Abstract
Introduction
Retinopathy of prematurity (RoP) is a vasoproliferative disorder caused by the abnormal development of retinal vessels in premature neonates. It is one of the major causes of childhood blindness, which is increasing with the increasing survival rate of low birth weight and premature neonates. This study has aimed to evaluate the role of oxidative stress and peroxidant antioxidant balance (PAB) in the pathogenesis and prediction of RoP.
Materials and methods
A total of 154 neonates weighing <1500 g admitted at the NICU of Ghaem Hospital, Mashhad, Iran, were enrolled in this cross-sectional study between 2018 and 2020. Blood samples were collected on the first day of birth to assess the peroxidant and antioxidant balance. The demographic, prenatal, and clinical course and postnatal problems were also recorded. The neonates were examined for RoP and divided into control (healthy) and affected (ROP) groups.
Results
There were significant differences between the two groups in gestational age, duration of oxygen therapy, and first and fifth minute Apgar score (P < 0.005). The mean PAB in infants without and with ROP was 19.79 HK (Hamidi–Koliakos) and 38.45 HK, respectively (P < 0.0001). Also, the mean PAB in neonates with ROP grade 1 and 2 was 36.69 HK and 45.53 HK, respectively (P = 0.002).
Conclusion
According to our findings, the PAB level can be helpful in predicting ROP incidence. With increasing PAB, the possibility of ROP severity will increase.
Similar content being viewed by others
Introduction
Prematurity is one of the major health-threatening problems in neonates [1]. Premature birth is the most important cause of neonatal morbidity and mortality. Premature neonates have various problems in function, maturation, and development of different organs, most notably complete lack of lung maturation, brain, eye, kidney, gastrointestinal, and immune systems; requiring intensive care [1, 2].
Retinopathy of prematurity (RoP), which is characterized by abnormal vascular growth of retinal vessels in preterm neonates, is one of the most common and important problems in preterm neonates. The most important predisposing factors of RoP are prematurity, low birth weight, and oxygen uptake [3, 4]. Other possible predisposing factors include apnea, mechanical ventilation, anemia and need for blood transfusion, vitamin deficiency, intraventricular hemorrhage, sepsis, acidosis, hypotension, Pneumothorax, chronic lung disease, high level of arterial carbon dioxide, environment light, seizures, and bradycardia have been associated with an increased incidence of RoP [4,5,6]. The role of free oxygen radicals and oxidative stress in the pathogenesis of ROP vascular changes has already been discussed. Oxidative stress is the imbalance between oxidants (free radicals) and antioxidants, which results in a redox state of the body and redox reactions. This disorder results from an increase in free radicals and an imbalance between the production and elimination of active species in the body and a decrease in the potency of the antioxidant system. Neonates have lower levels of antioxidants (beta-carotene, ceruloplasmin, transferrin, melatonin, and erythrocyte superoxidase) [6]. The antioxidant system of neonates, especially premature neonates, cannot eliminate the pro-oxidants well, which is involved in the pathophysiology and complications of many neonatal diseases including respiratory distress syndrome (RDS), asphyxia, bronchopulmonary dysplasia (BPD), intraventricular hemorrhage (IVH), patent ductus arteriosus (PDA), and necrotizing enterocolitis (NEC) [7, 8]. Premature neonates are more susceptible to oxidative stress by transferring from the hypoxic intrauterine to a normal euoxic environment and the need for extra oxygen, whereas preterm neonates have a lower level of antioxidants such as vitamins A and E, superoxide dismutase (SOD), catalase, and glutathione peroxidase (GPX) as the first-line defense to free radicals [9]. While suffering from complications of prematurity, these neonates are more susceptible to toxic oxygen damage when receiving supplemental oxygen to overcome respiratory failure due to the difficulties in autoregulation of retinal blood flow [10]. Kumar et al. showed that low birth weight neonates have lower levels of antioxidants. Also, diseases such as inflammation and perinatal asphyxia are more common in these infants because of the deficiency of major antioxidant enzymes such as SOD (that converts superoxide to GPX and H2O2) and catalase (that converts H2O2 to molecular oxygen and water), resulting in the body defense against free radical attacks [9]. To evaluate the balance, both oxidant and antioxidant levels status are required. Therefore, several methods have been proposed for the separate measurement of the oxidant and antioxidant status. These methods are laborious, time-consuming, expensive, and inaccurate. However, many of these methods only examine one side of the oxidative stress balance. There is no theoretical agreement to measure oxidative stress. Hence, the estimation of oxidant–antioxidant balance is indirect. A simple, fast, and inexpensive method for measuring the balance between oxidants and antioxidants is used simultaneously using tetramethylbenzidine (TMB). This cation provides redox status as peroxidant antioxidant balance. The diagnostic value of this marker has already been studied and proved in various studies [10]. Therefore, one of the major problems of preterm neonates that affect their future life is RoP. This case–control study has aimed to evaluate PAB in VLBW neonates with and without ROP.
Material and method
This cross-sectional study was carried out on low birth weight neonates (<1500 g) in the NICU of Ghaem hospital in Mashhad from January 2018 to April 2020. The research project was approved by Mashhad University of Medical Sciences (IR.MUMS.fm.REC.1394.258 code 940147). Informed consent was obtained from the parents prior to enrollment in the study. The exclusion criteria were: neonates with congenital anomaly and infection. A 0.2 cc of serum was isolated from the first blood sample collected from the neonate and sent to the laboratory for PAB measurement through TMB staining (3.3–3.5-tetramethylbenzidine) and oxidation of the stained cations [10]. The TMB–TMB cation can be used as a redox index according to its electrochemical and optical properties. This method is the first that can measure the balance of oxidants and antioxidants simultaneously in one experiment by using two different kinds of reactions; one enzymatic reaction where the chromogen TMB is oxidized to a color cation by peroxides; and a chemical reaction where the TMB cation is reduced to a colorless compound by antioxidants. The photometric absorbance is then compared with the absorbances given by a series of standard solutions that are made by mixing varying proportions (0–100%) of hydrogen peroxide with uric acid [10]. The results are expressed as the percentage of hydrogen peroxide in the calibration mixture and the PAB value shows the oxidative stress index and defined as an arbitrary unit (HK unit, Daryoush Hamidi Alamdari = H, George Koliakos = K).
Neonatal demographic information was recorded in a checklist. Complete neonatal characteristics (birth weight, age, sex, gestational age, Apgar score, and clinical symptoms), maternal history (age, pregnancy, and delivery problems, and type of delivery), and laboratory results were recorded in a questionnaire, then the statuses of the neonates were recorded until discharge. The neonates were examined and evaluated for RoP by an ophthalmologist at 32 weeks or four weeks after birth. The control group consisted of preterm neonates with no RoP. The classification of the stages and severity of RoP disease was defined based on the international classification to explain posterior and anterior extension. The eye was divided into three zones: zone I was the most posterior and zone III was the most anterior. Zone I: a circle whose center corresponds to the disc and its radius is twice the distance of the disk to the macula. Zone II: begins at the end of zone I and continues to the Ora serrate on the nasal side and almost to the equator on the temporal side. Zone III: the remainder of the retina that encompasses the upper and lower temporal regions and is anterior to zone II [11]. The severity of RoP was defined in five stages as the disease serially passed through these stages. However, stages 1 and 4 can occur simultaneously in one eye. Stage 1: demarcation line stage 2: the presence of ridge with or without small fibers of fibrovascular proliferation. Stage 3: ridge with extraretinal fibrovascular proliferation. Stage 4: subtotal retinal detachment. A: without fovea involvement. B: with fovea involvement. Stage 5: complete retinal detachment type 1 threshold disease is defined as stage 3 RoP in zone I or zone II at least five consecutive hours or a total of eight non-consecutive hours with plus disease. Plus disease is seen as dilatation and tortoise of posterior pole artery. Plus disease is an indicator of the severity of the disease and is defined as venous dilatation and arterial tortoise of posterior pole artery [11]. SPSS software version 22 was used for data analysis. A chi-square test was used to investigate the relationship between the qualitative variables. Odds ratios were also calculated and reported as necessary. A covariance test was used to control for confounding variables. Non-parametric Mann–Whitney test was used for comparing the mean of the abnormal distribution. A P-value < 0.05 was considered statistically significant.
Results
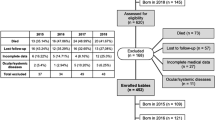
Out of 187 neonates, 13 died, 10 neonates had a definitive infection, two neonates had a congenital anomaly, two neonates had a congenital infection, and six neonates did not come back for an eye examination. A total of 88 neonates (56.3%) had RoP and 69 (43.3%) were normal. A total of 53 neonates had RoP grade I; 32 neonates had RoP grade II, and four neonates had RoP grade III. Fifty-one percent of neonates were male and 49% were female; 76% of girls had RoP but 32% of boys had RoP (OR = 6.85, P = 0.004). There was no relationship between the type of delivery and incidence of RoP (P = 0.395). Gestational age, 1 and 5 min Apgar scores, and the duration of oxygen therapy were significantly different between the two groups (P < 0.005). The mean PAB levels in infants with and without RoP were 38.45 HK and 19.79 HK, respectively (P < 0.0001) (Table 1).
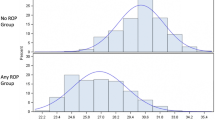
The mean PAB increased with increasing the severity of RoP, with a mean PAB of 19.8 HK in normal infants, 36.7 HK in infants with RoP grade I, and 45.5 HK in infants with RoP grade II of (P = 0.002, Shapiro–Wilk) (Fig. 1).
Despite controlling for confounding factors of gestational age, Apgar score of 1 and 5 min, and duration of oxygen therapy, The difference in PAB between the two groups was still significant (P = 0.007). Ninety-five percent of neonates with RoP recovered during follow-up, but two neonates with stage III involvement were treated with intravitreal bevacizumab (anti-VEGF) and two had laser treatment, both of which were found in subsequent retinal vascularization.
Discussion
According to the results of our study, PAB level was twice in neonates who later developed RoP in comparison to non-RoP neonates. The PAB level increased with increasing the severity of RoP in mild to moderate cases, despite elimination of confounding factors of gestational age, oxygen therapy duration, and Apgar score. Oxidative stress has a role in the pathogenesis of many neonatal diseases including BPD, RDS, IVH, NEC, and asphyxia [8, 12]. Garg et al. [13] showed that MDA oxidants were significantly higher in infants who developed RoP later. RoP occurs during two phases of pathological changes. The first phase begins with the pause in retinal vascular growth after the preterm birth. As the preterm infant is exposed to high oxygen concentrations, a partial hyperoxic condition occurs that results in a decrease in vascular endothelial growth factor (VEGF) and subsequently regression of the evolved retinal vessels. In the second phase of RoP, a relative hypoxic state develops after the oxygen is discontinued and its pressure is normalized. In addition, the metabolic requirement of the non-vascular tissue of the retina is now increasing as the neonates grow. Therefore, an increase in oxygen demand causes ischemic damage to the retina. This relative hypoxic state in the retina results in abnormal vascular proliferation and neovascularization. During the two phases of RoP, the retina is exposed to fluctuations in oxygen pressure, which increases with retinal hypoxia and result in the production of reactive oxygen species (RoS) [14]. Retinal development in preterm neonatal animal species is particularly susceptible to damage by RoS. Oxygen oscillations stimulate the expression of NADPH oxidase, which increases RoS and endothelial cell apoptosis, leading to the formation of the avascular retina. Repeated fluctuations in oxygen also increase endothelial growth factor (VEGF) and RoS. VEGF bioactivity is reduced by neovascularization and torsion. RoS inhibition through NADPH inhibitor of aposinine oxidase decreases avascular retina by interfering apoptosis [15].
More than half of the babies we examined had ROP. Inappropriate and poor control administration of hyperbaric oxygen in the delivery room may be the reason for the high prevalence of ROP in our center.
In our study, gestational age and birth weight of neonates with RoP were lower than those without RoP. Several studies have suggested that these two are the major risk factors for RoP [3, 4, 15, 16]. RoP has three major risk factors including gestational age, low birth weight, and external oxygen therapy, which means that incomplete retinal vascular growth in premature infants can predispose RoP. In our study, girls were six times more likely to develop RoP. But, in most epidemiological studies, there is no difference between the sexes in developing RoP. One study showed more RoP in boys [3].
In the present study, the duration of oxygen therapy in neonates with RoP was twice that of non-RoP neonates. Several studies have confirmed the association between the duration of oxygen therapy and the possibility of increased incidence of RoP [3, 4, 15, 16]. Due to extreme overcare, oxygen administration, mechanical ventilation, surfactant administration, and parenteral nutrition preterm infants are particularly exposed to free radicals during the first week of life. This prolongs the oxidative stress through increased oxygen delivery to the tissues [17].
The death of neonates and failure to attend eye examination was one of the limitations of our study.
Conclusion
According to our results, gestational age, 1 and 5 min Apgar score, duration of oxygen therapy, and sex are the risk factors for RoP. For the first time and with a different method, we showed that increased PAB level at birth can be a risk factor for RoP in the future.
Summary
What was known before
-
Retinopathy of prematurity (RoP) is a vasoproliferative disorder caused by the abnormal development of retinal vessels in premature neonates.
-
It is one of the major causes of childhood blindness, which is increasing with the increasing survival rate of low birth weight and premature neonates.
What this study adds
-
PAB level can be helpful in predicting ROP incidence.
-
With increasing PAB, the possibility of ROP severity will increase.
References
Boskabadi H, Omidian M, Mafinejad S. Neonatal Complications Related with Prolonged Rupture of Membranes Macedonian. J Med Sci. 2011;4:93–8.
Bakhshaee M, Boskabadi H, Hassanzadeh M, Nourizadeh N, Ghassemi MM, Khazaeni K, et al. Hearing impairment in the neonate of preeclamptic women. Otolaryngol Head Neck Surg. 2008;139:846–9.
Saeidi R, Taraghi B, Saeidi M. Incidence of retinopathy of prematurity (ROP) in low birth wight newborns. Iran J Neonatol. 2017;8:102–6.
Abrishami M, Maemori G, Boskabadi H, Yaeghobi Z, Mafi-Nejad S, Abrishami M. Incidence and risk factors of retinopathy of prematurity in mashhad, northeast. Iran Red Crescent Med J. 2013;15:229–33.
Li SY, Fu ZJ, Lo ACY. Hypoxia-induced oxidative stress in ischemic retinopathy. Oxid Med Cell Long. 2012;2012:26769.
Panfoli I, Candiano G, Malova M, De Angelis L, Cardiello V, Buonocore G, et al. Oxidative stress as a primary risk factor for brain damage in preterm newborns. Front Pediatr. 2018;6:369.
Boskabadi H, Maamori G, Ghayour-mobarhan M, Bagheri F. Kalateh mollaei M. Comparison of the predictive value of prooxidant-antioxidant balance and heat shock proteins in the diagnosis of neonatal asphyxia. Biomed Res Ther. 2017;4:1327–40.
Boskabadi H, Zakerihamidi M, Heidarzadeh M, Avan A, Ghayour-Mobarhan M, Ferns G. The value of serum pro-oxidant/antioxidant balance in the assessment of asphyxia. J Matern Fetal Neonatal Med. 2017;30:1556–61.
Kumar A, Ranjan R, Basu S, Khanna H, Bhargava V. Antioxidant levels in cord blood of low birth weight newborns. Indian Pediatr. 2008;45:583.
Alamdari DH, Paletas K, Pegiou T, Sarigianni M, Befani C, Koliakos G. A novel assay for the evaluation of the prooxidant–antioxidant balance, before and after antioxidant vitamin administration in type II diabetes patients. Clin Biochem. 2007;40:248–54.
Kanski JJ, Bowling B. Clinical ophthalmology: a systematic approach. Edinburgh: Elsevier Health Sciences; 2011.
Boskabadi H, Navaee Boroujeni A, Mostafavi-Toroghi H, Hosseini G, Ghayour-Mobarhan M, Hamidi Alamdari D, et al. Prooxidant-antioxidant balance in perinatal asphyxia. Indian J Pediatr. 2014;81:248–53.
Garg U, Jain A, Singla P, Beri S, Garg R, Saili A. Free radical status in retinopathy of prematurity. Indian J Clin Biochem. 2012;27:196–9.
Lee JW, Davis JM. Future applications of antioxidants in premature infants. Curr Opin Pediatr. 2011;23:161–6.
Azami M, Jaafari Z, Rahmati S, Farahani AD, Badfar G. Prevalence and risk factors of retinopathy of prematurity in Iran: a systematic review and meta-analysis. BMC Ophthalmol. 2018;18:83.
Bayat-Mokhtari M, Pishva N, Attarzadeh A, Hosseini H, Pourarian S. Incidence and risk factors of retinopathy of prematurity among preterm infants in Shiraz/Iran. Iran J Pediatr. 2010;20:303.
Buonocore G, Perrone S, Longini M, Vezzosi P, Marzocchi B, Paffetti P, et al. Oxidative stress in preterm neonates at birth and on the seventh day of life. Pediatr Res. 2002;52:46.
Author information
Authors and Affiliations
Contributions
HB, MM, GM, MaA, MoA, and MZ conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted. NS, MSS, MGM, SRHS, and ST designed the study and carried out the initial analyses, reviewed and revised the manuscript, and approved the final manuscript as submitted. FS, MK, AM, and MZ carried out the initial analyses, reviewed and revised the manuscript, and approved the final manuscript as submitted. MZ and HB designed the data collection instruments and coordinated and supervised data collection at two of the four sites, critically reviewed the manuscript, and approved the final manuscript as submitted. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Boskabadi, H., Marefat, M., Maamouri, G. et al. Evaluation of pro-oxidant antioxidant balance in retinopathy of prematurity. Eye 36, 148–152 (2022). https://doi.org/10.1038/s41433-021-01465-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01465-6
This article is cited by
-
Comparison of Retinopathy of Prematurity Incidence in Preterm Infants of Mothers with Preeclampsia and Infants of Healthy Mothers
The Journal of Obstetrics and Gynecology of India (2022)