Abstract
Objective
This study was performed to evaluate the clinical effect of skin redraping on lower eyelid epiblepharon accompanied by a medial epicanthal fold.
Methods
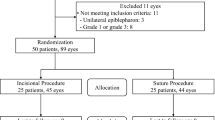
This retrospective case series involved 572 eyes of 286 patients who underwent skin redraping surgery to treat lower eyelid epiblepharon accompanied by a medial epicanthal fold from January 2015 to May 2019. The postoperative surgical results were classified as “good”, “fair” and “poor”. The incision scars were assessed using the Vancouver scar scale. The patients’ subjective satisfaction and incidence of complications were also documented.
Results
The mean patient age at the time of surgery was 6.9 ± 3.6 years (3–12 years), and the mean follow-up time was 32.6 ± 13.5 months (6–58 months). The clinical symptoms and severity of keratopathy were improved postoperatively. “Good” surgical outcomes were obtained in all patients, the mean Vancouver scar scale score was 1.1 ± 0.3, and hypertrophic scar formation did not occur. A total of 272 patients and their guardians were “very satisfied” with the cosmetic outcomes.
Conclusion
Skin redraping was effective and endurable in the treatment of lower eyelid epiblepharon accompanied by a medial epicanthal fold. The postoperative scars were slight and nearly invisible, and no cases of recurrence were observed in this study.
Similar content being viewed by others
Introduction
Epiblepharon refers to an abnormal state in which excessive skin and orbicularis oculi muscle tissues push the eyelid margin towards the eyeball, which causes the eyelashes to be tilted vertically toward the cornea and conjunctiva. In most patients, epiblepharon occurs bilaterally at the medial side of the lower eyelid. Typical clinical symptoms of epiblepharon are caused by corneal and conjunctival irritation (e.g., tears, photophobia, rubbing, blinking, and/or foreign body sensation). If clinical symptoms remain untreated for an extended duration, patients may develop keratitis and visual impairment.
Studies have shown that epiblepharon is present in 20% of Asian children at the age of 2 years, although its incidence decreases with age, 7% of Asian children exhibit epiblepharon at the age of 5–6 years [1]. The aetiology of lower eyelid epiblepharon includes movement in the horizontal direction, due to pressure from the medial epicanthal fold, and movement in the vertical direction, due to pressure from excessive skin and orbicularis muscle tissue [2]. The medial epicanthal fold (i.e., Mongolian fold) is a semilunar skin fold in the inner canthus that descends along the medial side from the upper eyelid to the lower eyelid. It is characterised by partial or complete occlusion of the inner canthus and lacrimal caruncle, and it may partially occlude the visual field. Many surgeons prefer simultaneous correction of epiblepharon and the medial epicanthal fold.
Several surgical procedures are available to correct epiblepharon, such as the everting suture technique [3], rotating suture technique [4], and Hotz procedure and its modified versions [5]. Generally, selection of the surgical treatment approach for epiblepharon depends on the severity of the epiblepharon and the surgeon’s preference [6]. The everting suture technique is used to treat mild to moderate epiblepharon, while incisional techniques (e.g., suture rotation technique and Hotz procedure) are used to treat severe epiblepharon. Notably, many difficulties limit the use of these techniques. The scar barrier created by the everting suture technique is not sufficiently secure to correct epiblepharon, and the reported recurrence rate is 24.3%; thus, use of this method has declined [7]. The rotating suture and Hotz techniques focus on resection of excessive skin and orbicularis oculi muscle, thereby ignoring correction of the medial epicanthal fold. Unfortunately, epiblepharon is often accompanied by a medial epicanthal fold in Asian patients [8]; disregarding this comorbid condition may lead to inadequate correction of epiblepharon and eventual recurrence. Therefore, the optimal surgical approach for treatment of lower eyelid epiblepharon (i.e., the approach that achieves a low recurrence rate) remains highly controversial. This retrospective study was conducted to evaluate the clinical results of a skin redraping method for treatment of lower eyelid epiblepharon combined with a medial epicanthal fold in Asian children.
Subjects and methods
This prospective study included 286 patients who underwent skin redraping from January 2015 to May 2019. Based on the patients’ recorded medical histories, all exhibited epiblepharon of the medial part of the lower eyelid combined with a medial epicanthal fold, along with clinical symptoms of ocular irritation (e.g., tears, photophobia, and rubbing). Preoperative cilia–cornea contact was observed by slit-lamp examination in all patients. The patients’ characteristics were recorded, including age, sex, degree of epiblepharon, symptoms, and follow-up duration. All procedures were performed by one experienced surgeon (N.S.) using a standard technique. The study protocol was approved by the Ethics Committee of Eye & ENT Hospital of Fudan University and adhered to the tenets of the Declaration of Helsinki. All patients provided informed consent prior to participation in our study. The exclusion criteria were previous eyebrow or eyelid surgery, congenital entropion, follow-up duration of <6 months, absence of ocular irritation, and distichiasis.
The following clinical characteristics were evaluated: preoperative and postoperative keratopathy related to epiblepharon; inner intercanthal distance; [9] lower eyelid morphology; and complications such as infection, ectropion, lacrimal drainage injury, and hypertrophic scar formation. Vancouver scar scale (VSS) scores were collected through clinical analysis by three independent doctors [10], to evaluate the incisional scars in the area of the lower eyelid and medial canthus [11].
The surgical outcome was classified as ‘good’, ‘fair’, or ‘poor’ [8]. A good outcome was defined as the absence of contact between the cilia and ocular surface. A fair outcome was defined as the presence of several points of contact between the cilia and ocular surface without clinical symptoms. A poor outcome was defined as the presence of multiple points of contact between the cilia and the ocular surface, with symptoms of ocular irritation. Patients with a good or fair outcome did not require further surgical intervention. The degree of subjective satisfaction with the cosmetic outcome was evaluated by the patients or their guardians and classified into four levels: ‘very satisfied’, ‘satisfied’, ‘neutral’, and ‘unsatisfied’. The VSS score and subjective satisfaction were analysed and collected when the patients and their guardians returned for their follow-up visit 6 months after the operation.
Surgical technique
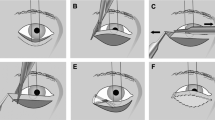
All surgical procedures (Fig. 1) were performed under general anaesthesia or local anaesthesia without sedation.
-
1.
The surgical design was established as follows. The surgeon pulled the skin of the inner canthus toward the nasal side to expose the angle of the covered inner canthus. The projection of the inner canthal fold surface at the innermost point of the inner canthus was established as the new inner canthus point ‘a’. From point ‘a’, a horizontal line was marked from the nasal side to the medial epicanthal fold edge of point ‘b’. Point ‘c’ was marked by traction of the medial epicanthal fold to the nasal side, which was 2 mm inside of the lacrimal caruncle. A line was formed to join points ‘b’ and ‘c’, and this line was then extended along the eyelash root to point ‘d’. Point ‘d’ was 2 mm beyond the edge of the trichiasis. The upper eyelid was opened along the double eyelid line (to a width of 4–5 mm if the patient did not exhibit a double eyelid); point ‘e’ represented the intersection of the curved double eyelid line and the epicanthal margin. A line was formed to join points ‘b’ and ‘e’ and marked alongside the curved edge of the epicanthal margin. The triangular area within lines ‘a–b–e’ was the estimated extent of skin resection (Fig. 1A, B).
-
2.
Local infiltration anaesthesia was performed with 2% lidocaine and 0.1% adrenaline (1:200,000). A skin incision was made along the marked line, and the skin of the triangular area within lines ‘a–b–e’ was resected.
-
3.
Abnormal adhesions between the skin and orbicularis oculi muscle were completely removed, which reduced the tension of the orbicularis oculi muscle on the skin and subcutaneous tissue. The adhesion between the medial canthal ligament and orbicularis oculi muscle was completely isolated, and the medial canthal ligament was then carefully separated and shortened by medial canthal ligament plication [12].
-
4.
Points ‘a’ and ‘c’ were connected with a 7-0 absorbable suture, and a tension-free flap was placed under the eyelashes for skin redraping. The skin beneath the trichiasis of the lower eyelid was removed (~0.5–1 mm), and the skin of the lower eyelid and corresponding points of the eyelid edge was intermittently sewn using a 7-0 absorbable suture without overcorrection of the lower eyelids. Additionally, the incision above the inner canthus was sewn using a 7-0 absorbable suture without tension, and well-formed along the curve of the upper eyelid crease.
A Surgical design. B Surgical design when the skin of inner canthus was pulled toward the nasal side. C Abnormal adhesion between skin and orbicularis oculi muscles was dissected. D Exposure of medial canthus ligament. E The tension-free flaps were prepared. F The tension-free flaps were sutured intermittently without overcorrection of the lower eyelids, the skin incision above the inner canthus was well-formed along with curve of the upper eyelid crease.
Results
This study involved 286 patients (161 boys, 125 girls), including 18 patients with mild epiblepharon, 93 patients with moderate epiblepharon, and 175 patients with severe epiblepharon. All patients exhibited clinical symptoms of ocular irritation, and most patients had one or more complaints. The mean patient age was 6.9 ± 3.6 years (range, 3–12 years), and the mean follow-up duration was 32.6 ± 13.5 months (range, 6–58 months).
General anaesthesia was used for patients younger than 10 years, while local anaesthesia without sedation was used for patients older than 10 years who were able to cooperate. The clinical symptoms and severity of keratopathy were improved postoperatively in all patients. During the postoperative follow-up visits, good outcomes were obtained in all patients; none had fair or poor outcomes. Hypertrophic scar formation was not present in any patients; the mean VSS score was 1.1 ± 0.3, which indicates that the scars of the lower eyelid and medial canthus were not obvious. The morphology of the lower eyelid was natural and symmetrical in all patients, and no patients exhibited lower eyelid creases or ectropion formation. After surgery, the inner intercanthal distance was reduced; furthermore, the lacrimal caruncle exhibited greater exposure, which resulted in cosmetic improvement of the eyes (Figs. 2 and 3). In terms of subjective satisfaction, 272 patients or their guardians were very satisfied with the cosmetic outcomes, while 14 patients or their guardians were satisfied with the degree of medial canthal scars; no patients or guardians reported neutral or unsatisfied results. Wound dehiscence was observed in the medial canthal area in one patient because of poor wound care by the guardians. However, the wound healing resumed after 3 days of careful dressing and care, and the medial canthal morphology was satisfactory for the patient’s guardians. There were no other complications, such as infection, incomplete eyelid closure, or canalicular injury. No patients developed recurrence in this study.
Discussion
Epiblepharon is a common disease in children, especially in Asian countries. Notably, 78% of affected children reportedly have no clinical symptoms because the eyelashes are often soft and sparse in young patients. However, the eyelashes gradually grow and harden after 3 years of age, which can contribute to the clinical symptoms of ocular irritation [13]. Accordingly, we typically recommend that children aged >3 years who exhibit ocular irritation undergo surgical correction as soon as possible.
Similar to epiblepharon, there is a high incidence of medial epicanthal folds in Asian countries [14,15,16]. More importantly, medial epicanthal folds are reportedly often present in association with severe epiblepharon [17]. Oh and Lee [2] indicated that the tangential vector of the medial epicanthal fold is the main cause of lower eyelid epiblepharon. Nevertheless, whether the optimal surgical approach involves treatment of epiblepharon alone or treatment of epiblepharon combined with medial epicanthal fold correction remains controversial [18]. Asamura et al. [8] suggested that epicanthoplasty is not always necessary for epiblepharon correction. Ni et al. [10] reported that patients who underwent a modified Hotz procedure combined with modified Z-epicanthoplasty had significantly better results than patients who underwent a modified Hotz procedure (98.6% vs. 78.0%, respectively).
The Hotz procedure and its modifications are among the most widely used methods for correction of epiblepharon. This procedure was designed to enable the excision of skin and orbicularis muscle tissue with tarsal fixation, and it generally produces a visible lower eyelid crease after surgery. However, patients in Asian countries do not anticipate the presence of a lower eyelid crease; thus, this crease constitutes an inappropriate cosmetic outcome. In a recent study [19], a rotating suture technique and L-plasty procedure were used to correct epiblepharon. However, the suture rotation technique and Hotz procedure may have been inappropriate for the patients with medial epicanthal folds in that study because the tangential vector could directly contribute to epiblepharon. Therefore, the undercorrection rate was relatively high because of the omission of epicanthoplasty. Woo et al. [20] reported that the undercorrection rate of the suture rotation technique in treatment of epiblepharon was 7.7%, and Sundar et al. [21] indicated that the undercorrection rate of the modified Hotz procedure for treatment of epiblepharon was 9.1%. The L-plasty procedure has been used for skin resection in the lower eyelid and medial canthal area. However, accurate removal of an L-shaped area of skin is difficult to achieve; if an insufficient amount of skin is removed, postoperative recurrence is likely. Conversely, if an excessive amount of skin is removed, the lower eyelid and medial epicanthal fold structures may be impaired, which leads to the onset of lower eyelid ectropion and obvious scars. Therefore, recurrence and scarring of the inner canthus are critical aspects of epiblepharon treatment that require urgent resolution.
Several methods are available to correct medial epicanthal folds, such as V-W plasty [22], Z-epicanthoplasty [23], Mustardé technique and its modifications [24]. However, the design of a skin flap is complex and time-consuming; thus, surgeons’ lack of experience may result in unsatisfactory cosmetic results. Some authors have advocated skin redraping for epicanthoplasty because this method is simple to design and easy to perform, with minimal scarring in the medial canthal area [25, 26]. Jung et al. [27] and Oh and Lee [2] reported that skin redraping was effective for correction of epiblepharon combined with a medial epicanthal fold. Based on the results of previous studies, skin redraping was used to improve the surgical outcomes, in the present study in conjunction with many modifications based on the senior author’s (N.S.) clinical experience.
Our study differs from prior studies in several important respects. First, the dissection performed between skin-orbicularis oculi muscles and orbicularis oculi muscles-superficial medial canthus ligament was sufficient. These procedures lead to structural remodelling of the lower eyelid and medial canthal area, which results in more effective and thorough correction of epiblepharon. Second, the previously described techniques did not involve preoperative design of the skin incision above the inner canthus. We performed skin resection of the triangular area within lines ‘a–b–e’. The precise and scientific preoperative determination of the excisional skin may effectively avoid unnecessary surgical procedures, such as repeated skin resection or prolonged incision. Third, minimal excision of excessive skin (width of 0.5–1 mm) beneath the trichiasis was removed compared with the amounts removed in other surgical procedures [8]. Flaps were then sutured in a tension-free pattern which could effectively avoid scar formation caused by excessive tissue removal. The scars were invisible with a VSS score of 1.1 ± 0.3. Fourth, isolation of the medial canthus ligament should be carefully considered because of the possibility of medial canthus ligament injury. Medial canthus ligament shorten [12] was performed for patients with severe conditions such as epicanthus inversus after careful evaluation by the surgeons. Finally, 286 patients were enroled in our study, which is a larger sample size than in previous studies; Jung et al. [27] evaluated 17 patients and Oh and Lee [2] evaluated 12 patients. Thus, our data may allow more robust conclusions. Follow-up examinations revealed that all patients had good outcomes, and no patients developed recurrence during the mean follow-up duration of 32.6 months.
Conclusion
Skin redraping is an effective long-term treatment for lower eyelid epiblepharon combined with a medial epicanthal fold. Successful surgical outcomes were achieved in all patients in terms of reduced cilia–cornea contact and improved clinical symptoms. In total, 272 patients or their guardians (95.1%) were very satisfied with their cosmetic outcomes. The postoperative scars were minimal or invisible, and no instances of recurrence were reported in this study.
Summary
What was known before
-
Skin Redraping was used to correct epicanthus fold before.
What this study adds
-
The structural remodelling of the lower eyelid and medial canthus area was obtained postoperatively, and structural remodelling was the fundamental change resulted in the following advantages. We put forward the skin resection of the “a-b-e” triangular region, the skin flaps were sutured without tension, and the incision above the inner canthus was well-formed along with curve of the upper eyelid crease. The precise determination of the skin removal may effectively avoid repeated skin resection or prolonged incision. Overcorrection of the lower eyelids was not necessary in our study, and retraction of revised eyelashes was not observed. Concept of minimally invasive was achieved, orbicularis oculi muscle was not removed, and the amount of skin excision was rare (0.5–1 mm). Medial canthus ligament shorten was not routinely performed for all patients, but for severe cases such as epicanthus inversus. The flaps in the lower eyelid and medial canthus area were sutured in a tension-free pattern which could effectively avoid scar formation. All 286 patients have Good results, and no incident of recurrence was observed in the 32.6 months of follow-up visit.
References
Noda S, Hayasaka S, Setogawa T. Epiblepharon with inverted eyelashes in Japanese children. I. Incidence and symptoms. Br J Ophthalmol. 1989;73:126–7.
Oh J, Lee K. Medial lower lid epiblepharon repair solely by skin-redraping medial epicanthoplasty. Br J Ophthalmol. 2014;98:1437–41.
Seo JW, Kang S, Ahn C, Esmaeli B, Sa HS. Non-incisional eyelid everting suture technique for treating lower lid epiblepharon. Br J Ophthalmol. 2018;102:1504–9.
Kim MS, Sa HS, Lee JY. Surgical correction of epiblepharon using an epicanthal weakening procedure with lash rotating sutures. Br J Ophthalmol. 2014;98:120–3.
Lin CC, Lai CC. Modified Hotz procedure with CO2 laser ablation of the orbicularis oculi muscle for epiblepharon. Can J Ophthalmol. 2019;55:63–7.
Khwarg SI, Choung HK. Epiblepharon of the lower eyelid: technique of surgical repair and quantification of excision according to the skin fold height. Ophthalmic Surg Lasers. 2002;33:280–7.
Hayasaka S, Noda S, Setogawa T. Epiblepharon with inverted eyelashes in Japanese children. II. Surgical repairs. Br J Ophthalmol. 1989;73:128–30.
Asamura S, Nakao H, Kakizaki H, Isogai N. Is it truly necessary to add epicanthoplasty for correction of the epiblepharon? J Craniofac Surg. 2013;24:1137–40.
Shin DH, Woo KI, Kim YD. Relationship between lower eyelid epiblepharon and epicanthus in Korean children. PLoS ONE. 2017;12:e0187690.
Ni J, Shao C, Wang K, Chen X, Zhou S, Lin H. Modified Hotz procedure combined with modified Z-Epicanthoplasty versus modified Hotz procedure alone for epiblepharon repair. Ophthalmic Plast Reconstr Surg. 2017;33:120–3.
Thompson CM, Sood RF, Honari S, Carrougher GJ, Gibran NS. What score on the Vancouver Scar Scale constitutes a hypertrophic scar? Results from a survey of North American burn-care providers. Burns. 2015;41:1442–8.
Lai CS, Lai CH, Wu YC, Chang KP, Lee SS, Lin SD. Medial epicanthoplasty based on anatomic variations. J Plast Reconstr Aesthet Surg. 2012;65:1182–7.
Guo L, Yuan F, Li B, Li JY, Wang CQ, Yan CH. Modified blepharosphincterectomy for congenital entropion in 24 cases. J Otolaryngol Ophthal Shandong Univ. 2014;28:77–8. In Chinese.
Park JI. Modified Z-epicanthoplasty in the Asian eyelid. Arch Facial Plast Surg. 2000;2:43–7.
Park JI. Z-epicanthoplasty in Asian eyelids. Plast Reconstr Surg. 1996;98:602–9.
Hyakusoku H, Fumiiri M. The square flap method. Br J Plast Surg. 1987;40:40–6.
Swan KC. The syndrome of congenital epiblepharon and inferior oblique insufficiency. Am J Ophthalmol. 1955;39:130–6.
Kashima T, Katori N, Yamada T, Imagawa Y, Nakauchi K. Epicanthoplasty simultaneous with epiblepharoplasty in cases of epiblepharon with epicanthus. Nippon Ganka Gakkai Zasshi. 2010;114:105–9.
Yan Y, Chen T, Wei W, Li D. Epiblepharon in Chinese children: relationships with body mass index and surgical treatment. J aapos. 2016;20:148–52.
Woo KI, Yi K, Kim YD. Surgical correction for lower lid epiblepharon in Asians. Br J Ophthalmol. 2000;84:1407–10.
Sundar G, Young SM, Tara S, Tan AM, Amrith S. Epiblepharon in East asian patients: the singapore experience. Ophthalmology 2010;117:184–9.
Fujiwara T, Maeda M, Kuwae K, Nishino K. Modified split V-W plasty for entropion with an epicanthal fold in Asian eyelids. Plast Reconstr Surg. 2006;118:635–42.
Wu S, Guo K, Xiao P, Sun J. Modifications of Z-epicanthoplasty combined with double-eyelid blepharoplasty in Asians. Aesthetic Plast Surg. 2018;42:226–33.
Yoon K. Modification of Mustarde technique for correction of epicanthus in Asian patients. Plast Reconstr Surg. 1996;97:245.
Oh YW, Seul CH, Yoo WM. Medial epicanthoplasty using the skin redraping method. Plast Reconstr Surg. 2007;119:703–10.
Pfeiffer MJ. Surgical treatment of medial epicanthus by skin replacement. Klin Monbl Augenheilkd. 2016;233:50–3.
Jung JH, Kim HK, Choi HY. Epiblepharon correction combined with skin redraping epicanthoplasty in children. J Craniofac Surg. 2011;22:1024–6.
Author information
Authors and Affiliations
Contributions
Study concept and design (GL, SN), acquisition of data (LNH, HAJ), analysis and interpretation of data (LNH, HAJ, WD), drafting of the manuscript (LNH, SN), critical revision of the manuscript for important intellectual content (LNH, SN), administrative, technical, or material support, study supervision (GL, SN).
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, N., He, A., Wu, D. et al. Skin redraping for correction of lower eyelid epiblepharon combined with medial epicanthal fold: a retrospective analysis of 286 Asian children. Eye 36, 844–849 (2022). https://doi.org/10.1038/s41433-021-01550-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01550-w
This article is cited by
-
Severe corneal involvement secondary to congenital lower eyelid epiblepharon
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)