Abstract
Background
To investigate the anatomical and functional results in eyes with peripapillary pachychoroid syndrome (PPS) undergoing photodynamic therapy (PDT).
Methods
A total of 25 eyes from 23 patients with PPS treated with PDT were retrospectively evaluated in this multicentric study. Main outcome measure was the proportion of eyes that achieved treatment success, defined as a decrease in both subretinal fluid (SRF) height and central subfield thickness (CST), at 3 months after PDT compared to baseline. Secondary outcomes were the change in CST, SRF, and best-corrected visual acuity (BCVA) 3 months after treatment and predictive factors for treatment success. When available, data between 3 and 12 months were also reviewed.
Results
Treatment success was achieved in 16 eyes (64%). In the total cohort, CST decreased significantly from 356 ± 118 µm at baseline to 282 ± 90 µm and 270 ± 91 µm at 1 and 3 months, respectively (p < 0.001). Maximal SRF height decreased significantly from 102 ± 83 µm at baseline to 38 ± 46 µm and 32 ± 42 µm at 1 and 3 months, respectively (p < 0.001), and remained stable at month 6 (29 ± 44 µm) and month 12 (23 ± 35 µm). BCVA improved significantly from baseline to month 3 (p = 0.021).
Conclusions
PDT can be considered an efficacious treatment option in patients with PPS. Prospective data with longer follow-up in a bigger cohort are needed in order to determine the optimal treatment algorithm in this relatively novel disease.
Similar content being viewed by others
Introduction
Pachychoroid is a relative novel term to define a specific phenotype characterized by the presence of dilated Haller layer veins (“pachyvessels”) with associated attenuation of the choriocapillaris and retinal pigment epithelium (RPE) dysfunction [1]. The pachychoroid disease spectrum (PDS) refers to a group of chorioretinal disorders sharing distinctive choroidal findings. Peripapillary pachychoroid syndrome (PPS) was recently described by Phasukkijwatana and co-authors as a variant of the PDS [2]. PPS is characterized by peripapillary choroidal thickening associated with nasal macular intraretinal fluid (IRF) and/or subretinal fluid (SRF) and occasionally optic disk oedema. The disease mainly affects elderly male patients [2].
Choroidal changes are thought to be underlying in PDS [3,4,5,6], and dilated peripapillary pachyvessels along with choroidal hyperpermeability are typical features of PPS [2]. While the findings on multimodal imaging have been well characterized, there has been limited investigation regarding the possible treatment strategies in patients with PPS yet. Photodynamic therapy (PDT) with verteporfin is the most efficient treatment option in reducing fluid leakage in patients with chronic central serous chorioretinopathy (CSC), a disease that has been found to be part of PDS [7, 8]. It has been shown that PDT has angio-occlusive properties leading to constriction of congested choroidal vessels and subsequent vascular remodelling [9, 10].
Recently, anti-vascular endothelial growth factor (VEGF) combined with full-dose PDT appeared to be effective in patients with pachychoroid neovasculopathy, which is another disease that is part of PDS [11]. In contrast to pachychoroid neovasculopathy, PPS does not exhibit evidence of macular and/or peripapillary choroidal neovascularisation (CNV), but resembles chronic CSC as both conditions show congested choroidal vessels and long-standing choroidal hyperpermeability. Therefore, there is a rationale for using PDT in the treatment of PPS. On this background, the aim of the present study was to investigate the anatomical and functional results in eyes with PPS undergoing PDT.
Methods
This was a retrospective, multicentre, cohort study including nine study centres. Institutional review board approval was obtained at each referral centres for a retrospective consecutive chart review. The study adhered to the guidelines of the Health Insurance Portability and Accountability Act and was performed in accordance with the tenets of the Declaration of Helsinki.
Study population
Medical records of patients with a diagnosis of PPS were retrospectively reviewed. Inclusion criteria were patients >18 and <75 years old with a PPS history. As per the previous literature [2], PPS was defined by the following findings on multimodal imaging: choroidal thickening that was more pronounced nasally compared to temporally to the fovea, presence of peripapillary IRF and/or SRF with underlying pachyvessels, mottled RPE alterations, as noted with colour fundus photography, spectral domain (SD) or swept source (SS) optical coherence tomography (OCT) and fundus autofluorescence. Only patients showing SRF or IRF in the fovea and underwent PDT were included in the study.
Enrolled patients were required to have had a complete ophthalmic exam and SD-OCT or SS-OCT at baseline (before PDT) and at follow-up visits with a minimum follow-up of 3 months after PDT. Eyes that received anti-VEGF injections, eplerenone or micropulse laser within 2 months prior to PDT were not included.
Exclusion criteria for this study were a history of intraocular surgery within the past 6 months, high refractive error (i.e. greater than −6 or +3 D), use of medication known to be associated with the occurrence cystoid macular oedema and the presence of other retinal diseases, or other masquerades based on OCT, fluorescein and indocyanine green angiography (FA and ICGA) findings. All eyes with low-quality OCT volume scans due to media opacities that prevented high-resolution imaging of the choroid, were also excluded from the study.
Clinical examination
For consecutive eligible patients, medical records and multimodal imaging findings were comprehensively reviewed. Data collected included patient demographics and Snellen best-corrected visual acuity (BCVA), which was converted to LogMAR for statistical analysis. Axial length (IOL Master 500, ZEISS Medical Technology, USA) was recorded when available.
In order to perform PDT, intravenous verteporfin (Visudyne, Novartis, Basel, Switzerland), was administered over a period of 10 min, and treatment was provided at 15 min after the start of the verteporfin infusion. The total light energy was set at 50 J/cm2 for the full-fluence approach and at 25 J/cm2 for half-fluence. Choice of PDT settings was determined by the treating physician. Patients were advised to avoid any direct sunlight exposure for 3 days after treatment. The PDT spot diameter was guided by FA and ICGA (Heidelberg Spectralis, Heidelberg Engineering, Germany) imaging to target FA-guided leaking spots and ICGA-guided choroidal hyperpermeability. The decision to perform either FA-guided or ICGA-guided PDT was made at the discretion of the treating physician.
Presence of any macular and/or peripapillary CNV was ascertained on multimodal imaging evaluation.
OCT analysis
OCT images were acquired using SD-OCT (Heidelberg Spectralis, Heidelberg Engineering, Germany) or SS-OCT (SS-OCT, DRI OCT Triton, Topcon Medical Systems, Oakland, New Jersey, USA). Patients were examined using the same machine at each visit. All OCT parameters were measured and graded at baseline visit (before PDT) and 1, 3, 6 and 12 months after PDT. For all patients, the horizontal 9- or 6-mm B-scan section through the central fovea was used for the analysis. OCT scans were included only when the peripapillary retina was clearly displayed. Presence and location of SRF and IRF were ascertained at baseline and each follow-up on the OCT B scan. Maximum SRF height was measured, whereas for IRF only a qualitative analysis was performed (present or absent). Central subfield thickness (CST) was defined as average retinal thickness of the circular area with 1-mm diameter around the foveal centre.
Choroidal thickness (CT) measurements were manually performed using EDI-OCT or SS-OCT images with the calliper tool provided by the embedded software as the distance between the Bruch’s membrane interface and the sclerochoroidal junction on the OCT scan. All the measurements were performed on a horizontal section passing through the central fovea at the following positions: (1) the centre of the fovea (subfoveal), (2) 1500 µm nasal to the foveal centre (N1.5), (3) 3000 µm nasal to the foveal centre (N3.0), (4) 1500 µm temporal to the foveal centre (T1.5), and (5) 3000 µm temporal to the foveal centre (T3.0). Presence of choroidal folds was also recorded.
Ellipsoid zone (EZ) and external limiting membrane (ELM) integrity were also evaluated subfoveally at baseline and each follow-up visit by two masked assessors (FT and DZ) who were blinded to the functional and anatomical results. In case of disagreement, the images were reviewed by a third grader (CI). Main outcome measure was the proportion of eyes that achieved treatment success at 3 months after PDT. Treatment success was defined as a decrease in both SRF maximal height and CST 3 months after PDT compared to baseline.
Secondary outcomes were the change in CST and SRF from baseline to 3 months after treatment, BCVA change 3 months after treatment, and predictive factors for treatment success. Moreover, data available between 3 and 12 months were reviewed.
Statistical analysis
The demographics and clinical characteristics of our study cohort were evaluated using traditional descriptive methods. Changes in BCVA, CST and SRF from baseline compared to month 1, 3, 6 and 12 months were tested by a paired t-test. Univariate analysis for outcome measures (CST and SRF decrease) was done using a t-test for continuous variables and Fisher’s Exact Test for binary variables by including the following variables: (1) eye, (2) gender, (3) CST, (4) SRF height, (5) presence of IRF, (6) ELM and EZ integrity, (7) CT at all measurement points, (8) previous treatments and (9) PDT settings (half-dose, half-fluence, half-dose half-fluence). Predictors with a p value ≤ 0.001 in univariate analysis were included in the final logistic regression model.
A forward stepwise selection procedure that retained only those variables with p < 0.05 was applied. ANOVA with repeated measures was used to investigate the correlation between treatment success and change in BCVA, CST, CT and SRF over time. Statistical analysis was performed by the Statistical Laboratory School of Mathematics (Tel Aviv University, Tel Aviv, Israel). All statistics were computed with SPSS statistical package version 26.0.
Results
A total of 25 eyes from 23 patients were included in the study. Mean age at baseline was 63.6 ± 10.0 years, 23 patients (92%) were male. Baseline characteristics are depicted in Table 1. At baseline mean CST was 356 ± 118 µm, and CT was 445 ± 103 µm subfoveally, 454 ± 110 µm (N1.5), 326 ± 133 µm (N3), 340 ± 116 µm (T1.5) and 292 ± 96 µm (T3) (p < 0.001). Neither baseline CST nor SRF height correlated with CT at any measurement point. At baseline, choroidal folds were present in six eyes (24%). Baseline foveal EZ layer was intact in two eyes (8%) and ELM in ten eyes (40%).
Nine eyes (36%) were treatment naïve, seven eyes (28%) had previously received intravitreal anti-VEGF injections, six (24%) had received oral eplerenone therapy and three eyes (12%) had previous micropulse laser. No eyes showed evidence of macular and/or peripapillary CNV on multimodal imaging evaluation. Axial length was available in 12 eyes with a mean length of 22.1 ± 1.1 mm.
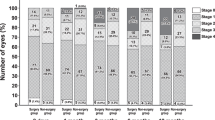
PDT regimens used were full-dose half-fluence in 14 cases (56%), half-dose half-fluence in 7 cases (28%), half-dose full-fluence in 3 cases (12%) and full-dose full-fluence in 1 case (4%). Mean follow-up duration after PDT was 9 ± 2.7 months.
Anatomical and functional outcomes
Anatomical and functional outcomes of eyes receiving PDT are summarized in Table 2 and Fig. 1. Treatment success, i.e. reduction in both CST and SRF height, was achieved in 16 eyes (64%). All study eyes had foveal SRF at baseline and a complete resolution of the subfoveal fluid at 3 months after PDT was achieved in ten eyes (40%). Overall, 17 eyes also had peripapillary SRF which resolved in 8 eyes (47%). Overall, 19 eyes presented IRF at baseline of which 10 had only peripapillary cysts and 9 had peripapillary and foveal intraretinal cysts. At 3 months after treatment, 9 eyes showed complete resolution of IRF.
A Late-phase fluorescein angiography (FA) illustrates speckled hyperfluorescence with staining and focal leakage in the macular and peripapillary area. B Mid- to late-phase indocyanine green angiography shows areas of indistinct hyperfluorescence, indicative of increased choroidal hyperpermeability. C Baseline spectral domain optical coherence tomography (SD-OCT) scan (white line on FA) through the optic disc shows a thickened peripapillary choroid, with subretinal fluid (SRF) and few intraretinal cysts in the nasal region. D Baseline 30° SD-OCT foveal scan confirms a thicker nasal choroid with some pachyvessels and SRF. E At the 3-month follow-up visit, SD-OCT scan shows complete resolution of SRF and central subfield thickness reduction from 227 to 212 µm. Best-corrected visual acuity improved from 20/32 to 20/25.
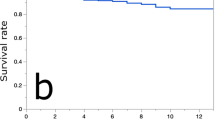
Maximal SRF height decreased significantly from 102 ± 83 µm at baseline to 38 ± 46 µm and 32 ± 42 µm at 1 and 3 months, respectively (p < 0.001), and remained stable at month 6 (29 ± 44 µm) and month 12 (23 ± 35 µm) in the total cohort. Mean baseline maximal SRF height was significantly greater in the treatment success group (141 vs. 36 µm, p < 0.001), and so was the decrease in SRF after treatment (p < 0.001, Fig. 2).
In the complete cohort, CST decreased significantly from 356 ± 118 µm at baseline to 282 ± 90 µm and 270 ± 91 µm at 1 and 3 months, respectively (p < 0.001), and remained stable at month 6 (269 ± 81 µm) and month 12 (276 ± 145 µm). Baseline CST was comparable in the treatment success and no-success group (p = 0.718, Fig. 3). Although mean CST decrease was greater in the treatment success group (−114 µm vs. −39 µm), the difference did not reach statistical significance (p = 0.097).
Note that in the treatment success group, baseline SRF height was significantly greater (141 vs. 36 µm, p < 0.001), and so was the difference between the two groups over time (p < 0.001). The most significant improvement was seen at 1 month after PDT and remained stable over the course of 12 months.
Mean BCVA was 0.59 ± 0.44 LogMAR (20/80) at baseline, 0.56 ± 0.51 LogMAR (20/80) at month 1 and 0.51 ± 0.45 LogMAR (20/63) at month 3. The improvement from baseline to month 3 was statistically significant (p = 0.021). Baseline BCVA and BCVA change after treatment were similar between the treatment success and no-success group (p = 0.905 and p = 0.677, respectively). Visual outcomes for both groups have been included in Table 2. BCVA decreased to 0.60 ± 0.46 LogMAR at month 6 and 0.65 ± 0.39 LogMAR at month 12 (p = 0.982).
Predictive factors for treatment success
Eyes that achieved treatment success at 3 months had significantly greater SRF height at baseline compared to eyes that did not achieve treatment success (p = 0.028). Logistic regression analysis revealed that eyes with an SRF height of 65 µm or more had a significantly greater chance to achieve treatment success compared to eyes with a lower SRF height (p = 0.044, OR = 1.048, 95% confidential interval 1.001–1.096).
Treatment success was independent from the following baseline parameters: CT, CST (p = 0.097), IRF presence (p = 0.364), integrity of the EZ (p = 0.265) and ELM (p = 0.073), BCVA (p = 0.053), history of previous treatment (p = 0.343) and PDT settings used (p = 0.495).
Discussion
To the best of our best knowledge, this is the first study to evaluate the efficacy of PDT in patients with PPS. Our results show a significant decrease in SRF in 16 eyes (64%), with complete resolution of the fluid in 10 eyes (40%), and a significant improvement in BCVA following treatment.
The entity of PPS was only recently defined as a distinct phenotype within the PDS [2]. PPS can present with variable severity: while some cases may be incidentally detected and present with only mild peripapillary IRF/SRF without foveal involvement, others may experience profound visual loss as result of chronic SRF/IRF accumulation and photoreceptor damage. To date, there is no evidence regarding the optimal clinical management and treatment for these rare and challenging cases. Phasukkijwatana et al. were the first to describe and define PPS, and their study included 31 eyes from 16 patients focusing on clinical features [2]. Data regarding treatment were available in eight eyes. Response to intravitreal anti-VEGF injections and topical or systemic carbonic anhydrase inhibitors was described as not efficacious by these authors. However, data regarding fluid type and quantity were not provided.
In the current study, we have shown a beneficial response to PDT in a relatively large cohort of patients with this rare condition in 25 eyes from 23 patients. A possible explanation for the efficacy of PDT might be found in the pathogenesis of the most frequently occurring disease within the PDS: CSC. Although clinical manifestations of CSC and PPS are different, they share common features and are believed to present different stages of one common pathogenic process [1, 12]. Both are characterized by a dysfunctioning pachychoroid, which results in a leaky outer blood–retina barrier at the level of the RPE. PDT has been shown to be the most efficacious therapy for chronic CSC [7, 8]. Analogy in pathogenesis and anatomical features built the rationale for us to use of PDT in the treatment of PPS. Nevertheless, the differences between the two PDS diseases may reflect the lower success rate of the PDT in PPS.
Several authors analysed the presence of cystoid retinal degeneration in the setting of chronic CSC [13,14,15]. Mohabati et al. reported a complete SRF absorption in 82% of eyes with chronic CSC after PDT with a resolution of the cystoid retinal degeneration in 37% of cases [13]. At month 3, we had a complete absorption of the SRF and IRF in ten eyes (40%) and nine eyes (36%), respectively. Therefore, we conclude that PPS patients may be less likely to achieve a complete resolution of the serous retinal detachment if compared to those with chronic CSC.
Treatment effect of PDT in CSC has been explained by choroidal remodelling, decrease of fluid leakage from the choroid via the defective RPE outer blood–retina barrier to the subretinal space [8]. A reduction of the total choroidal volume and specifically in the luminal choroidal area in the absence of associated choroidal stromal alterations, seems to confirm the hypothesis that large choroidal vessels are the main target of PDT [9].
Similarly, in the current study, we targeted hyperpermeable choroidal vessels by angiography-guided PDT. However, this theory stays to be proven in the setting of PPS by measuring the choroidal vascularity index and its subcomponents before and after treatment, although due to the presence of a very thick choroid in PPS patients, it may be difficult to measure [16, 17].
While there was a statistically significant improvement in both mean CST and SRF after treatment in the total cohort, eyes with greater SRF height at baseline were more likely to achieve treatment success, which was defined as a reduction in both CST and SRF. Specifically, a minimum height of 65 µm of SRF at baseline was predictive for treatment success. The role of persistent SRF is well known from chronic CSC. It leads to progressive irreversible photoreceptor damage with detrimental effect on vision [18,19,20]. In the absence of macular and/or peripapillary CNV, persistent accumulation of SRF in PDS can be attributed to a leaky outer blood–retina barrier due to irreversible damage at the level of the RPE, induced by a primary dysfunction of the underlying choroid [1]. We hypothesize that a greater amount of SRF at baseline might be a surrogate marker for more active leakage and explain the better response in these eyes. A complete resolution of SRF should be the purpose of treatment, to optimize the likelihood of recovery of retinal sensitivity [7, 8].
All other baseline parameters were comparable between the treatment success and no-success groups, including the different PDT types or protocols.
Our study was designed to assess a morphologic end point, namely a combined reduction of SRF and CST at 3 months. Treatment success was achieved in 16 eyes (64%), although a complete SRF resolution occurred only in 10 eyes (40%). Mean improvement in both parameters was statistically significant in the whole cohort at month 3 and remained stable until month 12. Our results indicate a sustained anatomical benefit of PDT in PPS which might be explained by transient choroidal ischemia and subsequent choroidal vascular remodelling caused by PDT, as previously described for CSC [10]. Conversely, BVCA improvement was significant only at month 3, indicating a limited functional benefits of the PDT in patients with PPS.
Limitations of our study include its retrospective design, relatively short follow-up and small cohort, and previous treatments administered. PDT settings differed between centres. Moreover, we did not include OCT-angiography analysis in the current study. Choroidal flow evaluation might add further information about the pathogenesis and susceptibility to PDT [21]. Lately, OCT-angiography reports have shown that PDT induces selective occlusion of the choriocapillaris leading to decreased leakage [22, 23].
In conclusion, the results of this pilot study show that PDT is efficacious in the treatment of patients with PPS. Nevertheless, the functional improvement in terms of BCVA seems to reduce over the time. Intervention at an early disease stage should be considered in patients with persistent SRF, when the outer retina is still preserved. Prospective data with longer follow-up in a bigger cohort are needed in order to determine the treatment algorithm in this relatively novel disease.
Summary
What was known before
-
Peripapillary pachychoroid syndrome is included in the pachychoroid spectrum disease.
-
Peripapillary pachychoroid syndrome can manifest with intra/subretinal fluid.
What this study adds
-
Photodynamic therapy is a valid treatment option for peripapillary pachychoroid syndrome.
-
Photodynamic therapy leads to a significant subretinal fluid reduction/reabsorption, even though in selected cases it may not be resolutive.
References
Cheung CMG, Lee WK, Koizumi H, Dansingani K, Lai TYY, Freund KB. Pachychoroid disease. Eye. 2019;33:14–33.
Phasukkijwatana N, Freund KB, Dolz-Marco R, Al-Sheikh M, Keane PA, Egan CA, et al. Peripapillary pachychoroid syndrome. Retina. 2018;38:1652–67.
Giray Ersoz M, Arf S, Hocaoglu M, Muslubas IS, Karacorlu M. Indocyanine green angiography of pachychoroid pigment epitheliopathy. Retina. 2017;38:1668–74.
Koizumi H, Yamagishi T, Yamazaki T, Kinoshita S. Relationship between clinical characteristics of polypoidal choroidal vasculopathy and choroidal vascular hyperpermeability. Am J Ophthalmol. 2013;155:305–313.e1.
Iida T, Kishi S, Hagimura N, Shimizu K. Persistent and Bilateral choroidal vascular abnormalities in central serous chorioretinopathy. Retina. 1999;19:508
Peiretti E, Iovino C. Indocyanine green angiography. In: Central serous chorioretinopathy. Burlington: Academic Press; 2019. p. 97–113.
van Dijk EHC, Fauser S, Breukink MB, Blanco-Garavito R, Groenewoud JMM, Keunen JEE, et al. Half-dose photodynamic therapy versus high-density subthreshold micropulse laser treatment in patients with chronic central serous chorioretinopathy: the PLACE Trial. Ophthalmology. 2018;125:1547–55.
van Rijssen TJ, van Dijk EHC, Yzer S, Ohno-Matsui K, Keunen JEE, Schlingemann RO, et al. Central serous chorioretinopathy: towards an evidence-based treatment guideline. Prog Retin Eye Res. 2019;73:100770.
Iovino C, Au A, Chhablani J, Parameswarappa DC, Rasheed MA, Cennamo G, et al. Choroidal anatomic alterations after photodynamic therapy for chronic central serous chorioretinopathy: a Multicenter Study. Am J Ophthalmol. 2020;217:104–13.
Chan WM, Lam DSC, Lai TYY, Tam BSM, Liu DTL, Chan CKM. Choroidal vascular remodelling in central serous chorioretinopathy after indocyanine green guided photodynamic therapy with verteporfin: A novel treatment at the primary disease level. Br J Ophthalmol. 2003;87:1453–8.
Kitajima Y, Maruyama-Inoue M, Ito A, Sato S, Inoue T, Yamane S, et al. One-year outcome of combination therapy with intravitreal anti-vascular endothelial growth factor and photodynamic therapy in patients with pachychoroid neovasculopathy. Graefe’s Arch Clin Exp Ophthalmol. 2020;258:1279–85.
Siedlecki J, Schworm B, Priglinger SG. The pachychoroid disease spectrum-and the need for a uniform classification system. Ophthalmol Retin. 2019;3:1013–5.
Mohabati D, Hoyng CB, Yzer S, Boon CJF. Clinical characteristics and outcome of posterior cystoid macular degeneration in chronic central serous chorioretinopathy. Retina. 2020;40:1742–50.
Piccolino FC, De La Longrais RR, Manea M, Cicinelli S, Ravera G. Risk factors for posterior cystoid retinal degeneration in central serous chorioretinopathy. Retina. 2008;28:1146–50.
Sahoo NK, Mishra SB, Iovino C, Singh SR, Munk MR, Berger L, et al. Optical coherence tomography angiography findings in cystoid macular degeneration associated with central serous chorioretinopathy. Br J Ophthalmol. 2019;103:1615–8.
Agrawal R, Ding J, Sen P, Rousselot A, Chan A, Nivison-Smith L, et al. Exploring choroidal angioarchitecture in health and disease using choroidal vascularity index. Prog Retin Eye Res. 2020;77:100829.
Iovino C, Pellegrini M, Bernabei F, Borrelli E, Sacconi R, Govetto A, et al. Choroidal vascularity index: an in-depth analysis of this novel optical coherence tomography parameter. J Clin Med. 2020;9:595.
Loo RH, Scott IU, Flynn HWJ, Gass JDM, Murray TG, Lou Lewis M. et al. Factors associated with reduced visual acuity during long-term follow-up of patients with idiopathic central serous chorioretinopathy. Retina. 2002;22:19–24.
Breukink MB, Dingemans AJ, den Hollander AI, Keunen JE, MacLaren RE, Fauser S, et al. Chronic central serous chorioretinopathy: long-term follow-up and vision-related quality of life. Clin Ophthalmol. 2016;11:39–46.
Iovino C, Chhablani J, Parameswarappa DC, Pellegrini M, Giannaccare G, Peiretti E. Retinal pigment epithelium apertures as a late complication of longstanding serous pigment epithelium detachments in chronic central serous chorioretinopathy. Eye. 2019;33:1871–6.
Demirel S, Özcan G, Yanık Ö, Batıoğlu F, Özmert E. Vascular and structural alterations of the choroid evaluated by optical coherence tomography angiography and optical coherence tomography after half-fluence photodynamic therapy in chronic central serous chorioretinopathy. Graefe’s Arch Clin Exp Ophthalmol. 2019;257:905–12.
Xu Y, Su Y, Li L, Qi H, Zheng H, Chen C. Effect of photodynamic therapy on optical coherence tomography angiography in eyes with chronic central serous chorioretinopathy. Ophthalmologica. 2017;237:167–72.
Cennamo G, Montorio D, Comune C, Clemente L, Iovino C, Carandente R, et al. Study of vessel density by optical coherence tomography angiography in patients with central serous chorioretinopathy after low-fluence photodynamic therapy. Photodiagnosis Photodyn Ther. 2020;30:101742.
Acknowledgements
The authors thank Ms. Ilana Gelernter for the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Financial disclosures: GQ: Alimera Sciences (Alpharetta, Georgia, USA), Allergan Inc (Irvine, California, USA), Amgen (Thousand Oaks,USA), Bayer Shering-Pharma (Berlin, Germany), Heidelberg Engineering Inc (Heidelberg, Germany), KBH (Chengdu; China), LEH Pharma (London, UK), Lumithera (Poulsbo; USA), Novartis (Basel, Switzerland), Sandoz (Berlin, Germany), Sifi (Catania, Italy), Sooft-Fidea (Abano, Italy), Zeiss (Dublin, USA). EB: Zeiss (Dublin, USA), CenterVue (Padova, Italy). RS: Zeiss (Dublin, USA). AL: Allergan Inc (Irvine, California, USA), Bayer (Berlin, Germany), Beyeonics (Haifa, Israel), Forsightlabs (CA, USA), Notal Vision (Tel Aviv, Israel), Novartis (Basel, Switzerland), Roche (Basel, Switzerland). DZ: Allergan Inc (Irvine, California, USA), Bayer (Berlin, Germany). The remaining authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Iovino, C., Peiretti, E., Tatti, F. et al. Photodynamic therapy as a treatment option for peripapillary pachychoroid syndrome: a pilot study. Eye 36, 716–723 (2022). https://doi.org/10.1038/s41433-021-01515-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01515-z