Abstract
Background/aims
Health-related quality of life (HRQoL) in age-related macular degeneration (AMD) is difficult to estimate as most generic tools underestimate vision. Our aim was to measure the effect of AMD on generic and visual quality of life and how it relates to handicap. We also aimed to validate the NG82 NICE AMD classification. Finally, we studied if a bolt-on visual domain increased the EQ-5D sensitivity to AMD.
Patients and methods
Ninety-six patients with AMD participated in this observational cross-sectional study. Visual (VF-14) and generic questionnaires (EQ-5D) with VIS, and the London handicap scale (LHS) was used to quantify HRQoL and handicap. ANOVA and regression analysis were used to identify significant associations.
Results
Visual dysfunction in AMD has a significant effect in VF-14 (P < 0.001), LHS (p < 0.001), and EQ-5D (p = 0.015). The EQ-5D was less sensitive than the VF-14 and LHS and was not significantly correlated with the VIS bolt-on domain (p = 0.608). On the other hand, VIS was significantly associated with visual acuity (p < 0.001), AMD diagnosis (p = 0.005), VF-14 (p < 0.001), and LHS (p < 0.001). The new AMD classification was a good predictor of visual HRQoL and had an excellent association with visual acuity in the best eye.
Conclusion
This article shows that visual impairment is associated with lower HRQoL and with an increased handicap. It also suggests that a visual dimension may increase the EQ-5D sensitivity in AMD. There was a relationship between visual impairment and handicap with the items of the new NICE AMD classification, which supports its use.
Similar content being viewed by others
Introduction
Age-related macular degeneration (AMD) is a condition characterized by loss of central vision. This leads to visual disability and has a negative effect on health-related quality of life (HRQoL) [1], which is defined as the individual’s subjective perception of the value of their state of health [2].
Impairment, or loss of function, causes disability, which is an inability to perform tasks. The reduced ability to undertake activities in relation to their peers has been termed by the World Health Organization as a handicap [3]. In AMD, the impairment is a loss of visual acuity, which is measured by the inability to identify letters on a chart. This leads to a handicap, which in AMD, for example, is not being able to read a price label. Adaptations of visual disability help to mitigate handicap—audible books and magnifying glasses are classic examples of such adaptations.
Visual impairment in AMD is best measured by visual acuity. However, HRQoL and its associated disability in vision are difficult to measure [4, 5] and there is no gold standard tool [6]. The National Institute for Clinical Excellence (NICE) has a preference for the Euroqol 5 dimension questionnaire (EQ-5D), which is a generic tool able to generate utility values and support the calculation of quality-adjusted life-years (QALYs) [7,8,9]. However, there is a considerable body of literature that suggests that the EQ-5D is not sensitive to identify changes of HRQoL in most visual disorders, including AMD [5, 6, 8, 10]. The lack of sensitivity of the EQ-5D to visual problems led to the development of the bolt-on vision dimension to the standard EQ-5D, the EQ-5D-VIS [11], which has been shown to be more sensitive to visual disorders [12]. The visual function index 14 (VF-14) is a questionnaire that has been created to measure the visual quality of life in patients undergoing cataract surgery and has since been validated for AMD [9]. Visual HRQoL tools provide a good indication of the patient’s visual quality of life but they do not measure the generic quality of life. The London handicap scale (LHS) is a validated tool that measures the patient’s handicap [3].
NICE has produced guidelines on the management of AMD, and introduced a new classification for AMD, with the aim to improve communication with patients [13]. A useful classification describes distinct states, which should imply a specific cause, prognosis, and/or an appropriate course of action. In previous classifications, the term dry AMD can refer to three distinct scenarios. It can refer to early AMD where the patient has drusen, good vision, and does not require routine hospital review. It can also be applied to geographic atrophy where the patient has advanced visual loss and needs low vision aid (LVA) and is eligible for a certificate of vision impairment (CVI). It could also mean that they have inactive wet AMD and do not require further treatment. This recent classification divides AMD into early and late, and visual acuity is one of the parameters in the diagnosis. Within late AMD, it can be subdivided into wet active, wet inactive, or dry. Indeterminate is a diagnostic category for a minority of cases that do not fall under any of those categories. Each diagnostic category is associated with a prognosis and a suggested treatment [13].
In this study, we aimed to:
-
Assess if the NG 82 AMD classification predicts HRQoL (visual and generic) and handicap.
-
Investigate if LVA clinics or demographic factors help to mitigate HRQoL and handicap.
-
Quantify if a bolt-on visual domain added to the EQ-5D is associated with standard EQ-5D values and if it correlates with visual acuity, visual quality of life, and handicap.
Methods
We have undertaken an observational cross-sectional study of patients attending the macular clinic of the Queen’s Medical Center, Nottingham University Hospitals, UK. It was approved by the London—Chelsea research ethics committee. Ninety-six patients were recruited who met the inclusion criteria of having an active diagnosis of AMD, ability to speak English, and capacity to consent. Exclusion criteria included other ocular conditions including moderate or advanced glaucoma, considerable cataract, uveitis, amblyopia, corneal pathology affecting visual acuity, vitreous hemorrhage, optic neuropathy, and moderate or severe diabetic retinopathy. All patients signed a consent form before the questionnaire was started.
Data collected
Clinical information gathered included AMD subtype, previous treatment (laser or injections), previous attendance to the LVA clinic, and presence of other disabilities. Their demographic data included age, gender, and educational attainment (pre-general certificate of secondary education (GCSE)-equivalent and GCSE equivalent and further education).
AMD classification was according to the classification introduced in the NICE guidelines [13]. Visual acuities were made using the early treatment diabetic retinopathy study (ETDRS) protocol as LogMar (Precision Vision, Villa Park, IL) for right, left, and both eyes. All patients had a thorough examination to exclude other causes for visual loss.
We used the generic EQ-5D-3L with a vision-specific dimension [11, 12] and the vision-specific VF-14 to measure their visual quality of life. Briefly, this consists of the normal three-tier EQ-5D with an additional dimension which rates vision in three states, 1—no difficulties, 2—moderate difficulties, 3—extreme difficulties. We used the LHS to measure handicap [3]. We had permission from the EuroQoL group to use the EQ-5D and from Rowan Harwood for the use of the LHS.
Statistical analysis
Subjects were divided into diagnostic groups, and differences in demographic variables across the groups were tested. Pearson chi-square tests were used to study associations between each pair of diagnostic groups and categoric variables including gender (male and female), employment status (working, unemployed/disabled, and retired), and educational attainment. Because this study is an observational exploratory study with no single primary outcome measure, we did not perform a power calculation. We collected a reasonable sample size and use our confidence intervals as the measure of uncertainty.
Descriptive analysis was used to categorize variables. T-tests were performed to assess differences between patient groups on the continuous variables, age, and visual acuity. Statistical significance was first checked by correlation. To test the association of a dependent variable with a categorical factor with more than two choices we used analysis of variance (ANOVA) or linear regression.
Linear regressions were performed with dependent variables being the HRQoL test values at the different time points and independent variables including the demographic and clinical variables. Two regression analysis methods were used. We first analyzed in univariate analysis, which meant that we analyzed individually all the clinical and demographic factors as independent variables against the quality of life tools as dependent variables. At this point, we eliminated any independent variables that had p value over 0.05. We then used a backward method, in which all previously tested independent variables were included and then removed if p > 0.05 until we had only significant variables. We then did a stepwise regression. This was made by comparison of models, in which the most significant independent variable (as per R2 score) was placed on top and successively less significant placed below until significance was lost. The R2 scores identify the weight of a significant independent variable within a dependent variable with 1.0 being equivalent to 100%.
Other factors listed as independent variables included the VIS dimension domain and driving (yes/no). The output of linear regression was made by listing the beta coefficient estimate, R2, and p value for statistical significance, where applicable. Ordinal regression analysis was made to study the correlation of visual acuity and AMD diagnosis with the VIS domain, which was divided into 1, 2, and 3, according to the responses given in the questionnaire. When using categorical values for linear regression we performed an ad hoc ANOVA to confirm significance.
All regressions were checked for autocorrelation using the Durbin–Watson test and the result not considered if the p-value of this analysis was below 0.05. All ANOVA analyses were checked for autocorrelation with Levene’s test and not considered if the p-value was below 0.05. Statistics were performed with Jamovi (version 1.1.9.0).
Results
Ninety-six patients were recruited and no patients withdrew from the study. Table 1 shows a summary of the population characteristics.
Visual acuity in the better eye (BEVA) was associated with binocular visual acuity
Mean visual acuity in the BEVA was 0.36 ± 0.32 and was strongly correlated to visual acuity with both eyes (p < 0.001), which was 0.34 ± 0.32 (Table 1). Mean visual acuity in the worst eye (WEVA) was not associated with binocular visual acuity.
New NICE AMD classification is associated with visual acuity in the better of the two eyes
AMD classification is strongly associated with age-adjusted BEVA (p < 0.001), which is expected as the classification of AMD is partly based on the patient’s visual acuity. AMD classification is associated with differences in visual acuity between early and late AMD (Table 1). However, there were no differences between normal and early AMD eyes or between different categories of late AMD (Table 1). WEVA diagnosis is significantly associated with age-adjusted WEVA visual acuity (WEVA; p < 0.001).
Linear regression analysis with post hoc ANOVA suggested that AMD classification in the best eye was a good predictor of VF-14 but not EQ-5D and LHS (Table 2). AMD classification in the WEVA did not predict any of the HRQoL tools (Table 2). Finally, AMD classification could significantly predict the bolt-on visual dimension in the EQ-5D-VIS (p = 0.005).
Visual acuity is the best predictor of quality of life scores and of the bolt-on VIS dimension
Age-adjusted BEVA was a significant positive predictor of visual QoL (VF-14), generic QoL (EQ-5D), and handicap (LHS) and this is shown in Table 2. BEVA was also a very good predictor of the EQ-5D-VIS bolt-on visual dimension (p < 0.001).
Age was also significantly and negatively associated with VF-14 and LHS but not EQ-5D (Table 2).
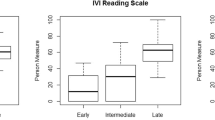
Vision is under-represented in EQ-5D and bolt-on VIS dimension is highly correlated with vision-related QoL
We have shown that the vision bolt-on dimension on its own is strongly associated with AMD classification and visual acuity in AMD. We correlated the EQ-5D-VIS bolt-on dimension with quality of life tools. Figure 1 shows VF-14 (Fig. 1A) and EQ-5D (Fig. 1B) plotted against responses to VIS. Further analysis with ANOVA suggested that the relationship of VF-14 and VIS dimension was highly significant (p < 0.001) with a η2 of 0.52. This significance was much less pronounced between the VIS and EQ-5D (p = 0.013) with a η2 of 0.089.
Box plots showing the spread of (A) VF-14, (B) EQ-5D, and (C) LHS values according to visual bolt-on dimension. 1: means no difficulties, 2: moderate difficulties, and 3: extreme difficulties. The bottom, middle and top lines in each box indicate the first quartile, median and third quartile, respectively. The bottom and top whiskers indicate the minimum and maximum value, respectively. Cross indicates mean.
We sought to correlate the six dimensions of the EQ-5D-VIS with the VF-14 in order to find the VIS dimension correlated with the final VF-14 score. Multivariate linear regression of VF-14 values with the six dimensions as independent variables suggested that vision (p < 0.001) and mobility (p = 0.012) are the only dimensions that can act as predictors of the VF-14 questionnaire, accounting for 55% (R2 = 0.55) of the VF-14 score (Table 3). This suggests that vision and mobility are the most important factors in vision-related HRQoL.
We also analyzed the response distribution of the EQ-5D-VIS six dimensions (Table 1). In our cohort of patients with AMD, the vision dimension has a disproportional number of “extreme” answers. However, the remaining five dimensions are shifted towards “no difficulties”. We did a regression analysis of the EQ-5D utility values against the six dimensions of the EQ-5D-VIS. This revealed that the VIS dimension is not significantly associated with the EQ-5D utility value (p = 0.608), suggesting that vision is not taken sufficiently into account in the EQ-5D utility score.
Vision is an important factor in the LHS and VIS dimension has a significant relationship with the handicap
The spread of LHS scores against those of the visual bolt-on domain of the EQ-5D-VIS dimension is shown in Fig. 1C. ANOVA showed a significant statistical relationship (p < 0.001) with a η2 of 0.26.
We analyzed the relative significance of the six dimensions of the EQ-5D as predictors for the LHS. According to this, VIS (p < 0.001) and pain (p < 0.001) are the only significant predictors and most important components of the score with a relative weight of 44% (R2 = 0.44) towards the total score when analyzed together (Table 3).
We tested if educational attainment or LVA clinic attendance were mitigating factors for decreased handicap as a result of visual impairment. There was no association of LVA attendance or educational attainment with the levels of handicap (Table 2).
Quality of life in AMD is affected by driving, and AMD is an important factor for the quality of life in patients who had to stop driving
Driving is an important part of everyday life in adults with visual disorders [14]. In this study, all patients who stopped driving for visual reasons did so because of AMD. Patients who were able to drive had statistically higher scores of visual and generic quality of life. These patients were also associated with higher LHS value scores (indicating lower handicap).
We compared patients who stopped driving due to AMD and patients who stopped driving for other reasons. This analysis showed that those with AMD had lower age-adjusted VF-14 scores (p < 0.001), indicating that visual disability and consequent inability to drive caused by AMD is a significant factor in the patient’s visual quality of life (Fig. 2A). Consistent with this, LHS scores were lower in patients who stopped driving due to AMD, indicating that these patients have a higher handicap than patients who stopped driving for other reasons (Fig. 2C). There was no significant difference when comparing these two groups against the EQ-5D (Fig. 2B; p = 0.213).
Discussion
In this study, we have shown that visual disability caused by AMD has a significant effect on the patient’s visual quality of life and handicap. We could not demonstrate that either LVA clinic attendance or educational attainment were effective as mitigating factors. Our results using the VF-14 and LHS and comparing them to EQ-5D support the suggestions in the literature that the EQ-5D lacks sensitivity to pick up the quality of life changes that are significant in AMD [5, 6, 8, 9]. The EQ-5D-VIS was sensitive to visual loss in AMD and correlated well with the visual quality of life. Lastly, we have shown that the new NICE AMD classification is closely associated with visual acuity and that it may help in communicating prognosis and treatment options to AMD patients.
This study is based on the framework that visual impairment causes disability and that this results in an individual being unable to perform tasks that would be normal and expected—the patient’s handicap.
The results here show that poor vision in AMD is associated with lower LHS scores (which indicate higher handicap). Furthermore, AMD patients who stopped driving because of vision had lower LHS scores than patients who stopped driving for other reasons. This is mirrored by the VF-14 values, giving more strength to the argument that handicap created by AMD is associated with loss of quality of life.
The handicap can be mitigated with tools or strategies to overcome the limitations caused by the disability [3]. In AMD, referral to LVA clinics is thought to help the patients overcome their disability by the prescription of magnifiers and by advice on how to optimize the remaining visual function. In our study, however, we did not find that LVA clinics were associated with a change in handicap levels or quality of life measurements. We also hypothesized that patients with higher educational attainment may be more adaptable and develop strategies to overcome their visual handicap. However, there was no correlation between education attainment and any of the quality of life tools.
Various studies in the literature have shown that the EQ-5D has poor sensitivity in AMD [5, 6, 8, 9, 15] and our results suggest the same. Firstly, although the EQ-5D had a significant relationship with visual acuity in the BEVA, it did not show a significant association with AMD diagnosis. This is unlike the VF-14, which provides a measure of the visual quality of life and which was highly associated. Furthermore, patients who stopped driving because of AMD had lower VF-14 and LHS values but showed no difference in EQ-5D values. Moreover, the vision bolt-on dimension, which was highly associated with visual acuity, AMD diagnosis, VF-14, and LHS was not significantly associated with the EQ-5D scores. Finally, the number of patients rating their vision as extremely impaired was in contrast with the rest of the five dimensions. These findings support that the utility value generated by the EQ-5D does not accurately reflect the quality of life in patients with AMD.
In order to see if we could improve the sensitivity of EQ-5D, a bolt-on vision dimension was added to the questionnaire. This has been described in previous studies with encouraging results [12, 16]. The EQ-5D-VIS bolt-on dimension was more sensitive to visual acuity loss and showed better correlations with VF-14 and LHS (R2 44% in VF-14 vs 26% in LHS vs 9% in EQ-5D). Multivariate analysis testing all the EQ-5D original dimensions and the bolt-on vision dimensions in the VF-14 and LHS showed that vision was the most important factor in the VF-14 and that it was also very important in the LHS. These results support that a vision bolt-on dimension could increase the EQ-5D sensitivity. Luo and colleagues have used experimental utility values created previously [11] to see if this vision-enhanced tool detected differences between individuals with vision problems and controls [12]. They found that this tool was more sensitive than the original EQ-5D. A preliminary report of this bolt-on visual dimension has suggested that this may be the most accurate and sensitive method to measure changes in quality of life after cataract surgery [17]. The EQ-5D-VIS is a promising compromise between the need for a generic quality of life tool that looks into an important dimension of an individual with AMD.
This study helps validate the NICE AMD classification. Its purpose was to be used as a communication tool with patients. We showed that it is highly correlated with best eye visual acuity and visual quality of life. The correlation with visual acuity is expected, as under the new classification vision is one of the parameters that help to allocate the diagnosis. The new terminology helps to predict the visual quality of life and to provide an insight into the visual disability created by AMD. It clearly also has good face validity as the terms correlate with etiology and with management.
This study is a cross-sectional survey of patients attending a single clinic. Furthermore, most of the patients were Caucasian and this potentially limits its generalizability. More work with higher numbers and higher diversity needs to be done.
These findings are important to the field of AMD. They show that the new classification performed reasonably well in predicting disability and handicap. The results show that visual impairment in AMD has a measurable impact on the patient’s handicap and quality of life, and also suggest that handicap is a measurement that should be used regularly. Finally, this study adds to the evidence in the literature that the EQ-5D has poor sensitivity in AMD and suggests that the addition of a bolt-on vision dimension to the EQ-5D can increase its sensitivity and provide a better indication of the effects of AMD on the patient’s quality of life.
Summary
What was known before
-
AMD affects negatively the quality of life; EQ-5D has limited value in the quality of life assessment in visual disorders.
What this study adds
-
New NICE AMD classification predicts visual acuity and visual related quality of life.
-
The inclusion of bolt-on vision dimension in the EQ-5D may increase sensitivity in AMD.
References
Chakravathy U, Evans J, Rosenfeld PJ. Age related macular degeneration. BMJ. 2010;340:c981
McDowell I, Jenkinson C. Development standards for health measures. J Health Serv Res Policy. 1996;1:238–46.
Harwood RH, Rogers A, Dickinson E, Ebrahim S. Measuring handicap: the London handicap scale, a new outcome measure for chronic disease. Qual Health Care. 1994;3:11–16.
Finger RP, Fenwick E, Hirneiss CW, Hsueh A, Guymer RH, Lamoureux EL, et al. Visual impairment as a function of visual acuity in both eyes and its impact on patient reported preferences. PloS ONE. 2013;8:e81042.
Espallargues M, Czoski-Murray CJ, Bansback NJ, Carlton J, Lewis GM, Hughes LA, et al. The impact of age-related macular degeneration on health status utility values. Investig Ophthalmol Vis Sci. 2005;46:4016–23.
Tosh J, Brazier J, Evans P, Longworth L. A review of generic preference-based measures of health-related quality of life in visual disorders. Value Health. 2012;15:118–27.
Petrou S, Hockley C. An investigation into the empirical validity of the EQ-5D and SF-6D based on hypothetical preferences in a general population. Health Econ. 2005;14:1169–89.
Bozzani FM, Alavi Y, Jofre-Bonet M, Kuper H. A comparison of the sensitivity of EQ-5D, SF-6D and TTO utility values to changes in vision and perceived visual function in patients with primary open-angle glaucoma. BMC Ophthalmol. 2012;12:43.
Mackenzie PJ, Chang TS, Scott IU, et al. Assessment of vision-related function in patients with age-related macular degeneration. Ophthalmology 2002;109:720–9.
Heintz E, Wiréhn AB, Peebo BB, Rosenqvist U, Levin LA. QALY weights for diabetic retinopathy-a comparison of health state valuations with HUI-3, EQ-5D, EQ-VAS, and TTO. Value Health. 2012;15:475–84.
Yang Y, Rowen D, Brazier J, Tsuchiya A, Young T, Longworth L. An exploratory study to test the impact on three “bolt-on” items to the EQ-5D. Value Health. 2015;18:52–60.
Luo N, Wang X, Ang M, Finkelstein EA, Aung T, Wong TY, et al. Vision “bolt-on” item could increase the discriminatory power of the EQ-5D index score. Value Health. 2015;18:1037–42.
NICE guideline [NG82]. Age-related macular degeneration. https://www.nice.org.uk/guidance/ng82. Accessed 13 Mar 2020.
Kulkarni BB, Leighton P, King AJ. Exploring patients’ expectations and preferences of glaucoma surgery outcomes to facilitate healthcare delivery and inform future glaucoma research. Br J Ophthalmol. 2019;103:1850–5.
Pearson I, Rycroft C, Irving A, Ainsworth C, Wittrup-Jensen K. A systematic literature review of utility weights in wet age-related macular degeneration. J Med Econ. 2013;16:1307–16.
Finch AP, Brazier JE, Mukuria C. Selecting bolt-on dimensions for the EQ-5D: examining their contribution to health-related quality of life. Value Health. 2019;22:50–61.
Gandhi M, Ang M, Teo K, Wong CW, Wei YC, et al. A vision ‘bolt-on’ increases the responsiveness of EQ-5D: preliminary evidence from a study of cataract surgery. Eur J Health Econ. 2020;21:501–11.
Acknowledgements
We thank Rowan Harwood for his help with LHS calculations. We also thank Apostolos Fakis for his help with statistical advice on sample size.
Author information
Authors and Affiliations
Contributions
All listed authors have been involved in the conception of study or acquired data. All authors have played a role in interpreting the results, reviewing the manuscript, and approved the final version. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
De Sousa Peixoto, R., Krstic, L., Hill, S.C.L. et al. Predicting quality of life in AMD patients—insights on the new NICE classification and on a bolt-on vision dimension for the EQ-5D. Eye 35, 3333–3341 (2021). https://doi.org/10.1038/s41433-021-01414-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01414-3
This article is cited by
-
Predictors of problems reported on the EQ-5D-3L dimensions among people with impaired vision in northern Portugal
Health and Quality of Life Outcomes (2022)
-
Anxiety levels moderate the association between visual acuity and health-related quality of life in chronic eye disease patients
Scientific Reports (2022)
-
A Patient Perspective on Quality of Life with wAMD: A Podcast
Ophthalmology and Therapy (2022)