Abstract
Objectives
To evaluate whether intravitreal injections (IVI) of anti-vascular endothelial growth factor (anti-VEGF) in neovascular age-related macular degeneration (nAMD) patients with prior stroke or acute myocardial infarction (AMI) are associated with increased mortality.
Methods
From 2005 to 2013, nAMD patients in the Taiwan National Health Insurance Research Database who received IVI of anti-VEGF and had a diagnosis of stroke/AMI prior to their first injections were defined as the IVI group. The mortality of the IVI group during the study period was compared to that of the non-IVI group, which consisted of nAMD patients who had prior stroke/AMI but were never exposed to anti-VEGF. The IVI group and the non-IVI group were 1–4 matched according to propensity score (PS), which was derived from age, sex, date of stroke/AMI and comorbidities. PS-adjusted Cox regression analyses were used to estimate the hazard ratio (HR) for mortality associated with IVI of anti-VEGF. Subgroup analyses were also performed according to the interval between stroke/AMI and IVI (≤6 months, 6 months to 1 year, 1–2 years, >2 years).
Results
There were 3384 individuals in the IVI group and 13,536 individuals in the non-IVI group. The IVI group had a significantly higher mortality risk (adjusted HR = 2.37; 95% confidence interval (CI), 2.14–2.62) than the non-IVI group. Subgroup analyses revealed that elevated mortality was significant when anti-VEGF was injected within 1 year after stroke/AMI.
Conclusions
We found an increased mortality risk associated with IVI of anti-VEGF in nAMD patients with prior stroke/AMI compared to the mortality risk of nAMD patients with prior stroke/AMD but without exposure to anti-VEGF.
Similar content being viewed by others
Introduction
Neovascular age-related macular degeneration (nAMD) is characterized by abnormal choroidal vessels growing into the sub-retinal pigment epithelial or sub-retinal space, leading to exudate and haemorrhage that impair vision. Since vascular endothelial growth factor (VEGF) stimulates the process of neovascularization, intravitreal injections (IVI) of anti-VEGF could inhibit the formation of neovessels in the eye and slow exudation and haemorrhage in the macula. Currently, the most commonly used anti-VEGF agents are bevacizumab, ranibizumab and aflibercept. For nAMD, IVI of anti-VEGF protect 90–95% of patients from a clinically significant decrease in visual acuity, and 33–40% of patients even perceive a clinically significant improvement [1, 2].
Although VEGF plays a key role in the pathogenesis of nAMD, it is essential in the restoration of the damaged vascular endothelium [3]. By blocking VEGF, arterial thromboembolic events (ATEs) such as stroke and acute myocardial infarction (AMI) may occur, leading to increased mortality [4,5,6,7,8,9]. Previous studies have revealed an increased risk of ATEs in patients receiving systemic (intravenous) bevacizumab treatment for malignant carcinoma [4,5,6,7]. IVI of anti-VEGF, at a much lower dose than systemic injection, has been found to increase the incidence of ATEs [8] and mortality [9] in some studies. However, more randomized control trials, observational studies, and meta-analyses revealed no significantly increased risk for severe systemic adverse events or mortality among patients receiving IVI of anti-VEGF [10,11,12,13,14,15]. The inconsistent results may be due to discrepancies in study design, inclusion/exclusion criteria and confounders. In addition, most of these studies included only those who had no stroke/AMI prior to IVI; thus, we could not determine the systemic safety of intravitreal anti-VEGF among those who had previous stroke/AMI. Since patients suffering from stroke/AMI have a damaged or vulnerable vascular system [3], angiogenesis has even more important role in tissue remodelling. Anti-VEGF, blocking the angiogenesis in these patients, might induce a deleterious outcome. To the best of our knowledge, only two population-based studies in Israel focused on the patients with previous stroke/AMI and found higher mortality risks after IVI of anti-VEGF [16, 17].
Therefore, in our study, we aimed to investigate mortality after IVI of anti-VEGF among nAMD patients with a past history of stroke/AMI. By comparing these patients with nAMD patients who also had prior stroke/AMI but never received IVI of anti-VEGF, we could determine whether IVI of anti-VEGF would significantly increase the risk of mortality in nAMD patients with prior stroke/AMI.
Materials and methods
Data source
Our study was approved by the ethics committee of Yang-Ming University Hospital (2015A018). The population-based study retrieved medical records since 1996 from the Taiwan National Health Insurance Database (NHIRD), which includes heath care information for all 23 million residents in Taiwan. The database was collected by the National Health Insurance Administration and was released for the purpose of research. All the data were de-identified and scrambled; therefore, the requirement for informed consent was waived by the regulation of the Institutional Review Board.
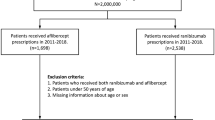
Inclusion and exclusion criteria
The study period was from January 1, 2005 to December 31, 2013. We identified patients treated with IVI of anti-VEGF for nAMD during the study period. They had to have stroke/AMI before IVI. Those treated with IVI of anti-VEGF from 1996 to the end of 2004 were excluded to ensure that patients enroled had their first injection during the study period. The date of the first injection of each patient during the study period was defined as the index date (the date of enrolment). These patients were classified into the IVI group. To ensure these patients received IVI of anti-VEGF because of nAMD, they should have nAMD as the principal diagnosis (the first diagnosis in the columns of diagnoses) on the date of IVI. This is because of the regulation of our National Health Insurance Administration that the indication of procedure/operation is presented as the principal diagnosis in the claimed data.
Then, we used the propensity score (PS) matching method to enrol controls from the population of patients who had a history of stroke/AMI and never received IVI of anti-VEGF. Four controls were matched to each patient in the IVI group according to PS and the date of stroke/AMI. In addition, the index date (date of enrolment) of each control was matched to the index date of the corresponding patient in the IVI group. The controls were classified into the non-IVI group. PS was computed from age, sex and comorbidities such as diabetes mellitus, hypertension, hyperlipidaemia, congestive heart failure, renal failure, obesity and smoking (or chronic obstructive pulmonary disease (COPD)). Because these factors were reported to have an impact on both AMD and mortality, they had to be adjusted as confounders. We merged patients with COPD with those had smoking on purpose of multivariate cox regression analysis. If the IVI group and the non-IVI group were well-matched according to the PS, these confounders would be well-controlled and balanced between the two groups.
Statistical analysis
The IVI group and the non-IVI group composed the study cohort. The patients were followed from the index date to the death date or to the end of 2013, whichever came first. First, the characteristics of the two groups were presented according to age, sex, diabetes mellitus, hypertension, hyperlipidaemia, congestive heart failure, renal failure, obesity, smoking, PS and follow-up time. For continuous variables, the mean and standard deviation were calculated, and group differences were analysed using the two-sample t-test. For categorical variables, frequencies and percentages in the two groups were compared using the chi-square test. The cumulative incidences of mortality during the follow-up period were also assessed and compared between the two groups.
Second, the incidence density of mortality was calculated separately in the two groups. The hazard ratio (HR) for mortality was then derived from Cox regression analysis after adjustment for PS. Subsequently, the interval between the date of stroke/AMI and the index date was calculated and was categorized into four levels (≤6 months, 6–12 months, 1–2 years and >2 years). Each person in our study cohort was classified into subgroups 1–4 according to the categorized interval levels (subgroup 1: ≤6 months; subgroup 2: 6–12 months; subgroup 3: 1–2 years; subgroup 4: >2 years). Subgroup analyses were performed to derive the HR for mortality corresponding to each interval.
Third, we performed two sensitivity analyses. In sensitivity analysis 1, patients with diabetes were excluded. Then the incidence density of mortality in the IVI group and the PS-matched non-IVI group was calculated. Cox regression analysis was used to derive the HR for mortality after adjustment of PS. In sensitivity analysis 2, the non-IVI group was matched to the IVI group on age, sex and index date, but not on the comorbidities. We derived the differences in comorbidities between the two groups. Multivariate Cox regression was applied to calculate the risk for mortality according to IVI of anti-VEGF after adjustment of age, sex and comorbidities. A p value < 0.05 was considered to be statistically significant. All statistical operations were performed using SAS statistical package, version 9.2 (SAS Institute, Cary, NC, USA).
Results
Demographic and clinical characteristics of the study sample
A total of 16,920 subjects were included in the study. Among the study cohort, 3384 received IVI of anti-VEGF (the IVI group), and 13536 PS-matched controls did not receive anti-VEGF (the non-IVI group). Table 1 shows the demographic and clinical characteristics of the two groups. Since the two groups were well-matched according to the PS, they were similar in age, sex and comorbidities. The mean age was 69.9 years. Males constituted 31.2% of the study cohort. High prevalence of some comorbidities was found in both groups. Nearly 36% had diabetes mellitus, 81% had hypertension and 56% had hyperlipidaemia. Those who smoked accounted for almost 45% of the study cohort. The proportion of anti-platelet and anti-coagulation drugs use was similar in the two groups (88.6% in the IVI group vs. 89.1% in the non-IVI group; p = 0.36). During the follow-up period, the cumulative incidence of mortality was significantly higher in the IVI group (16.8%) than in the non-IVI group (8.0%).
Mortality risk
Table 2 displays the incidence density of mortality with regard to the IVI group and non-IVI group. Their mortality rates were 732.73 and 309.24 per 10,000 years, respectively. The Cox regression after adjusting for PS yielded a significantly higher hazard of mortality for the injection group (HR = 2.36, with a 95% confidence interval (CI) 2.13–2.61).
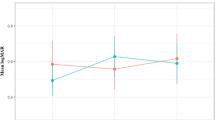
Subgroup analysis
Figure 1 shows the HRs for mortality of IVI compared to non-IVI, calculated separately according to categorized interval levels (subgroup 1: ≤6 months; subgroup 2: 6–12 months; subgroup 3: 1–2 years; subgroup 4: >2 years). In subgroup 1 and subgroup 2, those receiving IVI of anti-VEGF had a significantly higher risk of mortality with adjusted HRs of 4.84 (95% CI, 3.99–5.90) and 3.55 (95% CI, 2.67–4.68), respectively. However, if anti-VEGF was injected more than 1 year after stroke/AMI, it did not have a significant impact on mortality. The HRs for mortality in subgroup 3 and subgroup 4 were 1.34 (95% CI, 0.97–1.83) and 1.06 (95% CI, 0.86–1.29), respectively.
Sensitivity analyses
In sensitivity analysis 1, only patients without diabetes were included. Table 3 shows the incidence density of mortality in the IVI group and the non-IVI group (689.83/10,000 years vs. 308.69/10,000 years, respectively). The HR derived from Cox regression was 2.24 (95% CI, 1.96–2.54).
In sensitivity analysis 2, characteristics of the IVI group and the age- and sex-matched non-IVI group were compared. Supplementary Table 1 displays the differences in the prevalence of comorbidities between the two groups. Age- and sex-matched non-IVI group had significantly higher proportions of diabetes, congestive heart failure and smoking than the IVI group. However, renal failure was significantly more prevalent in the IVI group. The use of anti-platelet and anti-coagulation drugs was 88.6% in the IVI group and 89.2% in the age- and sex-matched non-IVI group (p = 0.31). During the follow-up period, the mortality rate was 16.8% in the IVI group, which was significantly higher than the 5.9% in the non-IVI group. Table 4 shows the HRs for mortality according to each covariates in the multivariate Cox regression. Age, male gender, diabetes, hypertension, hyperlipidaemia, congestive heart failure, renal failure, obesity and smoking significantly increased the mortality risk; so did the IVI of anti-VEGF (HR = 2.22; 95% CI, 1.89–2.59).
Discussion
This study reveals that among the nAMD patients with prior stroke/AMI, those who received IVI of anti-VEGF have a significantly higher mortality rate than those without any anti-VEGF injections (adjusted HR = 2.37; 95% CI, 2.14–2.62). The risk of mortality is more prominent if anti-VEGF is injected within 1 year after stroke/AMI.
IVI of anti-VEGF have become the first-line treatment for most cases of nAMD. A Cochrane systemic review published in 2019 showed the effectiveness of this therapy to maintain visual acuity [18]. However, several studies have assessed anti-VEGF agent in plasma and reported a reduced VEGF level in serum following IVI of anti-VEGF [19,20,21,22,23,24]. Therefore, concern of anti-VEGF over systemic adverse effects is necessary. Fortunately, in the MARINA and PIER randomized controlled trials, the incidence of stroke, myocardial infarction and mortality was not found to be elevated significantly following IVI of anti-VEGF for nAMD [1, 25]. Similarly, studies based on population health databases in the USA and Singapore revealed no statistically significant changes in all-cause mortality following IVI of anti-VEGF among nAMD patients [26, 27]. It is noteworthy that these studies excluded patients with prior stroke/AMI, who are more prevalent among the nAMD group and have a greater predisposition to mortality. Exclusion of these high-risk patients might decrease the mortality rate, thus making the difference in mortality between the IVI and non-IVI groups non-significant. Therefore, if we want to evaluate the impact of IVI of anti-VEGF on mortality among nAMD patients in the real world, it is appropriate to include those with prior stroke/AMI.
Hanhart et al. in 2017, based on the Israel Clalit Health database, evaluated the mortality rate of nAMD patients. Among them, 5385 received IVI of anti-VEGF (IVI group), and 10756 were age- and sex-matched controls (non-IVI group) [28]. In contrast to previous studies, Hanhart did not exclude patients with previous stroke/AMI. During the 6-year study period, 19.7% in the IVI group died, which was significantly higher than the 12.1% mortality rate in the non-IVI group (p value < 0.0001). After adjusting for confounders, the IVI group still had a significantly higher mortality rate (HR = 1.69; 95% CI, 1.54–1.84). Moreover, the same research team published another two papers focusing on nAMD patients with prior stroke and prior AMI, respectively [16, 17]. Compared with the age- and sex-matched controls (non-IVI group), those with IVI of anti-VEGF had a significantly higher risk of mortality (adjusted HR = 1.44 and 1.71, respectively). The findings that IVI of anti-VEGF increases the risk of mortality among nAMD patients with prior stroke/AMI are compatible with the findings of our study.
One of the strengths of our study is that we included nAMD patients with prior attacks of either stroke or AMI. Stroke and AMI are both critical vascular diseases leading to high risks of mortality. It is reasonable to postulate that the systemic effects of intravitreal anti-VEGF might further hinder the recovery of vascular damage and thus increase mortality. In addition, stroke and AMI have similar underlying risk factors and would be better considered as a whole. Therefore, our study focused on nAMD patients with prior stroke or AMI.
Another strength of our study is that we tried our best to reduce the confounding effects. In our study design, both the IVI group and non-IVI group had a diagnosis of nAMD and a past history of stroke/AMI at baseline. In addition, the non-IVI group was 1:4 PS-matched with the IVI group. In other words, the two groups were well-matched for age, sex and comorbidities, not only for age and sex. With the comprehensiveness of our NHIRD, these variables were available and accessible. This would decrease the confounding effects and increase the comparability between the two groups. The Cox regression adjusted for PS could also reduce the confounding effects.
Another strength of our study is that mortality was computed for different intervals between stroke/AMI and IVI. Our study revealed a higher risk of mortality when the interval was shorter. We also found that if the interval is more than 1 year, a significant increase in mortality does not exist. Our findings are compatible with those of a previous study conducted by Hanhart et al. [16]. Thus, IVI of anti-VEGF might be safer if it is performed more than 1 year after stroke/AMI than within 1 year. The significantly higher mortality when anti-VEGF was injected within 1 year after stroke/AMI may be due to the susceptibility to systemic adverse events in this stage. Patients with recently occurring stroke/AMI have worse vascular stability and a more fragile systemic status. Therefore, they are more susceptible to the harmful effects of anti-VEGF. On the other hand, a longer period after stroke/AMI leads to vessels and the whole body being healthier than when they were in the acute crisis stage; thus, they are stronger to survive even though anti-VEGF induces some side effects.
Our study has some limitations. First, some variables, such as visual acuity and dietary habits, are not recorded in our NHIRD. This may result in residual confounding. More prospective clinical studies are necessary to solve this problem. Second, we assessed all-cause mortality as an outcome, not cause-specific mortality. The reason is that some deaths are difficult to classify as being from a specific cause in our database. For example, when a patient with both neoplasm and cerebrovascular accident died, we cannot differentiate the direct cause of death from our database. Therefore, we adopted all-cause mortality to avoid misclassification. Further large epidemiologic studies will be conducted to differentiate the impact of anti-VEGF on cause-specific mortality. Third, we retrieved patients receiving anti-VEGF injections through the procedure codes, but we could not differentiate what kind of anti-VEGF the patients received. These are the inherent drawbacks of our database. Further clinical studies are necessary in order to include this information.
In the sensitivity analysis 1, we focused on the population without diabetes because we wanted to derive the impact of anti-VEGF on patients with nAMD. Patients with diabetes may also receive IVI of anti-VEGF due to diabetic retinopathy, thus they were excluded in order to make sure those receiving IVI of anti-VEGF were under the indication of nAMD. The significantly higher risk of mortality after IVI of anti-VEGF in nAMD patients without diabetes convinces us that it is a true phenomenon.
In the sensitivity analysis 2, we used age- and sex-matched controls instead of PS-matched controls as the non-IVI group; thus, the impact of comorbidities as well as IVI of anti-VEGF on the mortality risk could be computed in the multivariate Cox regression. The result that IVI of anti-VEGF remained a significant risk factor of mortality implies the association actually exists.
Due to the retrospective study design, we cannot conclude the causal relationship between IVI of anti-VEGF and increased mortality. However, we can still evaluate the possible association. Our study reminds ophthalmologists that if a nAMD patient has prior stroke/AMI requiring IVI of anti-VEGF, we have to confirm that the systemic conditions of the patient are being treated appropriately by physicians. Ophthalmologists should also be very cautious when performing IVI of anti-VEGF in these high-risk patients.
Conclusions
Currently, IVI of anti-VEGF has become the mainstay of treatment for nAMD. Our study, based on 9 years of NHIRD, revealed that treatment may be associated with an increased risk of mortality (adjusted HR = 2.37; 95% CI, 2.14–2.62) among nAMD patients with prior stroke/AMI. Therefore, ophthalmologists should carefully weigh the benefits and harms of anti-VEGF and emphasize the need for surveillance for systemic adverse effects.
Summary
What was known before
-
In the MARINA and PIER randomized controlled trials, the mortality was not found to be elevated significantly following IVI of anti-VEGF for nAMD.
-
Studies based on population health databases in the USA and Singapore revealed no statistically significant changes in all-cause mortality following IVI of anti-VEGF among nAMD patients.
-
However, previous studies excluded patients with previous stroke or AMI. Therefore, we could not determine the systemic safety of intravitreal anti-VEGF among those who had previous stroke/AMI.
What this study adds
-
We included nAMD patients with prior attacks of either stroke or AMI. We found that those who received IVI of anti-VEGF have a significantly higher mortality rate than those without any anti-VEGF injections.
-
In our statistical analyses, we used the propensity matching method and Cox regression to reduce the confounding effects.
-
We further found that the risk of mortality is more prominent if anti-VEGF is injected within 1 year after stroke/AMI.
Data availability
Data are available from the National Health Insurance Research Database (NHIRD) published by Taiwan National Health Insurance (NHI) Bureau. The data utilized in this study cannot be made available in the manuscript, the supplemental files, or in a public repository due to the ‘Personal Information Protection Act’ executed by Taiwan’s government, starting from 2012. Requests for data can be sent as a formal proposal to the NHIRD (http://nhird.nhri.org.tw) or by email to wt.gro.irhn@drihn.
References
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355:1419–31.
Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim RY, et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med. 2006;355:1432–44.
Hutter R, Carrick Fe Fau - Valdiviezo C, Valdiviezo C, Fau - Wolinsky C, Wolinsky C, Fau - Rudge JS, et al. Vascular endothelial growth factor regulates reendothelialization and neointima formation in a mouse model of arterial injury. Circulation. 2004;110:2430–5.
Schutz FA, Je Y, Azzi GR, Nguyen PL, Choueiri TK. Bevacizumab increases the risk of arterial ischemia: a large study in cancer patients with a focus on different subgroup outcomes. Ann Oncol. 2011;22:1404–12.
Zuo PY, Chen XL, Liu YW, Xiao CL, Liu CY. Increased risk of cerebrovascular events in patients with cancer treated with bevacizumab: a meta-analysis. PLoS ONE. 2014;9:e102484.
Chen XL, Lei YH, Liu CF, Yang QF, Zuo PY, Liu CY, et al. Angiogenesis inhibitor bevacizumab increases the risk of ischemic heart disease associated with chemotherapy: a meta-analysis. PLoS ONE. 2013;8:e66721.
Ranpura V, Hapani S, Chuang J, Wu S. Risk of cardiac ischemia and arterial thromboembolic events with the angiogenesis inhibitor bevacizumab in cancer patients: a meta-analysis of randomized controlled trials. Acta Oncol. 2010;49:287–97.
Schlenker MB, Thiruchelvam D, Redelmeier DA. Intravitreal anti-vascular endothelial growth factor treatment and the risk of thromboembolism. Am J Ophthalmol. 2015;160:569–80.e5.
Avery RL, Gordon GM. Systemic safety of prolonged monthly anti-vascular endothelial growth factor therapy for diabetic macular edema: a systematic review and meta-analysis. JAMA Ophthalmol. 2016;134:21–9.
Boyer DS, Heier JS, Brown DM, Francom SF, Ianchulev T, Rubio RG. A Phase IIIb study to evaluate the safety of ranibizumab in subjects with neovascular age-related macular degeneration. Ophthalmology. 2009;116:1731–9.
Campbell RJ, Gill SS, Bronskill SE, Paterson JM, Whitehead M, Bell CM. Adverse events with intravitreal injection of vascular endothelial growth factor inhibitors: nested case-control study. BMJ. 2012;345:e4203.
Sangroongruangsri S, Chaikledkaew U. Real-world safety of intravitreal bevacizumab and ranibizumab treatments for retinal diseases in Thailand: a prospective observational study. Clin Drug Investig. 2018;38:853–65.
Fung AE, Rosenfeld PJ, Reichel E. The international intravitreal bevacizumab safety survey: using the internet to assess drug safety worldwide. Br J Ophthalmol. 2006;90:1344–9.
Curtis LH, Hammill BG, Schulman KA, Cousins SW. Risks of mortality, myocardial infarction, bleeding, and stroke associated with therapies for age-related macular degeneration. Arch Ophthalmol. 2010;128:1273–9.
Poku E, Rathbone J, Wong R, Everson-Hock E, Essat M, Pandor A, et al. The safety of intravitreal bevacizumab monotherapy in adult ophthalmic conditions: systematic review. BMJ Open. 2014;4:e005244.
Hanhart J, Comaneshter DS, Vinker S. Mortality after a cerebrovascular event in age-related macular degeneration patients treated with bevacizumab ocular injections. Acta Ophthalmol. 2018;96:e732–9.
Hanhart J, Comaneshter DS, Freier-Dror Y, Vinker S. Mortality associated with bevacizumab intravitreal injections in age-related macular degeneration patients after acute myocardial infarct: a retrospective population-based survival analysis. Graefes Arch Clin Exp Ophthalmol. 2018;256:651–63.
Solomon SD, Lindsley K, Vedula SS, Krzystolik MG, Hawkins BS. Anti-vascular endothelial growth factor for neovascular age-related macular degeneration. Cochrane Database Syst Rev. 2019;3:Cd005139.
Drolet DW, Nelson J, Tucker CE, Zack PM, Nixon K, Bolin R, et al. Pharmacokinetics and safety of an anti-vascular endothelial growth factor aptamer (NX1838) following injection into the vitreous humor of rhesus monkeys. Pharm Res. 2000;17:1503–10.
Gaudreault J, Fei D, Rusit J, Suboc P, Shiu V. Preclinical pharmacokinetics of Ranibizumab (rhuFabV2) after a single intravitreal administration. Invest Ophthalmol Vis Sci. 2005;46:726–33.
Avery RL, Castellarin AA, Steinle NC, Dhoot DS, Pieramici DJ, See R, et al. Systemic pharmacokinetics following intravitreal injections of ranibizumab, bevacizumab or aflibercept in patients with neovascular AMD. Br J Ophthalmol. 2014;98:1636–41.
Wang X, Sawada T, Sawada O, Saishin Y, Liu P, Ohji M. Serum and plasma vascular endothelial growth factor concentrations before and after intravitreal injection of aflibercept or ranibizumab for age-related macular degeneration. Am J Ophthalmol. 2014;158:738–44.e1.
Zehetner C, Kralinger MT, Modi YS, Waltl I, Ulmer H, Kirchmair R, et al. Systemic levels of vascular endothelial growth factor before and after intravitreal injection of aflibercept or ranibizumab in patients with age-related macular degeneration: a randomised, prospective trial. Acta Ophthalmol. 2015;93:e154–9.
Yoshida I, Shiba T, Taniguchi H, Takahashi M, Murano T, Hiruta N, et al. Evaluation of plasma vascular endothelial growth factor levels after intravitreal injection of ranibizumab and aflibercept for exudative age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2014;252:1483–9.
Abraham P, Yue H, Wilson L. Randomized, double-masked, sham-controlled trial of ranibizumab for neovascular age-related macular degeneration: PIER study year 2. Am J Ophthalmol. 2010;150:315–24.e1.
Dalvin LA, Starr MR, AbouChehade JE, Damento GM, Garcia M, Shah SM, et al. Association of intravitreal anti-vascular endothelial growth factor therapy with risk of stroke, myocardial infarction, and death in patients with exudative age-related macular degeneration. JAMA Ophthalmol. 2019;137:483–90.
Ng WY, Tan GS, Ong PG, Cheng CY, Cheung CY, Wong DW, et al. Incidence of myocardial infarction, stroke, and death in patients with age-related macular degeneration treated with intravitreal anti-vascular endothelial growth factor therapy. Am J Ophthalmol. 2015;159:557–64.e1.
Hanhart J, Comaneshter DS, Freier Dror Y, Vinker S. Mortality in patients treated with intravitreal bevacizumab for age-related macular degeneration. BMC Ophthalmol. 2017;17:189.
Funding
This work was supported by the Taichung Veterans General Hospital (Grant number TCVGH-1106901B).
Author information
Authors and Affiliations
Contributions
Y-YC, Y-JL and Y-FY were involved in research design. Y-YC, Y-FY and PC were responsible for data collection. Y-YC, Y-JL and PC were involved in analysis and interpretation. Y-YC was responsible for manuscript preparation.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the ethical committee of National Yang-Ming University Hospital (2015A018).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Chen, YY., Lai, YJ., Yen, YF. et al. Increased mortality after intravitreal injections of anti-VEGF for neovascular AMD among patients with prior stroke or acute myocardial infarction. Eye 36, 153–159 (2022). https://doi.org/10.1038/s41433-021-01416-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01416-1
This article is cited by
-
Systemic adverse events and all-cause mortality following same-session bilateral intravitreal anti-VEGF injections: a systematic review
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Risk analysis for patients with arterial thromboembolic events after intravitreal ranibizumab or aflibercept injections
Scientific Reports (2023)