Abstract
Purpose
To evaluate the correlation between foveal changes in the detached retina in macula-off rhegmatogenous retinal detachments (RRD) and visual acuity outcome following repair.
Design
Retrospective, consecutive, observational case series.
Methods
Consecutive patients presenting with macula-off RRD between July 15 and September 15, 2017, underwent SD-OCT imaging and their medical records were reviewed. Specific OCT exam parameters were used to evaluate the fovea of the detached retina.
Results
In total, 47 patients with macula-off RRD were treated from July 15 to September 15, 2017. Forty-four eyes of 44 patients could be imaged by SD-OCT and were included in the analysis. Univariate analysis demonstrated a correlation between the height of the detachment, the duration of symptoms, the presence of macular hole and epiretinal membrane to the final VA. Correlation was also found between the presence of MH and the height of the detachment. However, multiple regression analysis demonstrated only a statistically significant correlation between the presence of a macular hole or an epiretinal membrane to the final VA.
Conclusions
Our study is the first to demonstrate the significance of foveal changes in the pathogenesis of lost vision in macula-off retinal detachments. The high rate of macular holes and the correlation between the MH and the height of the detachment suggest that elevated tension in the fovea in high detachments might play a significant role in the visual outcome of macula-off RRD following repair.
Similar content being viewed by others
Introduction
Rhegmatogenous retinal detachment (RRD) is an important cause of visual impairment and requires surgical treatment. The three main treatments options include pneumatic retinopexy (PR), pars plana vitrectomy (PPV) and scleral buckling (SB) [1]. Even with a good post-operative anatomic outcome, patients with macula-off RRD often have an incomplete visual recovery [2, 3]. Many pre-operative factors, including the duration of symptoms, the height of the detachment, pre-operative visual acuity, and optical coherence tomography (OCT) findings have been reported to correlate with the postoperative visual acuity [4,5,6,7,8,9,10].
OCT is the most accurate method to image the foveal structure in patients with macula-off RRD [4, 11,12,13,14,15,16]. A few retrospective case series have been able to demonstrate correlations between variables in the OCT, such as cavities in the inner nuclear layer (INL) and/or outer nuclear layer (ONL), retinal height of detachment at the fovea and subfoveal choroidal thickness (SCT) and the functional outcomes [7, 11, 13, 14, 17, 18]. Limitations in those studies include the inherent selection bias and the difficulty demonstrating the fovea on SD-OCT in a detached retina. The use of standard OCT scan parameters can only reliably capture the fovea in the setting of shallow detachments and hence will not demonstrate the fovea in more complex and bullous retinal detachments.
In the present study, we used specific OCT parameters to demonstrate the fovea in macula-off RRD and evaluated pre-operative clinical data and the SD-OCT findings in a consecutive group of patients with macula-off RRD. We aimed to assess which factors including pre-operative and surgical data correlate with the functional outcomes after retinal detachment surgery.
Materials and methods
This study was performed with approval from the Research Ethics Board at the Sunnybrook Health Sciences Centre, Toronto, Canada and the research was conducted with the adherence to the guidelines of the Declaration of Helsinki. As this is a chart-review retrospective study, no consent was obtained.
This was a retrospective, consecutive, observational case series. Data was retrospectively abstracted from the medical records of patients presenting with macula-off RRD between July 15 and September 15, 2017, at the Sunnybrook Health Sciences Centre, Toronto, Canada. Patients with any of the following conditions were excluded: previous retinal detachment, less than 6 months of follow up after surgery and any known preceding macular disease that could affect the final visual acuity.
Data collected included demographic characteristics, visual acuity, clinical characteristics of the retinal detachment (location, extent, number of tears), duration of retinal detachment, treatment, anatomical success at first surgery, lens status and intraocular pressure. The duration of macular detachment was based on the onset of central visual loss as reported by the patient and was defined as the time between the onset of the central visual decrease and the time of intervention. Best-corrected visual acuity (BCVA) was evaluated using the Snellen visual acuity (VA) chart and the data was converted to the logarithm of the minimum angle of resolution (logMAR) scale. When a patient could not read text 1 m away, VA was measured by counting fingers or by hand movement and was converted to a logMAR value of 1.8 or 2.4, respectively.
All OCT images were performed using the Cirrus HD-OCT (Carl Zeiss Meditec, Dublin, CA). Specific OCT examination parameters were used in our centre to image the fovea of the pre-operative detached retina. The optic nerve head was used as a landmark and five horizontal high definition (raster) lines at a length of 9 mm were obtained (Fig. 1). We found that positioning the nasal end of the superior-most raster line at the centre of the optic nerve head allowed imaging of the fovea in almost all cases.
A Five high definition (raster) lines at a length of 9 mm in a macula off RRD. The position of the top 5 lines in the optic nerve gives a good demonstration of the fovea with schisis-like changes in the OPL. B The fovea in chronic macula-off RD with subretinal depositions (arrow head). C SD-OCT demonstrating the height measurement from the outer retina to the hyper-reflective area of the RPE (arrow). D Foveal SD-OCT demonstrating tension in the foveal area with minimal residual outer retina.
The pre-operative OCT parameters recorded and included in the analysis were: RD height (which was manually measured as the shortest line segment from the outer retinal border of the thinnest area of the fovea to the centre of the hyperreflective area of the RPE, Fig. 1), intraretinal morphologic changes, and foveal and sub-retinal pathologic findings (epiretinal membrane, macular hole, and subretinal depositions). All OCT findings were evaluated by one of the authors (AH), who was masked to clinical data.
Descriptive statistical methods (mean, standard deviation) were used for characteristics such as age, sex, eye, and logMAR BCVA. Comparisons of variables between groups were performed using an independent t-test or ANOVA. Correlations between parameters were determined using Pearson’s test for linear variables and Spearman correlation for non-linear variables. Multiple linear regression analysis was carried out with stepwise modelling to determine which factors influenced the postoperative functional outcome. p < 0.05 was considered statistically significant. Statistical analyses used SPSS version 25.0 (SPSS Inc, Chicago, IL, USA).
Results
From July 15 to September 15, 2017, 47 patients were presented to our institute with macula-off RRD. We were able to demonstrate the fovea in 44 out of the 47 patients (93%). In 3 patients, the fovea could not be imaged by the pre-operative OCT, one patient due to significant vitreous haemorrhage, one patient had overhanging retina blocking the view of the fovea and one patient was not able to cooperate. All patients reached 6 months follow-up and 44 eyes of 44 patients were included in the analysis.
The mean patient age was 57.4 ± 21.1 years; 22 (50%) patients were treated with pneumatic retinopexy (PR), 17 (38.6%) were treated with pars plana vitrectomy (PPV) and 5 (11.4%) with scleral buckling. Twenty six (59.1%) patients were phakic at presentation, 7 of those were treated with PPV and 3 developed visual significant cataract during the six months follow up period and underwent cataract extraction before their last follow up. Six (27%) patients who were first treated with pneumatic retinopexy needed a second surgery to reattach the retina. All six were attached at the final follow up. Three (17%) patients who initially underwent PPV required a second surgery and 2 of these failed repeat surgeries. All SB patients were successfully reattached with a single procedure. No statistically significant difference in the final visual acuity was found between the PR and PPV groups.
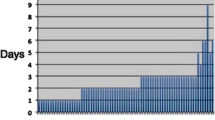
The mean duration of macular detachment was 41.5 ± 87.2 days (range, 1 to 356 days), with 14 days or less in 33 (76%) patients. Using the optic nerve as a landmark with the specific OCT parameters described above allowed us to image the fovea in bullous detachments. The height of the detachment was measured as the shortest line segment from the outer retinal border to the centre of the hyperreflective area of the RPE. (Fig. 1). Using this method, we were able to measure foveal detachment height up to 1826 µm. The average height of the detached macula was 869.36 ± 587.71 µm (range, 53 to 1826 µm).
While analysing the OCT images, we found three characteristic retinal changes in the detached retina: schisis-like changes/fluid in the outer plexiform layer (OPL), schisis-like changes/fluid in the inner nuclear layer (INL), and folds in the outer retina. We also documented the presence of epiretinal membrane, macular hole and subretinal depositions (Fig. 1). In patients with symptoms of less than two weeks duration, outer plexiform changes were found in 97% (32/33), retinal folds were found in 18% (6/33) and INL changes in 20% (7/33). In 18% (6/33) of patients, macular hole was demonstrated, either a full thickness macular hole or with a thin residual outer retinal remnant and 3% (1/33) had ERM. In patients with symptoms of more than two weeks duration, the most common findings were outer plexiform changes (6 patients, 60%) and subretinal depositions and epiretinal membrane, present in 30% of patients (3 patients) (Table 1).
Correlations between pre-operative variables
Correlations were examined between the retinal findings on OCT, the duration of symptoms and the RD height and the pre-operative VA. The main factor that correlated with pre-operative VA was the RD height (r = 0.519, p < 0.0001). Some OCT findings were also found to correlate with the pre-operative VA. Both presence of a macular hole (p = 0.047) and ERM (p = 0.037) were correlated with pre-operative VA (r = 0.311 and r = 0.339 respectively). No correlation was founded between macula-off duration and pre-operative VA (p = 0.354). Macula-off duration did have a correlation with the presence of subretinal depositions in the OCT (p = 0.001), likely secondary to the formation of proliferative vitreoretinopathy with long-standing detachment. A correlation was found between RD height and the presence of a macular hole (r = 0.334, p = 0.027) but not to any other OCT finding.
Correlations between pre-operative variables and final VA
Correlations between retinal findings on OCT; duration of symptoms; success rate of the first surgery; lens status and the RD height and the visual acuity at the time of the last follow up were explored. Correlations were found between visual acuity at presentation; height of the detachment; and duration of symptoms and final VA (p = 0.001, 0.003 and 0.03 respectively). We also found correlations between the presence of a macular hole or epiretinal membrane and final visual acuity (p = 0.02 and p = 0.03 respectively).
In the multiple regression analysis, statistically significant correlations were found between presence of a MH; presence of an epiretinal membrane; and success of the first surgery and final VA (p = 0.003, p = 0.007 and p = 0.006, respectively). The correlations that had been found between the height of the detachment and duration of symptoms to final visual acuity were found not to be statistically significant once multiple regression analysis was used (Table 2).
Patients with acute or sub-acute retinal detachment
In order to examine the effect of the duration of symptoms in the setting of acute or subacute detachment, we performed the same analysis on the subgroup of patients with symptoms of less than fourteen days duration. In total, 33 patients were included in this analysis. The average duration of loss of vision symptoms in this group was five days.
Correlations were found between visual acuity at presentation and the height of the detachment and final VA (p = 0.036, 0.014, respectively). A correlation was also found between the presence of a macular hole and final visual acuity (p = 0.012). No correlation was found between the duration of symptoms and final visual acuity in patients with symptoms than less than 14 days (p = 0.184).
In multiple regression analysis, a statistically significant correlation was only found between the presence of MH and final VA (p = 0.004). The correlation that was found between the height of the detachment to final visual acuity was not statistically significant.
Macular hole patients
Sub-analysis was done to the subgroup of patients with macular hole at presentation. Six patients had macular hole at presentation, three had a full thickness macular hole and three had thin residual outer photoreceptors. Patients with a MH had worse initial visual acuity, higher detachment and worse visual outcomes (Table 3). All six patients were treated with pneumatic retinopexy. Five were successfully reattached after PR. One patient had persistent fluid and was successfully reattached with PPV. Five patients had full thickness macular hole six weeks after surgery and all underwent successful PPV with ILM peeling and subsequent hole closure. One patient had spontaneous hole closure but developed significant ERM and underwent later PPV for ERM peeling.
Discussion
Changes in foveal architecture found on SD-OCT after macula-off RRD have been described and previous studies have shown their correlation to final visual acuity and residual visual complaints. Few studies have also been able to demonstrate a correlation between SD-OCT findings in the detached retina and final visual acuity [4, 11,12,13,14,15,16].
Wolfensberger et al. [19] reported that macular oedema correlated with poorer postoperative visual acuity, and Cho et al. [14] found that the presence of undulations of the separated outer retina was associated with a poorer visual prognosis. In other studies, Nakanishi et al. [4] and Kang et al. [11] failed to find a correlation between those findings and visual outcome. Other pre-operative variables that were reported as having predictive value for final postoperative visual acuity were the height of the macular detachment and the duration of the symptoms [4, 5, 20]. Park et al. postulated that external limiting membrane integrity could be another factor correlated to the final visual outcome [7].
Most of these retrospective case series contain inherent selection bias. Imaging the fovea with SD-OCT in a detached retina can be challenging and using routine OCT protocols, only shallow and easily demonstrable detachments can be imaged well. In our series, we used the optic nerve as a landmark and placed the edge of the superior-most of five high definition (raster) lines at the centre of the optic nerve head. Using this technique, we were able to demonstrate the fovea in the detached retina in 44 out of the 47 patients presented to our institute with macula-off RRD from July 15 to September 15, 2017.
We believe the use of the OCT methods described above allowed us to image the fovea in a very high proportion of patients with high retinal detachment, images that were not obtained in previous studies. The two main differences in OCT characteristics in our study compared to previous studies were the average detachment height and the prevalence of a macular hole in the detached retina. Previous studies showed an average detachment height of around 500 µm [6]. In our study, the average height was 869 ± 587 µm (range, 53 to 1826 µm). Six patients (6/44, 13%) in our study presented with secondary macular holes, a much higher percentage than reported previously. The average height of the detachment in those MH patients was 1357.17 ± 423.34 µm (range, 703 to 1,826 µm).
It is important to mention that, as described above, we measured the detachment height as the shortest line segment from the outer retinal border of the thinnest area of the fovea to the centre of the hyperreflective area of the RPE. In MH cases, where we cannot identify the centre of the fovea, we measured the shortest distance from the outer retinal border of the nasal edge of the macular hole to the hyperreflective area of the RPE. Another limitation of our study was that the measurement technique of the foveal detachment height by OCT has not been validated by past publications and were made by a single investigator in our study and hence did not allow us to assess the inter-observer variability of the height measurements. Although a small variation in the foveal detachment height measurements might occur, we do not believe it would be significant to the study findings.
The high detachment in the MH patients may partially explain the high prevalence of macular holes in our study relative to others. We hypothesize that previous studies underdiagnosed MHs due to the challenge in obtaining an image of the fovea in such high retinal detachments. MHs may resolve spontaneously after PPV for RRD and therefore will not be diagnosed at a later stage. As we do not have the axial length or refractive status of our patients, we cannot rule out that higher than expected prevalence of high myopia in our MH patients but don’t believe that this was a significant contributor to the high prevalence of MH in our study.
Like previous studies, correlation was found between the height of the detachment and the final visual acuity. Interestingly, once we performed a multivariable regression analysis, those correlations were no longer found to be statistically significant. The only pre-operative variable that was found to have a significant correlation was the presence of MH. Our study is the first to demonstrate the significance of macular hole formation in the pathogenesis of lost vision in macula-off retinal detachments.
The only variable, other than MH formation, to have a significant correlation to final visual acuity in the multivariate regression analysis was the success rate in the first surgery. In our study, six (27%) patients who were first treated with pneumatic retinopexy and three patients (17%) who initially underwent PPV required a second surgery. Although failure of the first surgery may have caused a confounding effect and prevented recognition of other significant correlations, we believe that due to the fact there was no correlation between the success rate in the first surgery and the detachment height, the duration of symptoms or MH formation it did not have a significant effect in our study.
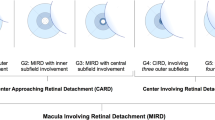
As macular hole formation in the process of retinal detachment was demonstrated only sporadically in the past, the exact mechanism of its formation is uncertain. One explanation could be vitreo-mauclar traction (VMT) on the fovea during the acute posterior vitreous detachment process at the time of the retinal tear and detachment. VMT is believed to be the mechanism of idiopathic macular hole formation [21]. Another mechanism could be cyst rupture. This mechanism was suggested in the past as a mechanism for traumatic macular hole [21, 22]. However, in our series, patients that developed MH had minimal intraretinal fluid. Johnson et al. [23] suggested a different mechanism for the formation of traumatic macular holes. They hypothesized that the tamponade-like movement of the posterior pole may cause traction force along the surface of the retina in a tangential manner. The high prevalence of macular hole formation in high macula-off detachments suggests that similar forces could be the reason for MH formation in our series. As the retina is anchored at the optic nerve and the vitreous base, in a high retinal detachment, during the detachment process, the wall tension in the retina is elevated and there are tangential traction forces on the foveal region, along the retina (Fig. 2). Those traction forces could cause macular hole and can explain the previous report demonstrating correlation between the height of the detachment and the final visual acuity. This theory bears further study.
Summary
What was known before
-
Many preoperative factors, including the duration of symptoms, the height of the detachment, preoperative visual acuity, and optical coherence (OCT) findings have been reported to correlate to the visual acuity results after RRD.
What this study adds
-
The high prevalence of Macula hole in macula-off detachment with significant retinal elevation and its correlation to final visual acuity offers another explanation to the mechanism of loss of vision – tangential traction forces on the foveal region.
References
Schwartz SG, Flynn HW, Mieler WF. Update on retinal detachment surgery. Curr Opin Ophthalmol. 2013;24:255–61. https://doi.org/10.1097/ICU.0b013e32835f8e6b
Gerding H, Hersener A. Anatomical and functional results of primary pars plana vitrectomy in rhegmatogenous retinal detachment. Klin Monbl Augenheilkd. 2013;230:409–12. https://doi.org/10.1055/s-0032-1328392
Schmidt JC, Rodrigues EB, Hoerle S, Meyer CH, Kroll P. Primary vitrectomy in complicated rhegmatogenous retinal detachment–a survey of 205 eyes. Ophthalmologica. 2003;217:387–92. https://doi.org/10.1159/000073067
Nakanishi H, Hangai M, Unoki N, Sakamoto A, Tsujikawa A, Kita M, et al. Spectral-domain optical coherence tomography imaging of the detached macula in rhegmatogenous retinal detachment. Retina. 2009;29:232–42. https://doi.org/10.1097/IAE.0b013e31818bcd30
Kim JD, Pham HH, Lai MM, Josephson JW, Minarcik JR, Von, Fricken M. Effect of symptom duration on outcomes following vitrectomy repair of primary macula-off retinal detachments. Retina. 2013;33:1931–7. https://doi.org/10.1097/IAE.0b013e3182877a27
Karacorlu M, Sayman Muslubas I, Hocaoglu M, Arf S, Ersoz MG. Correlation between morphological changes and functional outcomes of recent-onset macula-off rhegmatogenous retinal detachment: prognostic factors in rhegmatogenous retinal detachment. Int Ophthalmol. 2018;38:1275–83. https://doi.org/10.1007/s10792-017-0591-6
Park DH, Choi KS, Sun HJ, Lee SJ. Factors associated with visual outcome after macula-off rhegmatogenous retinal detachment surgery. Retina. 2018;38:137–47. https://doi.org/10.1097/IAE.0000000000001512
Mowatt L, Shun-Shin GA, Arora S, Price N. Macula off retinal detachments. How long can they wait before it is too late? Eur J Ophthalmol. 2018;15:109–17. http://www.ncbi.nlm.nih.gov/pubmed/15751248 Accessed December 6
Lecleire-Collet A, Muraine M, Menard J-F, Brasseur G. Predictive visual outcome after macula-off retinal detachment surgery using optical coherence tomography. Retina. 2005;25:44–53. http://www.ncbi.nlm.nih.gov/pubmed/15655440 Accessed December 6, 2018
Ross W, Lavina A, Russell M, Maberley D. The correlation between height of macular detachment and visual outcome in macula-off retinal detachments of ≤7 days’ duration. Ophthalmology. 2005;112:1213–7. https://doi.org/10.1016/j.ophtha.2005.01.040
Kang HM, Lee SC, Lee CS. Association of spectral-domain optical coherence tomography findings with visual outcome of macula-off rhegmatogenous retinal detachment surgery. Ophthalmologica. 2015;234:83–90. https://doi.org/10.1159/000381786
Theodossiadis PG, Theodossiadis GP, Charonis A, Emfietzoglou I, Grigoropoulos VG, Liarakos VS. The photoreceptor layer as a prognostic factor for visual acuity in the secondary epiretinal membrane after retinal detachment surgery: imaging analysis by spectral-domain optical coherence tomography. Am J Ophthalmol. 2011;151:973–80. https://doi.org/10.1016/j.ajo.2010.12.014
Gharbiya M, Grandinetti F, Scavella V, Cecere M, Esposito M, Segnalini A et al. Correlation between spectral-domain optical coherence tomography findings and visual outcome after primary rhegmatogenous retinal detachment repair. Retina. 2012;32:43–53. https://doi.org/10.1097/IAE.0b013e3182180114
Cho M, Witmer MT, Favarone G, Chan RP, D’Amico DJ, Kiss S. Optical coherence tomography predicts visual outcome in macula-involving rhegmatogenous retinal detachment. Clin Ophthalmol. 2012;6:91–6. https://doi.org/10.2147/OPTH.S28173
Sayman Muslubas I, Hocaoglu M, Ersoz MG, Arf S, Karacorlu M. Choroidal thickness in chronic rhegmatogenous retinal detachment before and after surgery, and comparison with acute cases. Int Ophthalmol. 2018;38:1035–42. https://doi.org/10.1007/s10792-017-0556-9
Delolme MP, Dugas B, Nicot F, Muselier A, Bron AM, Creuzot-Garcher C. Anatomical and functional macular changes after rhegmatogenous retinal detachment with macula off. Am J Ophthalmol. 2012;153:128–36. https://doi.org/10.1016/j.ajo.2011.06.010
Hagimura N, Suto K, Iida T, Kishi S. Optical coherence tomography of the neurosensory retina in rhegmatogenous retinal detachment. Am J Ophthalmol. 2000;129:186–90. http://www.ncbi.nlm.nih.gov/pubmed/10682971 Accessed December 6, 2018
Smith AJ, Telander DG, Zawadzski RJ, Choi SS, Morse LS, Werner JS, et al. High-resolution fourier-domain optical coherence tomography and microperimetric findings after macula-off retinal detachment repair. Ophthalmology. 2008;115:1923–9.
Wolfensberger TJ, Gonvers M. Optical coherence tomography in the evaluation of incomplete visual acuity recovery after macula-off retinal detachments. Graefes Arch Clin Exp Ophthalmol. 2002;240:85–9. http://www.ncbi.nlm.nih.gov/pubmed/11931084 Accessed December 6, 2018
Guérin CJ, Lewis GP, Fisher SK, Anderson DH. Recovery of photoreceptor outer segment length and analysis of membrane assembly rates in regenerating primate photoreceptor outer segments. Invest Ophthalmol Vis Sci. 1993;34:175–83. http://www.ncbi.nlm.nih.gov/pubmed/8425823 Accessed December 6, 2018
Duker JS, Kaiser PK, Binder S, de Smet MD, Gaudric A, Reichel E, et al. The international vitreomacular traction study group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology. 2013;120:2611–9. https://doi.org/10.1016/j.ophtha.2013.07.042
Yanagiya N, Akiba J, Takahashi M, Shimizu A, Kakehashi A, Kado M, et al. Clinical characteristics of traumatic macular holes. Jpn J Ophthalmol. 1996;40:544–7.
Johnson RN, McDonald HR, Lewis H, Grand MG, Murray TG, Mieler WF, et al. Traumatic macular hole: observations, pathogenesis, and results of vitrectomy surgery. Ophthalmology. 2001;108:853–7. https://doi.org/10.1016/S0161-6420(00)00650-3
Author information
Authors and Affiliations
Contributions
AH was responsible for designing the protocol, writing the protocol and report, conducting the statistics, extracting and analysing data, interpreting results and summary the finding. RT contributed to writing the report, extracting and analysing data and interpreting results. AA contributed to extracting and analysing data, interpreting results and writing the protocol. PK and KE contributed to designing the protocol.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hostovsky, A., Trussart, R., AlAli, A. et al. Pre-operative optical coherence tomography findings in macula-off retinal detachments and visual outcome. Eye 35, 3285–3291 (2021). https://doi.org/10.1038/s41433-021-01399-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01399-z
This article is cited by
-
Impact of duration of silicone oil tamponade on foveal and parafoveal thickness in rhegmatogenous retinal detachment: a retrospective cohort study
International Ophthalmology (2024)
-
The prognostic implication of visual acuity at the time of uveal melanoma diagnosis
Eye (2023)
-
How should we report the foveal status in eyes with “macula-off” retinal detachment?
Eye (2023)
-
A mathematical determination of foveal attachment in primary rhegmatogenous retinal detachment when obscured by bullous retina
International Journal of Retina and Vitreous (2022)