after screen usage or lesson every 30 min, was only 6 (5.2%) of all participants. Whether taking a break every 30 min or not did not have a statistically significant effect on the amount of myopic progression in 2020 (p = 0.708, Mann–Whitney U Test).
Discussion
The first case of COVID-19 in Turkey was announced in March 11 by the Turkish Ministry of Health, on the very same day the pandemic was declared by the WHO [13, 14]. The subjects of our study consisted of the cases that presented to our outpatient department between August and December 2020, taking into account that the schools were closed and home-education started in March 2020.
The negative effect of close work and the positive effect of daylight in keeping myopia progression under control have been demonstrated by other studies [15]. Children staying at home during the pandemic and attending online education has increased the concerns about myopia progression. The results of our study have revealed that progression in the last year, within the age range of 8–17 years, is significantly higher than in the previous years. In addition, spending 2 h daily in an outdoor activity and living in a detached house were both found to decrease myopic progression. However, the effect of the duration of digital device use and the type of device used (smartphone, tablet, television) on myopia progression, was not found to be statistically significant.
Wang et al. have recently reported a 1.4 to 3 times increase in the myopia prevalence in 2020 in children aged 6–8 years, compared to the previous five years, with the ‘photoscreening’ test in over one hundred thousand children [16]. We evaluated the follow-up examinations of children with a diagnosis of myopia instead of children newly diagnosed with myopia. Wang et al. did not use cycloplegia for the refraction evaluation in children [16]. The myopia results of photoscreening-based devices are known to be exaggerated and to be affected by the experience of the person performing the measuring [17, 18]. Although these devices are useful in preverbal and nonverbal children, the general ophthalmological approach in school-age children is to determine cycloplegic refraction values [19]. We only included the cases that had undergone cycloplegic evaluation in our study, in order to ensure healthy results.
The relationship of long-term exposure to digital device screens with myopia is still controversial and some studies support this relationship, while others claim the opposite [20, 21]. Interestingly, the duration of reading, watching television or playing games on the computer has been suggested to influence myopia’s progression, rather than its occurrence, in the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error Study [22]. However, this may not be due to the effect of digital screens on the progression alone and could also be influenced by the ‘substitution effect’, as in the indirect decrease of the outdoor activity related to the increased time spent in front of the screen [23]. The effect on myopia of the activities performed in front of the digital screen, may not be equivalent to the effect of reading and writing in traditional education [24, 25]. Dopamine release in the retina is stimulated by daylight and suppresses the axial expansion of the eye [26, 27]. In addition, studies have revealed that the dopaminergic system in the frontal lobe is activated by the use of a digital device [28]. The effect of display devices on the retinal dopamine levels is not known, however, Spiperone, a dopamine antagonist, has been shown to inhibit the protective effect of light against the increase of the ocular axial length in experimental models [29]. It has not been possible to demonstrate the relationship between myopia progression and the duration of use of a digital display device such as a tablet, smartphone, or computer with our study.
Outdoor activities have previously been shown to decrease the occurrence and progression of myopia [30, 31]. He et al. have reported that every additional 40 min of outside activities decreases myopia incidence by 23% [30]. Wu et al. have suggested that myopia progression in children who spent >11 h a week outdoors decreases by 53% [31]. In general, 2 h of outdoor activities per day is assumed to decrease myopia progression in school age children [7]. We similarly observed that myopia progression was 33% less in children with 2 h of outdoor activity daily, even though the duration spent in front of the screen was similar. Although outdoor activities had a protective effect on myopia progression in our study, we did not observe a similar protective effect on the myopia progression rate. This result indicates that myopia progression occurs as a result of multiple factors, including environmental ones.
The type of house the child lives in is one of these environmental factors and we found it to be an independent risk factor for myopia progression. Similarly, a relationship between the type of the house the subject lives in and myopia, was revealed in a study conducted in Australia [20]. Myopia was reported to be more common in children living in apartment buildings compared to those living in detached houses in the same study [20]. He et al. found a significant relationship between school location and myopia [32]. Wu et al. reported an increase in the myopia prevalence with increasing number of floors in the building [33]. We think that accepting myopia as a public health problem could be effective in the intensification of screening in pre-school and school-aged children, as well as in designing cities in the fight against myopia.
The limitations of this study include the lack of data on pre-school children, the potential bias resulting from the information about the time spent in front of the screen and outside activities being self-reported, by way of the telephone, the accuracy of which could not be verified. The lack of biometry or keratometry information and the inability to determine the cause-effect relationship, as a result of the study’s cross-sectional design, are also limitations. A German study comparing refractive error information obtained from the patient statements with the information obtained from the opticians, has shown the two to be very similar [34]. Our study is, however, and to the best of our knowledge, the first to evaluate the effect of home education during the COVID-19 pandemic in myopic children, using cycloplegic refraction results. It is also the first study to investigate the effect of the technological devices used for home education on myopia progression.
In conclusion, home education during the COVID-19 pandemic has increased the myopia progression rate in children, compared to the previous years. This increase has been found to be related to the duration of outdoor activities, as reported previously. A detached type of housing allows for a child to perform outside activities easily, while at home. During home confinement, education programmes of school children should be designed while taking into account preventive measures for MP, in particular for allowing children to spend at least 2 h of outdoor time per day.
Summary
What was known before
-
Myopia progression is considered to increase with close work and little exposure to daylight.
What this study adds
-
Spending 2 h daily in an outdoor activity and living in a detached house were both found to decrease myopic progression. The effect of the duration of digital device use and the type of device used (smartphone, tablet, television) on myopia progression, was not found to be statistically significant.
References
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–42.
Dolgin E. The myopia boom. Nature. 2015;519:276–8.
Morgan IG, French AN, Ashby RS, Guo X, Ding X, He M, et al. The epidemics of myopia: aetiology and prevention. Prog Retin Eye Res. 2018;62:134–49.
Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012;379:1739–48.
Saw SM, Chua WH, Hong CY. Nearwork in early-onset myopia. Invest Ophthalmol Vis Sci. 2002;43:332–39.
Fricke TR, Jong M, Naidoo KS, Sankaridurg P, Naduvilath TJ, Ho SM, et al. Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050: systematic review, meta-analysis and modelling. Br J Ophthalmol. 2018;102:855–62.
Wong CW, Tsai A, Jonas JB, Ohno-Matsui K, Chen J, Ang M, et al. Digital screen time during the COVID-19 pandemic: risk for a further myopia boom? Am J Ophthalmol. 2020;223:333–7.
Klaver CCW, Polling JR, Enthoven CA. 2020 as the year of quarantine myopia. JAMA Ophthalmol. 2021;139:300–1.
Global monitoring of school closures caused by COVID-19. https://en.unesco.org/covid19/educationresponse. Accessed 16 May 2020.
Sumitha M, Sanjay S, Kemmanu V, Bhanumathi MR, Shetty R. Will COVID-19 pandemic-associated lockdown increase myopia in Indian children? Indian J Ophthalmol. 2020;68:1496.
Pellegrini M, Bernabei F, Scorcia V, Giannaccare G. May home confinement during the COVID-19 outbreak worsen the global burden of myopia? Graefes Arch Clin Exp Ophthalmol. 2020;258:2069–70.
Hsu CC, Huang N, Lin PY, Fang SY, Tsai DC, Chen SY, et al. Risk factors for myopia progression in second-grade primary school children in Taipei: a population-based cohort study. Br J Ophthalmol. 2017;101:1611–7.
Republic of Turkey Ministry of Health, General Directorate of Public Health. COVID-19 (SARS-CoV2 Infection) Guide (Science Board Study): General information, epidemiology and diagnosis. Republic of Turkey Ministry of Health website. June 1, 2020. https://covid19bilgi.saglik.gov.tr. Accessed 4 June 2020.
Global surveillance for COVID-19 caused by human infection with COVID-19 virus: interim guidance. World Health Organization; March 20, 2020.
Jones-Jordan LA, Sinnott LT, Cotter SA, Kleinstein RN, Manny RE, Mutti DO, et al. CLEERE study group. Time outdoors, visual activity, and myopia progression in juvenile-onset myopes. Invest Ophthalmol Vis Sci. 2012;53:7169–75.
Wang J, Li Y, Musch DC, Wei N, Qi X, Ding G, et al. Progression of myopia in school-aged children after COVID-19 home confinement. JAMA Ophthalmol. 2021;139:293–300.
Chat SW, Edwards MH. Clinical evaluation of the Shin-Nippon SRW-5000 autorefractor in children. Ophthalmic Physiol Opt. 2001;21:87–100.
Peterseim MM, Papa CE, Wilson ME, Cheeseman EW, Wolf BJ, Davidson JD, et al. Photoscreeners in the pediatric eye office: compared testability and refractions on high-risk children. Am J Ophthalmol. 2014;158:932–8.
Hu YY, Wu JF, Lu TL, Wu H, Sun W, Wang XR, et al. Effect of cycloplegia on the refractive status of children: the Shandong children eye study. PLoS ONE. 2015;10:e0117482.
Ip JM, Saw SM, Rose KA, Morgan IG, Kifley A, Wang JJ, et al. Role of near work in myopia: findings in a sample of Australian school children. Invest Ophthalmol Vis Sci. 2008;49:2903–10.
Guan H, Yu NN, Wang H, Boswell M, Shi Y, Rozelle S, et al. Impact of various types of near work and time spent outdoors at different times of day on visual acuity and refractive error among Chinese school-going children. PLoS ONE. 2019;14:e0215827.
Jones-Jordan LA, Mitchell GL, Cotter SA, Kleinstein RN, Manny RE, Mutti DO, et al. CLEERE study group. Visual activity before and after the onset of juvenile myopia. Invest Ophthalmol Vis Sci. 2011;52:1841–50.
Ku PW, Steptoe A, Lai YJ, Hu HY, Chu D, Yen YF, et al. The associations between near visual activity and incident myopia in children: a Nationwide 4-year follow-up study. Ophthalmology. 2019;126:214–20.
Sah RP, Ramasubramanian V, Reed O, Meyer D, Bradley A, Kollbaum PS. Accommodative behavior, hyperopic defocus, and retinal image quality in children viewing electronic displays. Optom Vis Sci. 2020;97:628–40.
Lanca C, Saw SM. The association between digital screen time and myopia: a systematic review. Ophthalmic Physiol Opt. 2020;40:216–29.
McCarthy CS, Megaw P, Devadas M, Morgan IG. Dopaminergic agents affect the ability of brief periods of normal vision to prevent form-deprivation myopia. Exp Eye Res. 2007;84:100–7.
Feldkaemper M, Schaeffel F. An updated view on the role of dopamine in myopia. Exp Eye Res. 2013;114:106–19.
Dresp-Langley B. Children’s health in the digital age. Int J Environ Res Public Health. 2020;17:3240.
Smith EL 3rd, Hung LF, Huang J. Protective effects of high ambient lighting on the development of form-deprivation myopia in rhesus monkeys. Invest Ophthalmol Vis Sci. 2012;53:421–8.
He M, Xiang F, Zeng Y, Mai J, Chen Q, Zhang J, et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015;314:1142–8.
Wu PC, Chen CT, Lin KK, Sun CC, Kuo CN, Huang HM, et al. Myopia prevention and outdoor light intensity in a school-based cluster randomized trial. Ophthalmology. 2018;125:1239–50.
He M, Huang W, Zheng Y, Huang L, Ellwein LB. Refractive error and visual impairment in school children in rural southern China. Ophthalmology. 2007;114:374–82.
Wu X, Gao G, Jin J, Hua W, Tao L, Xu S, et al. Housing type and myopia: the mediating role of parental myopia. BMC Ophthalmol. 2016;16:151.
Jobke S, Kasten E, Vorwerk C. The prevalence rates of refractive errors among children, adolescents, and adults in Germany. Clin Ophthalmol. 2008;2:601–7.
Acknowledgements
We would like to thank Optician Özlem Aslan for her contribution to our study.
Author information
Authors and Affiliations
Contributions
FA was responsible for designing the study protocol, conducting the search, obtaining data, interpreting results, drafting and revising the article. FA, NSK obtained the data, conducted the analyses, contributed to the design of the study, interpreting results and revision of the article. All authors read and approved the final paper.
Corresponding authors
Ethics declarations
COMPETING INTERESTS
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aslan, F., Sahinoglu-Keskek, N. The effect of home education on myopia progression in children during the COVID-19 pandemic. Eye 36, 1427–1432 (2022). https://doi.org/10.1038/s41433-021-01655-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01655-2
This article is cited by
-
Attitudes and knowledge of myopia management by Spanish optometrists
International Ophthalmology (2023)
-
Effects of behaviors and surrounding environment on myopia before and during the COVID-19 pandemic: a longitudinal analysis of children and adolescents in China
Journal of Public Health (2023)
-
Comment on: The effect of home education on myopia progression in children during the COVID-19 pandemic
Eye (2022)