Abstract
Objective
To determine the relationship between visual impairment and other disabilities in a developing country.
Methods
In this cross-sectional ancillary study, all individuals 50 years and older in 18 communities in the Chitwan region of Nepal were administered visual acuity screening and the Washington Group Short Set (WGSS) of questions on disability. The WGSS elicits a 4-level response for six disability domains: vision, hearing, walking/climbing, memory/concentration, washing/dressing, and communication. The association between visual impairment and disability was assessed with age- and sex-adjusted logistic regression models.
Results
Overall, 4719 of 4726 individuals successfully completed visual acuity and disability screening. Median age of participants was 61 years (interquartile range: 55–69 years), and 2449 (51.9%) were female. Participants with vision worse than 6/60 in the better-seeing eye were significantly more likely to be classified as having a disability in vision (OR 18.4, 95% CI 9.9–33.5), walking (OR 5.3, 95% CI 2.9–9.1), washing (OR 9.4, 95% CI 4.0–21.1), and communication (OR 5.0, 95% CI 1.7–13.0), but not in hearing (OR 0.6, 95% CI 0.006–2.2) or memory (OR 2.2, 95% CI 0.7–5.1).
Conclusions
Visually impaired participants were more likely to self-report disabilities, though causality could not be ascertained. Public health programs designed to reduce visual impairment could use the WGSS to determine unintended benefits of their interventions.
Similar content being viewed by others
Introduction
Globally at least 2.2 billion people have visual impairment. Of these, at least 1 billion have visual impairment that has yet to be addressed or could have been prevented [1]. The 2017 Global Burden of Diseases, Injuries, and Risk Factors study, which estimated years lived with disability to provide context about the burden of nonfatal diseases, found vision loss to be the third leading impairment for both sexes [2]. Moreover, the burden of visual impairment is forecast to increase substantially by 2050 as large portions of the global population age and life expectancy improves [3]. The high burden of visual impairment extends to the economic realm as well, leading to billions of dollars in productivity losses [4].
The burden of visual impairment is not distributed evenly. For example, the prevalence of distance visual impairment in low- and middle-income countries is estimated to be four times higher than that of high-income regions [5]. Furthermore, older individuals, women, and rural residents have also been found to have a higher risk of visual impairment [6,7,8]. Disabilities unrelated to vision are also thought to be associated with visual impairment, although supporting data are relatively sparse [1].
Disability refers to the impairments, limitations and restrictions that a person faces while interacting with their environment—physical, social, or attitudinal [1]. The importance of disability has received increased attention in recent years, but data on the relationship between visual impairment and disability are scant [9]. Several previous studies have examined the relationships between visual function, visual disability, and activities of daily living in high-income countries, and one study assessed self-reported disability and visual impairment using the World Health Organization Disability Assessment Schedule in six lower- and middle-income countries [10,11,12,13]. The results from these studies suggest an association between disability and visual impairment, but data from other settings would add confidence to the findings.
In the present study, we evaluated the relationship between visual impairment and self-reported disability using a standardized disability questionnaire developed by the United Nations Washington Group (WG) on Disability Statistics and recommended by the World Bank for household surveys [14]. We conducted the study in a resource-limited setting in Nepal, where the burden of both visual impairment and disability would be expected to be relatively high [5]. We hypothesized that visual impairment would be associated with higher self-reported disability.
Materials and methods
Study design and settings
The study took place in the Chitwan district of Nepal from 16 January, 2018 to 22 December, 2019. At the time, the district was divided into numerous village development committees (VDC), which were in turn subdivided such that each VDC consisted of nine wards. As part of a cluster-randomized trial, 36 wards from 6 VDCs in the Chitwan district were randomized to receive a community-based eye disease screening intervention or no screening intervention. Screening visits were performed by the same screening team in a central area of the community. The present report is an ancillary cross-sectional study conducted only in the 18 communities randomized to the screening intervention; this ancillary study compares the results of a visual acuity assessment and a disability questionnaire completed during the screening visit. The study adhered to the Strengthening of the Reporting of Observational Studies in Epidemiology guidelines.
Participants
All individuals aged 50 years or older who were found to be residing within the randomized communities on a door-to-door census conducted 1–4 weeks prior to the screening visit were invited to participate in the study. All consenting participants reported to a central location in the community to undergo visual acuity screening and a fill out a disability questionnaire.
Visual acuity
Each eye was tested separately using a visual acuity screening card developed by Nepal Netra Jyoti Sangh (Kathmandu, Nepal); the foldable card had four faces, three of which contained a single tumbling E optotype of a different size (i.e., corresponding to visual acuities of 6/60, 6/18, and 6/9 when tested at 6 m). Each optotype size was presented at 6 m in four arbitrary directions at the discretion of the tester, with a successful effort requiring a correct answer for all four directions. Testing was conducted in a well-lit environment outside of direct sunlight. The right eye was tested first with the left eye occluded and then the left eye was tested with the right eye occluded. Participants were tested with spectacle correction, if any was available (i.e., the WHO’s definition of presenting visual acuity), followed by pinhole occlusion. Visual acuity was defined at the person level as the smallest optotypes that could be read in the better-seeing eye, either with spectacle correction if available (i.e., presenting visual acuity) or through a pinhole occluder (i.e., pinhole acuity).
Disability
The Washington Group Short Set of questions on disability (WGSS) was translated into Nepali and administered verbally to each participant [15]. This questionnaire elicits a 4-level response (i.e., “no difficulty,” “some difficulty,” “a lot of difficulty,” or “cannot do at all”) for disabilities in six domains: vision, hearing, walking/climbing, memory/concentration, washing/dressing, and communication (Supplementary Fig. 1). The questionnaire was administered verbally to each participant.
Statistical considerations
The exposure of interest was presenting visual acuity in the better-seeing eye, dichotomized at three different thresholds (i.e., 6/9, 6/18, and 6/60—the three thresholds screened with the visual acuity card) indicating the ability versus the inability to see that line of vision. The outcome of interest was the presence of disability for each domain, with disability defined as “a lot of difficulty” or “cannot do at all” in at least one domain on the WGSS, as recommended by the Washington Group on Disability Statistics [16, 17]. Logistic regression models were constructed for each disability domain outcome and adjusted for the potential confounders of sex, age in years, and presence of self-reported diabetes mellitus (i.e., an indicator of systemic co-morbidity), with separate models to assess each of the visual acuity thresholds. Individuals with missing data were excluded from the analysis. In a secondary analysis, the prevalence of disability and visual impairment was calculated for each community, and community-level associations assessed with a linear regression weighted by the number of respondents per community. Intraclass correlation coefficients (ICC) were calculated to determine the degree to which disability and visual impairment clustered within communities [18]. The sample size was based on the underlying clinical trial, and therefore, fixed; we planned to enrol at least 4500 people across the 18 communities. Assuming a 2% prevalence of blindness based on a prior study from Nepal [19], a 5% prevalence of disability in people without visual impairment, and an alpha of 0.05, then this sample size would provide ~80% power to estimate a 7.5% greater prevalence of disability in the visually impaired group. Centre values for descriptive statistics are reported as medians and all odds ratios (ORs) are presented with their corresponding 95% confidence intervals (CIs). The data met underlying assumptions for logistic regression models. Analyses were performed with R version 3.6.0 (R Foundation for Statistical Computing, Vienna, Austria) [20].
Ethics
The study received Institutional Review Board approval from the University of California San Francisco, and ethical approval from Nepal Netra Jyoti Sangh, and the Nepali Health Research Council. The study adhered to the guidelines of the Declaration of Helsinki. Verbal informed consent was obtained for all participants; verbal consent was approved by ethical committees due to the high levels of illiteracy in the study area. No stipend was provided.
Results
A total of 4726 individuals aged 50 years or older presented for examination, of which 4719 successfully completed visual acuity and disability screening. The median age of participants successfully completing screening was 61 years (interquartile range: 55–69 years), and 2449 (51.9%) were female.
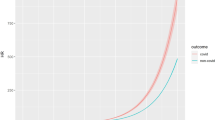
The best presenting visual acuity in the better-seeing eye was 6/9 in 3101 (65.7%) participants, 6/18 in 1148 (24.3%) participants, 6/60 in 369 (7.8%) participants, and worse than 6/60 in 101 (2.1%) participants. When disability was defined using the WG recommendation of “a lot of difficulty” or “inability” in at least one domain, 233 people (5.0%) reported having a disability. When disability was defined as “some difficulty” or worse in one or more domains, 842 people (17.8%) reported having a disability. Age- and sex-stratified results of the vision screening and disability questionnaire are summarized in Table 1. As depicted in Fig. 1, both visual impairment and the number of reported disabilities became significantly more prevalent with advanced age but did not differ substantially by sex. The proportion of people with a disability increased as presenting vision in the better-seeing eye worsened, regardless of whether the threshold for disability was defined as “some” difficulty or “a lot” of difficulty (Fig. 2).
Presenting acuity results were classified into four ordered groups based on the best visual acuity line successfully read. Bars show the distribution of disability scores within each vision group. Note limit of the y-axis is set to 40% so as to better visualize the distribution of disability scores within each vision group.
Participants with worse presenting visual acuity were more likely to self-report a disability, with greater magnitudes of association for those with more advanced vision loss (Fig. 3). For example, compared to those with better vision, participants whose presenting vision was worse than 6/60 in the better-seeing eye were more likely to be classified as having a disability in the vision (OR 18.4, 95% CI 9.9–33.5), walking (OR 5.3, 95% CI 2.9–9.1), washing (OR 9.4, 95% CI 4.0–21.1), and communication (OR 5.0, 95% CI 1.7–13.0) domains. In contrast, disabilities in the hearing and memory domains had weaker associations with visual impairment (OR 0.6, 95% CI 0.06–2.2 and OR 2.2, 95% CI 0.7–5.1, respectively). Conclusions did not change when analyses were repeated with pinhole-corrected visual acuity (Supplementary Fig. 2).
Each dot represents the odds ratio from an age- and sex-adjusted logistic regression that models the presence of disability as a function of a dichotomous visual acuity exposure variable; bars represent 95% confidence intervals. Visual acuity groups indicate the best presenting visual acuity achieved (relative to those not achieving the respective acuity). The horizontal dashed line represents an odds ratio of 1.
The community prevalence of visual impairment (i.e., visual acuity worse than 6/60) did not significantly correlate with the community prevalence of disability (i.e., “a lot of difficulty” or “unable to do” in at least one domain of the WGSS), with each 10 percentage-point increase in the prevalence of visual impairment corresponding to a 3.1 percentage-point reduction (95% CI 25.6-point reduction to 19.4-point increase) in the prevalence of disability (P = 0.77, regression weighted by a number of respondents per community; Fig. 4). Other thresholds of visual acuity impairment and disability were likewise not statistically significant. The magnitude of within-community clustering, as assessed by the ICC, was estimated to be 0.007 (95% CI 0–0.17) for the presence of at least one disability and 0.06 (95% CI 0–0.42) for presenting visual acuity impairment worse than 6/60.
Disability was defined as “a lot of difficulty” or “unable to do” in one or more domains of the disability questionnaire and visual impairment as best presenting acuity worse than 6/60. Each point represents a study community, sized proportional to the number of community members tested. The best-fit line from a linear regression of community-level data is shown as a dashed line.
Discussion
This study’s principal finding was that people with visual impairment were more likely to have other self-reported disabilities. The likelihood of an association was strengthened by the observation of a dose response, with greater odds of disability for worsening states of visual impairment (Fig. 3).
We found that ~2.1% of the population 50 years or older in this region of Nepal had a presenting visual acuity worse than 6/60 in the better-seeing eye. Although the visual acuity thresholds and age groups of this study differ somewhat from prior studies, the extent of visual impairment observed here was generally in line with previous estimates of visual impairment in Nepal and indicates a relatively large burden of visual impairment in this region of Nepal [19, 21, 22].
Several previous studies found lower estimates of social and physical functioning in those with visual impairment, but these studies used a variety of measurement tools and did not focus specifically on disability [12, 23,24,25,26,27]. For example, one study using data collected from 2007 to 2010 in six lower- and middle-income countries found an association between visual impairment and self-reported disability as assessed by the World Health Organization Disability Assessment Schedule 2.0 [13]. In the years since this study was completed, consensus has grown to support the United Nations WGSS of disability questions, a relatively quick 6-item questionnaire [28]. Use of this instrument in the present study enhances its generalizability and provides valuable, internationally comparable data. It was simple to incorporate into the study, added little time to fieldwork, and will help provide context to the main results of the clinical trial. We recommend its use by other research groups.
We found that approximately 5% of participants 50 years and older reported a lot of difficulty or inability in at least one of the tested disability domains, with rapidly increasing prevalence as the population aged (Fig. 1A). Of the queried domains, self-reported difficulty with vision was most common. Reduced visual acuity was significantly associated with self-reported disabilities in walking, washing, and communication, but not hearing or memory (Fig. 3). Although this study cannot assess causality, it is reasonable to speculate that difficulty with vision would make walking and washing more challenging and could also hamper the ability to initiate and maintain communication. In contrast, vision has a less plausible direct causal impact on hearing loss, although both are associated with age. Of note, prior work has shown a longitudinal association between vision loss and cognitive decline [29,30,31]. The lack of an association between vision loss and memory in the present study could be due to several factors, including inadequate sample size, inability of a single question to accurately assess cognition when compared to the neuro-psychiatric tests used in other studies, and difficulty obtaining accurate responses from those who suffer severe deficits in cognition.
Despite the inability to assess causality in the present study, it is tempting to speculate whether interventions to improve visual acuity in a population could also reduce other perceived disabilities, especially since vision correction is likely a more easily modifiable risk factor than others for the disabilities elicited in this study. Future randomized trials of interventions that specifically target visual impairment, but not other disabilities, might consider including disability assessments as secondary outcomes.
The present study found that 5.0% of participants 50 years or older reported at least 1 disability when the threshold for a disability was set to “a lot” of difficulty (i.e., the cutoff recommended by the WG), and 17.8% when the threshold was defined as “some” difficulty in one or more domains (the definition employed by some other groups). These estimates are relatively consistent with population-based studies from Peru, Morocco, and Uganda, although the study definitions and/or reporting of outcomes are not exactly the same between the studies, making a direct comparison difficult [32,33,34]. These previous studies have found visual disability to be either the most common or second most common disability among the six tested domains, and have found an increasing prevalence of disability with age—each of which was also confirmed in the present study.
We found that community-level estimates of visual impairment did not correlate strongly with community-level disability prevalence, and that the magnitude of within-community clustering was minimal. This suggests that studies based on cluster sampling that seek to investigate the relationship between visual impairment and disability would likely be better off using an individual-level rather than community-level outcome.
Several limitations of the present study should be noted. Visual acuity was tested at only three acuity levels, limiting the granularity of the data and thus the statistical power. As stated above, the observational nature of the study precluded conclusions about causality. Ordinal multi-category data on disability and visual acuity impairment were dichotomized, a simplification that reduced statistical power but also made for more parsimonious regression models that were easier to interpret. While the regression models were adjusted for self-reported diabetes, data on other potential confounders of the relationship between vision and disability were not collected, preventing a more detailed multivariable analysis. Finally, while the inclusion of a random set of communities increased the study’s generalizability within this region of Nepal, the generalizability of the findings outside of Nepal is not clear: it is possible that visual impairment has a stronger magnitude of association with other disabilities in a place like Nepal with limited access to health services.
In summary, we found a significant association between visual impairment and disabilities in seeing, walking, washing, and communication, with higher odds of disability for groups with more advanced visual impairment in this area of Nepal. The causality of this association remains unclear. Incorporation of the WGSS into a community-based study of a blindness prevention program was quick and easy, and well accepted by the study participants. Inclusion of disability questions could be worthwhile for future studies of interventions for visual impairment, either to provide context about the characteristics of the study population or as a secondary outcome.
Summary
What was known before
-
Disabilities unrelated to vision are thought to be associated with visual impairment although data is scarce.
What this study adds
-
A population-based sample of adults 50 years and older in Nepal had visual acuity testing and answered a standardized disability questionnaire developed by the United Nations Washington Group on Disability Statistics and recommended by the World Health Organization.
-
Individuals with vision worse than 6/60 in the better-seeing eye were more likely to report disabilities in vision, walking, washing, and communication but not hearing or memory.
-
The questionnaire was easy to implement and may provide information on unintended benefits of public health programs intended to reduce visual impairment.
Data availability
The data that support the findings of this study are available on request from the corresponding author, JMN.
References
World Health Organization. World report on vision. Geneva, Switzerland: World Health Organization; 2019. https://www.who.int/publications-detail/world-report-on-vision.
Global Burden of Disease Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858.
GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2020;9:130–43.
Frick KD, Joy SM, Wilson DA, Naidoo KS, Holden BA. The global burden of potential productivity loss from uncorrected presbyopia. Ophthalmology. 2015;122:1706–10.
Bourne RRA, Flaxman SR, Braithwaite T, Cicinelli MV, Das A, Jonas JB, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e888–e897.
Resnikoff S, Pascolini D, Etya’ale D, Kocur I, Pararajasegaram R, Pokharel GP, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82:844–51.
Flaxman SR, Bourne RRA, Resnikoff S, Ackland P, Braithwaite T, Cicinelli MV, et al. Global causes of blindness and distance vision impairment 1990–2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e1221–e1234.
Hashemi H, Yekta A, Jafarzadehpur E, Doostdar A, Ostadimoghaddam H, Khabazkhoob M. The prevalence of visual impairment and blindness in underserved rural areas: a crucial issue for future. Eye. 2017;31:1221–8.
World Health Organization. World report on disability. Valletta, Malta: World Health Organization; 2011. https://www.who.int/disabilities/world_report/2011/report.pdf.
Whitson HE, Malhotra R, Chan A, Matchar DB, Østbye T. Comorbid visual and cognitive impairment: relationship with disability status and self-rated health among older Singaporeans. Asia Pac J Public Health. 2014;26:310–9.
Rubin GS, Roche KB, Prasada-Rao P, Fried LP. Visual impairment and disability in older adults. Optom Vis Sci. 1994;71:750–60.
West SK, Munoz B, Rubin GS, Schein OD, Bandeen-Roche K, Zeger S, et al. Function and visual impairment in a population-based study of older adults. The SEE project. Salisbury Eye Evaluation. Invest Ophthalmol Vis Sci. 1997;38:72–82.
Ehrlich JR, Stagg BC, Andrews C, Kumagai A, Musch DC. Vision impairment and receipt of eye care among older adults in low- and middle-income countries. JAMA Ophthalmol. 2019;137:146–58.
Tiberti M, Costa V. Disability measurement in household surveys: a guidebook for designing household survey questionnaires. Washington, DC: The World Bank; 2020.
Madans JH, Loeb ME, Altman BM. Measuring disability and monitoring the UN convention on the rights of persons with disabilities: the work of the Washington Group on Disability Statistics. BMC Public Health. 2011;11:S4.
Washington Group on Disability Statistics. The measurement of disability recommendations for the 2010 round of censuses. Washington, DC: Washington Group on Disability Statistics; 2009. http://www.washingtongroup-disability.com/publications/implementing/.
Mont D. Measuring disability prevalence. World Bank Special Protection. 2007;706:1–41.
Lüdecke D, Makowski D, Waggoner P, Patil I. Performance: assessment of regression models performance. R package version 04. Vienna, Austria: 2020;5.
Thapa R, Bajimaya S, Paudyal G, Khanal S, Tan S, Thapa SS, et al. Prevalence and causes of low vision and blindness in an elderly population in Nepal: the Bhaktapur retina study. BMC Ophthalmol. 2018;18:42.
Team R Core. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2013.
Pradhan S, Deshmukh A, Giri Shrestha P, Basnet P, Kandel RP, Lewallen S et al. Prevalence of blindness and cataract surgical coverage in Narayani Zone, Nepal: a rapid assessment of avoidable blindness (RAAB) study. Br J Ophthalmol. 2018;102:291–4.
Sapkota Y, Limburg H. Epidemiology of blindness in Nepal 2012. Kathmandu, Nepal: National Research and Monitoring Department of Nepal Netra Jyoti Sangh and Survey Advisory Committee; 2012.
Globe DR, Varma R, Torres M, Wu J, Klein R, Azen SP, et al. Self-reported comorbidities and visual function in a population-based study: the Los Angeles Latino Eye Study. Arch Ophthalmol. 2005;123:815–21.
Hairi NN, Bulgiba A, Cumming RG, Naganathan V, Mudla I. Prevalence and correlates of physical disability and functional limitation among community dwelling older people in rural Malaysia, a middle income country. BMC Public Health. 2010;10:492.
Rudberg MA, Furner SE, Dunn JE, Cassel CK. The relationship of visual and hearing impairments to disability: an analysis using the longitudinal study of aging. J Gerontol. 1993;48:M261–265.
Swanson MW, McGwin G. Visual impairment and functional status from the 1995 National Health Interview Survey on Disability. Ophthalmic Epidemiol. 2004;11:227–39.
Salive ME, Guralnik J, Glynn RJ, Christen W, Wallace RB, Ostfeld AM. Association of visual impairment with mobility and physical function. J Am Geriatr Soc. 1994;42:287–92.
Groce NE, Mont D. Counting disability: emerging consensus on the Washington Group questionnaire. Lancet Glob Health. 2017;5:e649–e650.
Zheng DD, Swenor BK, Christ SL, West SK, Lam BL, Lee DJ. Longitudinal associations between visual impairment and cognitive functioning: the Salisbury Eye Evaluation Study. JAMA Ophthalmol. 2018;136:989–95.
Lim ZW, Chee ML, Soh ZD, Cheung N, Dai W, Sahil T, et al. Association between visual impairment and decline in cognitive function in a multiethnic asian population. JAMA Netw Open. 2020;3:e203560.
Chen SP, Bhattacharya J, Pershing S. Association of vision loss with cognition in older adults. JAMA Ophthalmol. 2017;135:963–70.
Bernabe-Ortiz A, Diez-Canseco F, Vasquez A, Kuper H, Walsham M, Blanchet K. Inclusion of persons with disabilities in systems of social protection: a population-based survey and case-control study in Peru. BMJ Open. 2016;6:e011300.
Bachani AM, Galiwango E, Kadobera D, Bentley JA, Bishai D, Wegener S, et al. A new screening instrument for disability in low-income and middle-income settings: application at the Iganga-Mayuge Demographic Surveillance System (IM-DSS), Uganda. BMJ Open. 2014;4:e005795.
Hajjioui A, Abda N, Guenouni R, Nejjari C, Fourtassi M. Prevalence of disability in Morocco: results from a large-scale national survey. J Rehabil Med. 2019;51:805–12.
Funding
The study was supported by the National Eye Institute and the Fogarty International Center of the National Institutes of Health (NIH) [Award Number D43TW009343] as well as the University of California Global Health Institute (UCGHI) in the form of a Fogarty grant to JMN and grants from That Man May See, the Fortisure Foundation, the Harper-Inglis Memorial for Eye Research, the Peierls Foundation, the Alta California Eye Research Foundation, the Bofinger Glaucoma Research Fund, and Research to Prevent Blindness. The authors held no agreement with the funders that may have limited their ability to complete the research as planned and have full control of all primary data.
Author information
Authors and Affiliations
Contributions
Concept and design: JDK, KSO, JSM, and VMS. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: JMN and JDK. Critical revision of the manuscript for important intellectual content: All Authors. Administrative, technical, or material support: RPK, RB, BP, HB, SB, KSO, VMS, and JSM. Supervision: JDK.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41433_2021_1498_MOESM3_ESM.eps
Supplemental Figure 2. Association of visual impairment and pinhole visual acuity. Panel A shows the proportion of people in each visual acuity category, with acuity defined as the best pinhole acuity in the better-seeing eye, and with proportions stratified by age group. Panel B shows the number of people in each visual acuity category. Panel C shows the distribution of raw disability scores within each vision group, stratified by type of disability. Panel D shows the results from age- and sex-adjusted logistic regression models in which the presence of disability (defined as “a lot” or “unable to do” in one or more domains) is modeled as a function of a dichotomous pinhole visual acuity exposure variable (able to read the respective line of vision relative to those unable to read the line); dots represent odds ratios and bars represent 95% confidence intervals, and the dashed line represents an odds ratio of 1.
Rights and permissions
About this article
Cite this article
Nesemann, J.M., Kandel, R.P., Byanju, R. et al. Association of visual impairment with disability: a population-based study. Eye 36, 540–546 (2022). https://doi.org/10.1038/s41433-021-01498-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01498-x
This article is cited by
-
Interaction between visual impairment and subjective cognitive complaints on physical activity impairment in U.S. older adults: NHANES 2005–2008
BMC Geriatrics (2024)
-
Associations of walking impairment with visual impairment, depression, and cognitive function in U.S. older adults: NHANES 2013–2014
BMC Geriatrics (2022)
-
Vision-related quality of life amongst patients with low vision and blindness in a resource-limited country
International Ophthalmology (2022)