Abstract
Objective
To define the swept-source optical coherence tomography (SS-OCT) features which distinguish ocular toxoplasmosis (OT) from other forms of retinochoroiditis.
Methods
This is a prospective diagnostic study enrolling 43 eyes of 43 patients with active toxoplasmic (TOXO) retinochoroiditis matched to 54 eyes (54 lesions) with non-TOXO retinochoroiditis evaluated by structural SS-OCT.
Results
The finding of retinal hyper-reflective round deposits, sub-lesional choroidal thickening, and sub-lesional retinal pigment epithelium elevation were more likely to be found in TOXO lesions with a positive likelihood ratio of 45.2 (95% CI: 6.45–316.56), 23.86 (95% CI: 6.09–93.36), and 9.79 (95% CI: 4.22–22.7), respectively. The presence of each of these findings was associated with a high level for positive predictive value (PPV) (88.63–97.29), negative predictive value (NPV) (88.3–92.45), sensitivity (83.72–90.69), and specificity (90.74–98.14). Two-parameter model binary logistic regression suggested that sub-lesional retinal pigment epithelium elevation and sub-lesional choroidal thickening were significant predictors of the diagnosis of OT (Wald = 11.905, p < 0.001; Wald = 14.881, p < 0.001; respectively). By adding hyper-reflective round deposits along the posterior hyaloid or the retinal surface the model improved its performance with very good diagnostic accuracy with area under the curve (AUC) values of 0.96 (95% CI: 0.9–0.99) for two parameters model and 0.98 (95% CI: 0.93–0.99) for the three parameters model.
Conclusions
Our results show that three OCT findings including retinal hyper-reflective round deposits, sub-lesional choroidal thickening, and sub-lesional retinal pigment epithelium elevation are more likely to occur in OT patients as compared with non-OT patients.
Similar content being viewed by others
Introduction
Ocular toxoplasmosis (OT), caused by the protozoan parasite Toxoplasma gondii, is the leading cause of posterior uveitis in the world, accounting for 20–80% of the cases [1]. Retina is the primary site of the infection, but the choroid, vitreous, and anterior chamber are also involved secondarily by inflammation [2].
The diagnosis of OT is primarily clinical, based on the presence of unilateral, unifocal necrotizing retinochoroiditis often associated with a preexistent chorioretinal scar, and variable vitritis [3]. There is, however, a wide spectrum of clinical presentations in OT that may make the distinction with other infectious and noninfectious causes of retinochoroiditis problematic [3,4,5]. Serological tests may support the diagnosis, and analysis of aqueous humor for the presence either of parasitic DNA or of specific antibodies may be useful for the diagnosis of atypical OT [3, 5].
Multimodal imaging, including conventional and new modalities, has been increasingly used in the appraisal and management of OT [6]. Spectral domain-OCT (SD-OCT) and enhanced depth imaging-OCT (EDI-OCT) were found to be useful in delineating vitreal, retinal, and choroidal morphologic changes seen in acute toxoplasmic retinochoroiditis [6,7,8,9]. So far, data on the newly developed swept-source (SS) OCT are scarce, and there have been a very few descriptive studies comparing OCT features of OT with that of other specific conditions [4]. Diagnostic studies based on a sound statistical analysis of the distinguishing OCT features of OT are lacking.
The purpose of this study was to assess the validity of SS-OCT to detect OT among patients with retinochoroiditis or retinitis.
Methods
This is a prospective diagnostic study, carried out at the Department of Ophthalmology, Fattouma Bourguiba University Hospital of Monastir, Tunisia between January 1, 2016 and December 30, 2019.
Pre-test
A pre-test was carried out. Ten training OCT images of patients with toxoplasmic retinochoroiditis and ten OCT images of patients with non-toxoplasmic retinochoroiditis were presented to two independent masked senior ophthalmologists (MM, IK) with 5 and 9 years experience, respectively, who evaluated qualitative changes on structural SS-OCT. In instances of disagreement, there was open adjudication between the two readers until a consensus was established.
Patient enrollment
Sample size (N) calculation was performed considering the cross sectional study’s design and the formula for logistic regression as follows: N = 10k/p, where k is the number of covariates (3 in our study) and p is the smallest proportion of positive cases in the population [10, 11]. The minimum total number of patients needed for this study was ~68.
Were included patients with clinical features of acute OT (TOXO group). The diagnosis of OT in all patients was based on the clinical observation of focal retinochoroidits with or without associated retinochoroidal scar and the presence of positive toxoplasma serology. In doubtful cases, diagnosis was confirmed by aqueous humor analysis with PCR or antibody assessment with the Western blot technique.
The control group comprised patients with acute noninfectious or infectious retinochoroiditis other than toxoplasmosis (non-TOXO group). Each specific entity in the non-TOXO group was diagnosed according to current diagnostic criteria [1].
Exclusion criteria were retinochoroiditis of undetermined etiology, choroiditis with spared retinal layers on OCT, significant media opacities precluding an adequate fundus visualization, trauma, other retinal diseases such diabetic retinopathy, hypertensive retinopathy, central serous chorioretinopathy, macular degeneration, and optic nerve diseases such as glaucoma or optic neuropathy.
All patients underwent complete ophthalmic examination including measurement of Snellen best-corrected visual acuity (BCVA), slit-lamp examination, tonometry, and dilated fundus examination. Only one lesion for one eye was selected for OCT analysis in both groups [12]. In case of multiple lesions, the largest lesion was selected for the analysis.
OCT acquisition and data
SS-OCT images (DRI OCT Triton plus, Topcon, Tokyo, Japan) were obtained the same day as the ophthalmic examination. This system uses a short cavity swept laser with a wavelength of 1050 nm and a speed of 100,000 A-scans per second. All OCT scans were obtained by the same experienced operator. A three-dimensional (3D) 12 × 9-mm scan and/or a 12-mm radial scan made of 12 line scans spread across 360° passing throw the lesions were obtained.
The two independent masked senior ophthalmologists (MM, IK) mentioned above, evaluated all OCT images. The images were randomly presented to the graders.
Qualitative analysis was based on screening for vitreous, retinal, and choroidal changes including vitritis, hyper-reflective oval deposits within the vitreoretinal interface, hyaloid thickening, retinal thickening, hyper-reflectivity of the inner retinal layers, retinal pigmented epithelium (RPE) elevation, subretinal fluid, choroidal hyporeflectivity, and thickening. In instances of disagreement, a third independent assessor (SK) was asked to grade the image. These findings were then compared between the two patient groups.
Quantitative analysis included measurements of retinal and choroidal thickness in the area and adjacent to the active lesion. Retinal thickening was measured as the perpendicular distance from the inner portion of the hyper-reflective line of the lesion to the hyper-reflective line of the RPE. Retinal thickening was defined when retinal thickness exceeded 250 µm. Sub-lesional choroidal thickness was measured beneath the lesion, as the perpendicular distance from the outer portion of the hyper-reflective line of the RPE–Bruch’s membrane interface to the hyper-reflective line of the sclerochoroidal interface using the manual calliper function in the SS-OCT software. Two measurements were obtained from the vertical and horizontal sections under the center of the lesion and were averaged for analysis. The mean value, obtained by the two vertical and horizontal measurements, from the two separate examinators was calculated for the quantitative analysis. Simultaneously, the intraclass correlation coefficient (ICC) was calculated for choroidal thickness measurements. The more ICC is close to 1 the more reproducibility is important [13].
Sub-lesional choroidal thickening was defined when choroidal thickness exceeded 50 µm as compared to the adjacent extra-lesional choroid.
Statistical methods
All statistical analyses were carried out using SPSS 21.0 software. The collected data were coded for analysis. P values of <0.05 were considered significant. Statistical analyses were carried out to compare patients with toxoplasmic retinochoroiditis and patients with other causes of retinitis or retinochoroiditis.
Qualitative changes were compared between the two groups using Chi-square test. The Cohen’s kappa coefficient (interrater reliability) was calculated for all qualitative variables. Values ≤0 indicate no agreement; values between 0.01 and 0.20 none to slight agreement; 0.21–0.40 fair agreement, 0.41–0.60 moderate agreement, 0.61–0.80 substantial agreement, and 0.81–1.00 almost perfect agreement [14].
Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (PLR), diagnostic odds ratio (DOR), and 95% confidence intervals (CI) for each item were calculated for OCT findings and stratified in Toxo group and non-Toxo group. PLR value in the range of <2, 2–5, 5–10, and >10 is recognized as showing a not meaningful, small, moderate, and large increase of probability, respectively. DOR was used as a measure of the effectiveness of a diagnostic test; wherein DOR = 1 means no diagnostic value, DOR > 1 means higher odds of disease, and DOR < 1 means lower odds of disease.
Receiver operating characteristic curves were used to study diagnostic accuracy of the markers in patients with OT, represented by area under the curve (AUC). An AUC in the range of <0.5, ≥0.7–0.8, ≥0.8–0.9, and ≥0.9 defined no discrimination, acceptable discrimination, excellent discrimination, and outstanding discrimination, respectively. A binary logistic regression model was applied using the variables, with the highest AUC scores as explanatory independent variables (i.e., predictors) to classify OT and non-OT cases (i.e., the categorical dependent variables).
The guidelines for accurate logistic regression modeling were followed in this study [15]. Binary logistic regression models were constructed using stepwise analysis to determine which variables were able to differentiate between OT and non-OT retinochoroiditis or retinitis. Different combinations of these parameters were tested to see if the specificity or sensitivity improved.
Results
During the study period a total of 43 eyes of 43 immunocompetent patients were included (TOXO group) and matched to 54 eyes of 54 patients diagnosed with non-toxoplasmic retinochoroiditis (non-TOXO group). The two groups were comparable in terms of gender (Table 1). Mean age in the TOXO group was lower than that in the non-TOXO group.
The non-TOXO group included Behçet’s disease in 18 eyes (33.33%), rickettsial disease in 11 eyes (20.40%), viral acute retinal necrosis and fungal disease in six eyes (11.11%) each, ocular tuberculosis in four eyes (7.40%), sarcoidosis, bartonellosis, ocular toxocariasis, and syphilis in two eyes (5.2%) each, and CMV retinitis in one eye (1.85%).
Unilateral uveitis was more common in the TOXO group than in the non-TOXO group (p = 0.001) (Table 1). Initial BCVA was comparable in both groups, as was the vitreous cells and haze grade (Table 1). The size of selected lesion for the study at presentation was comparable in both groups (Table 1).
Of the TOXO group eyes, 23 (53.5%) had typical active retinochoroiditis associated with chorioretinal scar and 20 eyes (46.5%) had active retinochoroiditis without chorioretinal scar.
SS-OCT findings in the TOXO and non-TOXO groups are detailed in Table 2.
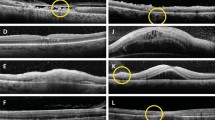
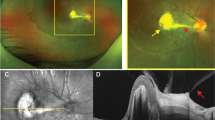
Comparison of the two groups showed that among the OCT findings, hyper-reflective round-shaped deposits along the posterior hyaloid, retinal hyper-reflective round deposits, sub-lesional retinal pigment epithelium elevation, choroidal hyporeflectivity, and sub-lesional choroidal thickening had a significantly higher prevalence in eyes of the TOXO group than in those of the non-TOXO group (p < 0.001 for each) (Figs. 1–3). Inner retinal layers hyper-reflectivity and serous retinal detachment were also more prevalent in the TOXO group (p = 0.04 and 0.036, respectively).
Color fundus photograph (a) of the left eye of a 40-year-old woman shows a yellow-white active toxoplasmic retinochoroiditis associated with periarterial plaques inferonasally. A corresponding linear SS-OCT scan (b) shows a partially detached thickened posterior hyaloid (arrowhead), hyper-reflectivity and thickening of the inner retinal layers (arrows), retinal architecture disorganization, hyper-reflective round-shaped deposits along the posterior hyaloid and the retinal surface (pink dots), sub-lesional retinal pigment epithelium elevation (yellow line), and sub-lesional choroidal thickening and hyporeflectivity delineated by the cyan line.
Color fundus photograph (a) of the right eye of a 31-year-old woman demonstrates a large yellow-white retinochoroidal lesion in the posterior pole adjacent to the superotemporal retinal vascular arcade. A corresponding linear SS-OCT (b) shows posterior hyaloid thickening, hyper-reflective vitreous dots, hyper-reflective round-shaped deposits along the retinal surface (arrows), focal hyper-reflective retinal thickening, retinal architecture disorganization, sub-lesional retinal pigment epithelium elevation (arrowheads), sub-lesional choroidal thickening and hyporeflectivity (asteriks), and serous retinal detachment (stars). Color fundus photograph (c) of the left eye of a 30-year-old woman shows a yellow-white active retinochoroidal lesion in the posterior pole, inferonasal to the macula. A linear SS-OCT scan passing through the lesion (d) shows hyper-reflective round-shaped deposits along the posterior hyaloid (arrow), focal hyper-reflective thickening of the retina predominantly involving the inner layers, retinal architecture disorganization, sub-lesional retinal pigment epithelium elevation (triangle), and sub-lesional choroidal thickening and hyporeflectivity (asteriks). A macular OCT scan (e) demonstrates hyper-reflective round-shaped deposits along the posterior hyaloid (arrows), and a shallow serous retinal detachment. Color fundus photograph (f) of the left eye of a 35-year-old woman shows a large yellow-white active superomacular retinochoroidal lesion adjacent to an old scar. A linear SS-OCT scan (g) shows posterior hyaloid thickening, hyper-reflective thickening of the retina predominantly involving the inner layers, retinal architecture disorganization, a splitting of retinal pigment epithelium-Bruch’s complex (arrows), and a sub-lesional choroidal thickening and hyporeflectivity.
Color fundus photograph (a) of a left eye of a 16-year-old female with Behçet’s disease shows a superomacular white retinal lesion. A corresponding linear SS-OCT scan (b) shows vitreous linear hyper-reflectivity at the edge of the lesion with punctate vitreous dots, focal hyper-reflective retinal thickening causing posterior shadowing, and retinal architecture disorganization. Color fundus photograph (c) of a 28-year-old man with rickettsial disease shows a white retinal lesion along the superior vascular arcade. Corresponding linear SS-OCT (d) demonstrates hyper-reflective vitreous dots, focal hyper-reflective thickening of the inner retinal layers causing posterior shadowing, and retinal architecture disorganization. Color fundus photograph (e) of the left eye of a 35-year-old woman with indolent granular CMV retinitis. A corresponding linear SS-OCT (f) shows hyper-reflectivity involving all retinal layers and retinal architecture disorganization. Color fundus photograph (g) of the right eye of a 56-year-old woman with endogenous candida endophthalmitis presenting with multiple white retinal lesions. SS-OCT through the largest lesion (arrow) (h) shows a partially detached posterior hyaloid with an adjacent preretinal vitreous condensation (arrowhead), focal hyper-reflective thickening of the inner retinal layers causing posterior shadowing, and retinal architecture disorganization. It is noteworthy that SS-OCT shows no sub-lesional retinal pigment epithelium elevation or sub-lesional choroidal thickening in any of these patients with non-toxoplasmic retinitis.
Cohen’s kappa coefficient calculated for the qualitative variables in both groups showed substantial agreement to almost perfect agreement for all SS-OCT findings (extremes: 0.78 and 0.98).
Quantitative choroidal assessment showed a sub-lesional choroidal thicknes of 610.17 µm (±250.84) in the TOXO group and 351.18 µm (±170.89) in the non-TOXO group (p = 10−3).
We identified seven variables that provided high DOR (higher than 5) which included hyper-reflective round-shaped deposits along the posterior hyaloid, retinal hyper-reflective round deposits, inner retinal layers hyper-reflectivity, retinal thickening, splitting of the retinal pigment epithelium-Bruch’s complex, sub-lesional retinal pigment epithelium elevation, and sub-lesional choroidal thickening (Table 2).
Three major OCT findings were identified to be more likely to occur in OT patients compared with non-TOXO patients. They included retinal hyper-reflective round deposits, sub-lesional retinal pigment epithelium elevation, and sub-lesional choroidal thickening, with a PLR of 45.2, 23.86, and 9.79, respectively. The presence of each of these findings was associated with a high level for PPV (88.63–97.29), NPV (88.3–92.45), sensitivity (83.72–90.69), and specificity (90.74–98.14) (Table 2).
Cohen’s kappa coefficient shows almost perfect agreement for retinal hyper-reflective round deposits and sub-lesional retinal pigment epithelium elevation: 0.84 and 0.98, respectively. The intraclass correlation coefficient for choroidal thickness measurements was 0.84.
A separate comparison between the TOXO group and each etiology in non-TOXO group was performed. According to the AUC values, excellent discrimination and outstanding discrimination were obtained for five items in the majority of sub-groups (Supplementary Table 1).
In all sub-groups, the highest curves were noted for hyper-reflective round-shaped deposits along the posterior hyaloid and sub-lesional choroidal thickening.
The selection of predictors for the binary logistic regression analysis was based on the AUC analysis results. Using a two-parameter model binary logistic regression suggested that sub-lesional retinal pigment epithelium elevation and sub-lesional choroidal thickening were significant predictors of the diagnosis of OT (Wald = 11.905, p < 0.001; Wald = 14.881, p < 0.001; respectively). By adding hyper-reflective round-shaped deposits along the posterior hyaloid or the retinal surface the model improved its performance with very good diagnostic accuracy, with AUC values of 0.96 (95% CI: 0.9–0.99) for two-parameter model and 0.98 (95% CI: 0.93–0.99) for the three-parameter model (Supplementary Table 2).
Discussion
SD-OCT and, more recently SS-OCT, are widely used in the diagnosis and management of toxoplasmic retinochoroiditis. SS-OCT provides several advantages over SD-OCT including improved penetration through opacities, faster acquisition times, and a greater depth and field [7]. It can visualize the vitreous, retinal, and choroidal changes in a single scan, compared with the different imaging algorithms required with SD-OCT [7]. SS-OCT effectively increases the accuracy of choroidal and RPE analyses, highly hampered by the shadowing induced by the active retinitis above.
Our SS-OCT study, consistent with previous SD-OCT studies, shows that an array of structural changes can occur in patients with active OT. These include posterior hyaloid thickening and detachment, vitreous hyper-reflective dots, increased reflectivity in the inner retina with disorganization of retinal structure, posterior shadowing, RPE elevation, and choroidal thickening with hyporeflectivity beneath the active lesion.
Although, the number of each etiology in the non-TOXO group was small, the wide majority of SS-OCT findings cited above maintained excellent to outstanding discrimination value for the diagnosis of toxoplasmic retinochoroiditis compared to specific non-toxoplasmosis retinitis or retinochoroiditis.
Almost all previous OCT studies in OT were retrospective and non-comparative studies, and therefore do no not provide statistical evidence on the diagnostic value for any specific OCT finding. In a recent retrospective descriptive study by Invernizzi et al., SD-OCT was useful in differentiating OT from viral retinitis [4]. Hyper-reflective round deposits in the posterior hyaloid and the retinal surface were more frequent in OT than in viral herpetic retinitis, and choroidal changes including choroidal architecture disruption and thickening were found to be significantly more frequent in OT [4].
To the best our knowledge, the current study is the first prospective, diagnostic study to define the OCT features, which distinguish OT in immunocompetent patients from non-toxoplasmic aetiologies of retinochoroiditis. The control (non-TOXO) group was broadened to include a variety of infectious and noninfectious uveitic entities that may clinically mimic OT. Patients were stratified based on whether they were diagnosed with OT or non-OT for thorough statistical analysis with PPV, NPV, AUC, PLR, and DOR of the various documented SS-OCT findings.
Our results show that three OCT findings including retinal hyper-reflective round deposits, sub-lesional retinal pigment epithelium elevation, and sub-lesional choroidal thickening are more likely to occur in OT patients compared with non-OT patients.
In addition to previously described OCT findings, a splitting of the retinal pigment epithelium-Bruch’s complex offers a specificity and a PPV of 100%. This finding was scarcely reported in the literature and may be explained by a necrotic process in the edge of RPE as the parasite progresses from the retina to the choroid [16].
Our study has some limitations. The sample size of the non-toxoplasmic group was relatively small, and the inclusion of a wide variety of entities in this group did not allow separate analysis of all OCT findings for each specific etiology. The study also did not include immunocompromised patients in toxoplasmosis group who may have different OCT changes.
In conclusion, this prospective study provides information regarding SS-OCT findings of active toxoplasmic retinochoroiditis as compared to non-toxoplasmic retinochoroiditis, and reveals several of these features as distinctive for ocular toxoplasmosis. SS-OCT, as well as SD-OCT with EDI mode, is extremely useful in the diagnosis of acute toxoplasmic retinochoroiditis, particularly in the absence of associated old scar.
Supplementary material is available on Eye’s website.
Summary
What was known before
-
SD-OCT and EDI-OCT were found to be useful in delineating vitreal, retinal, and choroidal morphologic changes seen in acute toxoplasmic retinochoroiditis.
What this study adds
-
The current diagnostic study defines the OCT features, which distinguish OT in immunocompetent patients from non-toxoplasmic aetiologies of retinochoroiditis.
Change history
23 July 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41433-021-01692-x
References
Tsirouki T, Dastiridou A, Symeonidis C, Tounakaki O, Brazitikou I, Kalogeropoulos C, et al. A focus on the epidemiology of uveitis. Ocul Immunol Inflamm. 2018;26:2–16.
Kijlstra A, Petersen E. Epidemiology, pathophysiology, and the future of ocular toxoplasmosis. Ocul Immunol Inflamm. 2014;22:138–47.
Garweg JG. Ocular toxoplasmosis: an update. Klin Monbl Augenheilkd. 2016;233:534–9.
Invernizzi A, Agarwal AK, Ravera V, Mapelli C, Riva A, Staurenghi G, et al. Comparing optical coherence tomography findings in different aetiologies of infectious necrotising retinitis. Br J Ophthalmol. 2018;102:433–7.
Cunningham ET, Belfort R, Muccioli C, Arevalo JF, Zierhut M. Ocular toxoplasmosis. Ocul Immunol Inflamm. 2015;23:191–3.
Brandão-de-Resende C, Balasundaram MB, Narain S, Mahendradas P, Vasconcelos-Santos DV. Multimodal imaging in ocular toxoplasmosis. Ocul Immunol Inflamm. 2020;28(8):1196–1204.
Chen KC, Jung JJ, Engelbert M. Single acquisition of the vitreous, retina and choroid with swept-source optical coherence tomography in acute toxoplasmosis. Retin Cases Brief Rep. 2016;10:217–20.
Goldenberg D, Goldstein M, Loewenstein A, Habot-Wilner Z. Vitreal, retinal, and choroidal findings in active and scarred toxoplasmosis lesions: a prospective study by spectral-domain optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2013;251:2037–45.
Oréfice JL, Costa RA, Scott IU, Calucci D, Oréfice F, Grupo Mineiro de Pesquisa em Doenças Oculares Inflamatórias (MINAS). Spectral optical coherence tomography findings in patients with ocular toxoplasmosis and active satellite lesions (MINAS Report 1). Acta Ophthalmol. 2013;91:e41–7.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–9.
Wang X, Ji X. Sample size estimation in clinical research: from Randomized Controlled Trials to observational studies. Chest. 2020;158:S12–20.
Karakosta A, Vassilaki M, Plainis S, Elfadl NH, Tsilimbaris M, Moschandreas J. Choice of analytic approach for eye-specific outcomes: one eye or two? Am J Ophthalmol. 2012;153:571–9.e1.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med. 2012;22:276–82.
Stoltzfus JC. Logistic regression: a brief primer. Acad Emerg Med. 2011;18:1099–104.
Vasconcelos-Santos DV, Campos WR, Oréfice F. Necrotic retinal pigment epithelium in toxoplasmic retinochoroiditis. Acta Ophthalmol. 2010;88:e92.
Acknowledgements
Ministry of Higher Education and Research of Tunisia.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study concept and design, and all authors acquired and interpreted study data. IK, MM, and HBA collected data. MBF and MM performed statistical analyses. IK and SK drafted the manuscript. NA, SK, and MK provided critical manuscript revisions and supervised the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
The study protocol followed the Tenets of the Declaration of Helsinki and was approved by the local institutional review board. Informed consent was obtained for all participants prior to their inclusion in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Due to a processing error the spelling of given name by Manel Ben Fredj.
Supplementary information
Rights and permissions
About this article
Cite this article
Ksiaa, I., Khochtali, S., Mefteh, M. et al. Distinguishing swept-source optical coherence tomography findings in active toxoplasmic retinochoroiditis. Eye 36, 1222–1230 (2022). https://doi.org/10.1038/s41433-021-01491-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01491-4
This article is cited by
-
Clinical Features and Possible Origin of Preretinal Deposits in Different Ocular Diseases and Events: A Narrative Review
Ophthalmology and Therapy (2023)