Abstract
Background
The use of monoscopic cameras for glaucoma screening is increasing due to their portability, lower cost, and non-mydriatic capabilities. However, it is important to compare the accuracy of such devices with stereoscopic cameras that are used clinically and are considered the gold standard in optic disc assessment. The aim of this study is to compare vertical cup-to-disc ratio (VCDR) estimates obtained using images taken with a monoscopic and stereoscopic camera.
Methods
Participants were selected from the Tema Eye Survey. Eligible subjects had images of at least one eye taken with two cameras. They were classified as meeting the glaucoma threshold if an eye had a VCDR estimate >97.5th percentile, corresponding to >0.725 for this population. Hence, we used 0.725 as the cutoff to group eyes into two categories: positive and negative. We calculated sensitivity, specificity, and predictive values of VCDR assessed by expert readers at a reading center for monoscopic photos using stereoscopic photos as the gold standard.
Results
Three hundred and seventy-nine eyes of 206 participants were included in the study. Most participants were female (60.2%) and the most common age group was 50–59 years (36.4%). Sixteen eyes met the glaucoma threshold (VCDR > 0.725). Of these, the VCDR estimates of 14 eyes (87.5%) disagreed on the glaucoma threshold from the two cameras. The sensitivity to detect glaucoma with the monoscopic camera was 14.3% (95% CI: 4.0, 40.3).
Conclusions
The low sensitivity of monoscopic photos suggests that stereoscopic photos are more useful in the diagnosis of glaucoma.
Similar content being viewed by others
Introduction
Glaucoma is one of the most common causes of vision loss worldwide. In 2010, an estimated 2.1 million people were blind due to glaucoma, and 4.2 million people were visually impaired [1]. In an urban Ghanaian population aged 40 years and older, the overall prevalence of primary open angle glaucoma was found to be 6.8% [2]. With the increase in life expectancy in sub-Saharan Africa, the burden of age-related diseases such as glaucoma is also expected to rise.
Screening for glaucoma allows early detection, which can reduce vision loss and blindness through early treatment. Grødum and colleagues found that participants diagnosed with glaucoma after population screening had less advanced glaucoma at initial diagnosis compared to those in the same birth cohort that self-selected for seeking help from an ophthalmologist and who were diagnosed with glaucoma in clinic [3]. Diagnosis of glaucoma involves measurement of intraocular pressure (IOP), evaluation of visual field, and assessment of the optic nerve head (ONH) appearance. Unlike the equipment used in clinical settings, less expensive and portable devices that do not require extensive photographic expertise are necessary to screen patients, particularly in under-resourced areas. With advancements in technology, portable, non-mydriatic cameras have been introduced for screening. Therefore, it is important to evaluate their accuracy for glaucoma detection [4].
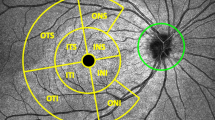
Glaucoma is known to cause distinct structural damage to the ONH. One of the simplest measures used for glaucoma diagnosis is assessment of the vertical cup-to-disc ratio (VCDR), which is a ratio between the vertical diameter of the optic cup and the optic disc [5]. If the VCDR exceeds a certain threshold value or varies significantly from the fellow eye, then the eye is suspected to be glaucomatous. This study aims to compare the VCDR estimates obtained from images taken using two devices: (a) a tabletop simultaneous stereoscopic mydriatic fundus camera, the gold standard for this study and (b) a portable non-mydriatic monoscopic digital fundus camera.
Materials and methods
The Tema Eye Survey (TES) is a population-based study of participants aged 40 years and older from five communities of Tema, Ghana. The detailed study design has been described elsewhere [6]. Briefly, the goal of TES was to determine the prevalence of glaucoma, blindness, and visual impairment in a West African adult population [7]. Among the 5603 patients examined during 2006–2008, 362 (6.5%) were found to have glaucoma. A follow-up study was conducted in 2015–2016 to determine the incidence and progression of glaucoma in the same study population [8]. The data used in this analysis were collected during the follow-up study.
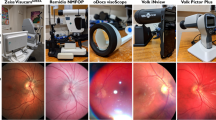
During the follow-up investigation participants without previously diagnosed glaucoma received an initial screening test that consisted of measuring distance visual acuity, IOP, central corneal thickness (CCT), visual field testing, and fundus photography. Visual acuity was measured using a reduced logMAR tumbling E chart at four meters, moving to one meter, if needed. IOP was measured using a Tonopen (Reichert Ophthalmic Instruments, Depew, New York, USA), and CCT was measured by ultrasonic pachymetry (DGH Technology Inc., Exton, Pennsylvania, USA). The anterior segment was examined using a flashlight, and visual field screening tests were performed using the Frequency Doubling Technology perimeter C20-5 program (FDT; Carl Zeiss Meditec, Dublin, California, USA). Non-mydriatic monoscopic optic disc and macular photographs were taken using a Smartscope PRO camera (Optomed Oy, Hallituskatu, Finland) [6, 9].
Participants failed the screening tests if they had best-corrected monocular distance visual acuity worse than 20/40, more than one abnormal spot on FDT for two tests in either eye, average IOP ≥ 21 mmHg on two readings, narrow anterior chamber by flashlight testing, or abnormal optic disc or macular photographs. These participants were recalled to the clinic for a comprehensive eye examination by a glaucoma specialist. This examination involved visual acuity measured using the reduced logMAR tumbling E chart, and automated perimetry using the Humphrey Visual Field Analyzer with 24-2 Swedish Interactive Threshold Algorithm standard metrics (Carl Zeiss Meditec, Dublin, California, USA). Participants also received slit-lamp examination of the anterior segment including Goldmann applanation tonometry, gonioscopy and fundus biomicroscopy with a +90-diopter lens. After dilation, stereoscopic optic disc and macular photographs were taken with a Nidek 3Dx camera (Nidek Co, Ltd, Gamagori, Japan) [6, 9]. Using a secure study website, the optic disc photographs were sent to Moorfields Eye Hospital Reading Center, London, UK to estimate the VCDR.
To be included in this analysis, eyes needed images taken using both the monoscopic and stereoscopic cameras. Hence, all individuals in our analysis failed the initial screening and had returned to the clinic for further assessment. However, our analysis does not include all individuals who returned for the comprehensive assessment because some were missing monoscopic images due to logistical issues in the busy clinic.
Participants were classified as having glaucoma based on Foster et al.’s category 1 definition. Participants were classified as having glaucoma if their eye had a VCDR estimate >97.5th percentile, asymmetry of VCDR between eyes >97.5th percentile for a healthy population, or neuroretinal rim width reduced to <0.1 CDR (between 11 to 1 o’clock or 5 to 7 o’clock) and also showed a definite visual field defect consistent with glaucoma [2, 5]. In our population, the 97.5th percentile corresponds to a VCDR estimate of 0.725 [2]. Hence, we used 0.725 as the cutoff to group eyes into two categories: ≤0.725 (“negative” - did not meet the glaucoma threshold) and >0.725 (“positive” - met the glaucoma threshold). We classified visual impairment based on the United States definition as follows: Normal (logMAR 0 to 0.3; Snellen 20/20 to 20/40), Impaired (logMAR > 0.3–1.0; Snellen > 20/40 to 20/200), and Blind (logMAR > 1.0; Snellen > 20/200).
The primary analyses utilized the Moorfields’ grading for both the monoscopic and stereoscopic images. Moorfields’ expert, non-physician readers were masked to the main study question. We performed a sub-analysis to determine whether image assessment by glaucoma specialists differed from the reading center grading. For the sub-analysis, a subset of the images was independently re-graded by two glaucoma specialists. Images were selected to include all eyes that were discordant in their binary outcome (positive or negative) for the two images based on Moorfields’ grading and a subset of the remaining images, with an oversampling of eyes that had VCDR estimates close to the threshold value on at least one Moorfields’ grade. The glaucoma specialists were masked to the VCDR estimates reported by Moorfields. One of the glaucoma specialists was involved in the study design, and therefore was aware of the study goal while the other was masked to the main study question. All monoscopic images were graded before stereoscopic images for both the overall study and the sub-analysis. Graders and glaucoma specialists used a hand-held stereoscope (Screen-Vu, Portland, OR, USA) to assess VCDR.
The Ethics Committee of the Ministry of Health of Ghana and the Institutional Review Board at the University of North Carolina at Chapel Hill approved the study. The study protocol adhered to the tenets of the Declaration of Helsinki, and all participants provided written informed consent before any study procedures were conducted.
Statistical analysis
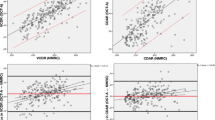
All analyses were conducted using SAS software, version 9.4 (SAS Institute Inc., Cary, North Carolina, USA). Descriptive statistics were used to characterize the study sample. Continuous variables were summarized with means and standard deviations, and categorical variables with frequencies and percentages. The monoscopic and stereoscopic VCDR estimates were categorized into two groups (positive and negative) using the 97.5th percentile as the cutoff, which corresponds to 0.725 for the Tema population. Therefore, the continuous VCDR estimates were categorized into binary groups and sensitivity, specificity, and positive and negative predictive values were calculated using stereoscopically-assessed VCDR estimates as the gold standard. We computed 95% confidence intervals (95% CIs) accounting for correlation between eyes of the same individual. We plotted histograms to assess the distribution of the differences in VCDR estimates obtained from the two devices. To compare the differences, we plotted an enhanced Bland–Altman plot with a regression of the differences in VCDR estimates against the mean. The mean VCDR was calculated by taking the average of the VCDR estimates obtained from the two cameras. For the sub-analysis examining the repeat grading by glaucoma specialists, we calculated the mean difference in VCDR estimates obtained from the two devices for each grader to assess whether any systematic differences exist.
Results
There were 206 participants included in this study. The demographic characteristics of the participants are shown in Table 1. Most participants were female (60.2%) and the most common age group was 50–59 years (36.4%). Thirteen were diagnosed with incident glaucoma.
A total of 379 eyes (92%) had VCDR data available for both stereoscopic and monoscopic cameras. Among these, only 139 eyes (37.9%) had normal vision, 203 eyes (55.3%) failed the FDT test, and 66 eyes (18%) had IOP ≥ 21 mmHg (Table 2). A total of 16 eyes met the glaucoma threshold based on images from at least one camera (Table 3). Among these eyes, the VCDR estimates for 14 eyes (87.5%) disagreed between the two cameras. Twelve of these discrepant eyes met the glaucoma threshold in the stereoscopic images and two met the glaucoma threshold with the monoscopic images. For the 33 eyes excluded from the comparative analysis, only one out of the 15 with only stereoscopic data met the glaucoma threshold, and none of the eyes with only monoscopic data met the glaucoma threshold. The FDT and IOP results for the excluded eyes were similar to all eyes included in the analysis; however, approximately half the excluded eyes were blind.
For the 12 eyes where the stereoscopic image indicated glaucoma but the monoscopic image did not, most (66.7%) failed two other screening criteria and one eye failed three other screening criteria. For the two eyes that reached the glaucoma threshold on the monoscopic but not on stereoscopic images, both had visual impairment and failed the FDT test; however, neither had high IOP. The absolute difference between the stereoscopic and monoscopic VCDR estimates was ≥0.1 for two-thirds of the stereoscopic “positive” eyes. Three of these eyes (25%) had differences between 0.2 and 0.3 and one eye (8.3%) had a difference of 0.4 (data not shown).
Among our study population, there were large differences in the stereoscopic and monoscopic estimates, ranging from −0.25 to 0.40, with an overall mean difference of −0.01 (Fig. 1). However, since the regression line in Fig. 1 moves from a negative to positive VCDR difference, this indicates that for small VCDR estimates, the reading center reported smaller stereoscopic VCDR estimates, but for large VCDR estimates, stereoscopic VCDR estimates were larger compared to monoscopic. The regression line crosses the no-difference line, where stereoscopic and monoscopic VCDR estimates are equal, at ~0.5 mean VCDR. Hence, histograms were plotted to examine variation in the differences above and below this value. For eyes with a stereoscopic VCDR ≥ 0.5, the stereoscopic value was higher than the monoscopic value 67% of the time, while for stereoscopic values <0.5, the stereoscopic value was higher for only 32% (data not shown). A similar pattern was found among the 56 images regraded by the two glaucoma specialists. The mean difference (stereoscopic VCDR-monoscopic VCDR) was 0.08 for grader 1 and 0.13 for grader 2 (data for individual gradings performed by glaucoma specialists not shown). The mean difference in gradings performed by Moorfields for this subset was 0.05.
The sensitivity of the monoscopic camera to detect glaucoma was 14.3% (95% CI: 4.0, 40.3) and the specificity was 99.5% (95% CI: 97.8, 99.9). Additionally, the positive predictive value was 50.0% (95% CI: 19.8, 80.2) and the negative predictive value was 96.8% (95% CI: 94.5, 98.2).
Discussion
This study demonstrated that VCDR estimated using monoscopic images has low sensitivity (14.3%; 95% CI: 4.0, 40.3) to detect glaucoma. Thus, a high proportion of eyes with glaucoma would be missed when using this technique as a screening tool. This finding is important when considering use of this and other non-stereoscopic cameras for glaucoma screening. Most screening tests are designed with high sensitivity in order to maximize the likelihood of identifying disease at an early stage, when treatment may be more effective. Additionally, over-identifying potential cases is preferable to under-identification because further glaucoma assessment of false-positive cases is relatively simple and non-invasive. With a low sensitivity test, there is a higher rate of false negatives, which would prevent early diagnosis and treatment for some individuals who are screened [10]. Given the low sensitivity of monoscopic images in our study, the use of this device would lead to missed cases of glaucoma suspects and delay the potential to receive early treatment that could prevent blindness.
VCDR estimates using monoscopic images, on average, are lower than estimates made using stereoscopic images when estimates are close to the glaucoma threshold. Importantly, the difference in estimates between the two cameras increases as the VCDR estimate increases. Thus, as VCDR estimates reach closer to the glaucoma threshold, there is a larger difference between assessment of stereoscopic and monoscopic images, with the latter more likely to yield estimates below the threshold. Indeed, in this study, of the 14 eyes with glaucomatous VCDR using stereoscopic images, monoscopic images led to underestimation of the VCDR in 12 (85.7%). Interestingly, in two cases, the monoscopic estimate was above the threshold when the stereoscopic estimate was not. The VCDR difference was 0.12 for one eye and 0.05 for the other. Both of these eyes failed the FDT test and had visual impairment. The FDT was designed to detect dysfunction of the magnocellular pathway, specifically Y-like magnocellular (My) cells, which are preferentially affected in glaucoma [11]. FDT has been shown to detect visual field deficits earlier than standard automated perimetry [12, 13]. Given that these two eyes failed multiple screening criteria, they might have early signs of glaucoma. The VCDR difference for both eyes is small and we expect that as the glaucoma severity increases, the stereoscopic VCDR estimate will likely exceed the glaucoma threshold as well.
We further analyzed a subset of images to determine whether the differences between stereoscopic- and monoscopic-related VCDR estimates determined by glaucoma specialists was consistent with the assessment done by the reading center. This sub-analysis had consistent findings, with VCDR estimates from stereoscopic images being larger on average compared to monoscopic images. The differences in VCDR estimates determined by each glaucoma specialist showed the same trend as the assessment done by the Moorfields Reading Center. The results of our analysis are similar to those of prior studies that have indicated larger CDR measurements with stereoscopic versus monoscopic images [14,15,16]. We did not compare interobserver agreement as part of this study because significant variation in assessment of CDR estimates has been previously reported between glaucoma specialists [14], and observers have higher reproducibility with themselves than between each other when assessing the optic disc [16]. Furthermore, findings from Tielsch’s study aimed at comparing intraobserver and interobserver agreement for optic disc assessment recommended using the same observer for assessing stereoscopic photographs [17].
Although monoscopic cameras provide some practical advantages, images acquired from stereoscopic devices capture the three-dimensional nature of the optic disc, allowing proper assessment of cup depth and disc shape [18, 19]. Monoscopic devices such as Smartscope PRO are portable and less expensive than stereoscopic cameras, making them easier to use for community-based screening. Furthermore, they capture optic disc images without requiring pupil dilation; hence, patients need not wait until the mydriatic drops become effective [18, 20]. However, this study found that in comparison to VCDR estimates obtained from the stereoscopic images, VCDR estimates obtained from the monoscopic images had low sensitivity, therefore, limiting its ability to capture glaucoma suspects. Although CDR estimates are not the only factor considered for glaucoma diagnosis, they are used extensively as a screening tool to identify glaucoma suspects [21]. Prior studies comparing effectiveness of glaucoma screening using monoscopic images to direct ophthalmoscope or clinical eye examination have indicated low sensitivity when monoscopic images are used by themselves to detect glaucoma [22,23,24]. The two dimensional nature of non-stereoscopic images fails to capture optic disc contour at the same level as stereoscopic images [14]. Although stereoscopic methods require a stereoviewer, careful alignment, stereopsis, and equipment with higher cost, optic disc evaluation using stereoscopic methods has been considered to be better and more reproducible in comparison to monoscopic methods [7, 14, 16, 23, 25]. A prior study has also indicated that stereoscopic images allow earlier detection of neuroretinal rim changes compared to monoscopic imaging [15]. Hence, the results from this study further support the need to assess optic disc images using stereoscopic methods.
While there have been advancements in the diagnostic techniques for glaucoma and optic nerve health that recommend approaches other than CDR assessments [26], for screening purposes, capturing optic nerve images and assessing CDR estimates remain the standard approach. Given the high resolution, reproducibility, and quantitative assessment of retinal layers provided by optic coherence tomography (OCT), this technology has gained popularity for glaucoma diagnosis. However, it is important to note that the assessment provided by OCT complements the assessment done using optic nerve photographs and should not be considered as a replacement for glaucoma screening and diagnosis. The use of photography during screening enables experts to provide their assessment even while they are not present in the field and is regarded as a useful real-time telemedicine tool [27].
Our study has some limitations. We had a small number of incident glaucoma cases. While we had 206 participants in this study, only 13 were diagnosed with glaucoma. This limits the precision to detect differences between the cameras and resulted in wide confidence intervals. However, given that the monoscopic images missed 85% of the glaucoma cases, it is unlikely that a larger study would yield different results. Given the small sample size of eyes that met the glaucoma threshold and low incidence of glaucoma in our study, we did not calculate kappa statistics, which is generally used as a measure of agreement. Instead, we calculated sensitivity and specificity, which might provide better assessment of agreement between the two devices in this study due to the smaller sample size [28]. Given that monoscopic images were taken before dilation and stereoscopic images after dilation, we are unable to separate out the effect of dilation on identifying glaucoma suspects in this study. Also, it was out of the scope of the study to determine whether pupil dilation impacted the quality of photos and assessment of CDR. Although one study noted that dilation results in images with better quality and optic disc rim visualization [29], several studies have shown that optic disc photos captured with portable non-mydriatic fundus camera are of acceptable quality and allows reliable CDR estimation during screenings [21, 24, 30,31,32]. Given that these portable non-mydriatic devices are being introduced for use in resource-limited settings for screening purposes, it is important to address the impact of these combined features on the overall sensitivity of the monoscopic camera. Furthermore, the cutoff (0.725) used to classify monoscopic VCDR estimates into two categories (positive and negative) was based on the distribution of the stereoscopic VCDR estimates for the Tema population. This may have contributed to the poor sensitivity seen in our study, since a cutoff based on the distribution of monoscopic VCDR estimates might have been more suitable to categorize the monoscopic estimates. However, the clinical standard for diagnosis of glaucoma is based on stereoscopic images; hence, a VCDR distribution of the Tema population based on monoscopic estimates has not been done yet.
Our study has several strengths. First, this study used a population-based design that allowed us to capture a representative sample of the general population and includes a wide variety of optic disc features. Hence, findings from this study can be generalized to the larger Tema population. Second, optic disc images were analyzed by an internationally-renowned ophthalmic reading center. Assessment of optic disc images by a reading center has been recommended for glaucoma prevalence studies [7, 33]. Third, we classified participants as having glaucoma based on the Foster et al.’s definition, which takes into account numerous factors such as visual field defect, VCDR estimate, and neuroretinal rim width. This definition was proposed to standardize glaucoma definition using simple assessment of the structure and function of the optic nerve [5]. Another strength of this study is the inclusion of repeat analysis of a subset of images conducted by two glaucoma specialists. The results from this subanalysis further corroborated our finding based on the reading center’s grading that VCDR estimates obtained from stereoscopic images were larger on average compared to monoscopic images for higher VCDR values.
In conclusion, the low sensitivity of monoscopic in comparison to stereoscopic assessment in this study emphasizes the need to assess optic disc images using stereoscopic devices. For non-invasive screening purposes, it is essential to capture most glaucoma suspects in order to intervene early and limit the risk of further disease progression. Use of stereoscopic devices allows proper assessment of optic disc and hence, should be promoted for glaucoma screening purposes rather than monoscopic devices that results in a higher number of missed glaucoma suspects.
Summary
What was known before
-
Use of monoscopic cameras is increasing for glaucoma screening purposes due to their low cost, portability, and non-mydriatic nature.
What this study adds
-
On average, VCDR estimates obtained using a monoscopic device were smaller in comparison to the estimates obtained from a stereoscopic device. The differences in VCDR estimates increased as the estimates reached closer to the glaucoma threshold.
-
Stereoscopic devices allow better assessment of the VCDR in comparison to monoscopic devices.
References
Bourne RRA, Taylor HR, Flaxman SR, Keeffe J, Leasher J, Naidoo K, et al. Number of people blind or visually impaired by glaucoma worldwide and in world regions 1990–2010: a meta-analysis. PLoS ONE. 2016;11:1–16.
Budenz DL, Barton K, Whiteside-de Vos J, Schiffman J, Bandi J, Nolan W, et al. Prevalence of glaucoma in an urban West African population: the Tema Eye Survey. JAMA Ophthalmol. 2013;131:651–8.
Grødum K, Heijl A, Bengtsson B. A comparison of glaucoma patients identified through mass screening and in routine clinical practice. Acta Ophthalmol Scand. 2002;80:627–31.
Nduaguba C, Lee RK. Glaucoma screening: current trends, economic issues, technology, and challenges. Curr Opin Ophthalmol. 2006;17:142–52.
Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86:238–42.
Budenz DL, Bandi JR, Barton K, Nolan W, Herndon L, Whiteside-De Vos J, et al. Blindness and visual impairment in an urban West African population: the Tema Eye Survey. Ophthalmology. 2012;119:1744–53.
Mwanza JC, Grover DS, Budenz DL, Herndon LW, Nolan W, Whiteside-De Vos J, et al. A comparison of cup-to-disc ratio estimates by fundus biomicroscopy and stereoscopic optic disc photography in the Tema Eye Survey. Eye. 2017;31:1184–90.
Mwanza JC, Tulenko SE, Barton K, Herndon LW, Mathenge E, Hall A, et al. Eight-year incidence of open-angle glaucoma in the Tema Eye Survey. Ophthalmology. 2019;126:372–80.
Mwanza JC, Tulenko SE, Budenz DL, Mathenge E, Herndon LH, Kim HY, et al. Longitudinal change in central corneal thickness in the Tema Eye Survey. Am J Ophthalmol. 2018;186:10–18.
Maxim LD, Niebo R, Utell MJ. Screening tests: a review with examples. Inhal Toxicol. 2014;26:811–28.
White AJR, Sun H, Swanson WH, Lee BB. An examination of physiological mechanisms underlying the frequency-doubling illusion. Investig Ophthalmol Vis Sci. 2002;43:3590–9.
Medeiros FA, Sample PA, Weinreb RN. Frequency doubling technology perimetry abnormalities as predictors of glaucomatous visual field loss. Am J Ophthalmol. 2004;137:863–71.
Bayer AU, Erb C. Short wavelength automated perimetry, frequency doubling technology perimetry, and pattern electroretinography for prediction of progressive glaucomatous standard visual field defects. Ophthalmology. 2002;109:1009–17.
Lichter PR. Variability of expert observers in evaluating the optic disc. Trans Am Ophthalmol Soc. 1977;74:532–72.
Morgan JE, Sheen NJL, North RV, Choong Y, Ansari E. Digital imaging of the optic nerve head: monoscopic and stereoscopic analysis. Br J Ophthalmol. 2005;89:879–84.
Varma R, Steinmann WC, Scott IU. Expert agreement in evaluating the optic disc for glaucoma. Ophthalmology 1992;99:215–21.
Tielsch JM, Katz J, Quigley HA, Miller NR, Sommer A. Intraobserver and interobserver agreement in measurement of optic disc characteristics. Ophthalmology. 1988;95:350–6.
Chan HHL, Ong DN, Kong YXG, O’Neill EC, Pandav SS, Coote MA, et al. Glaucomatous optic neuropathy evaluation (GONE) project: The effect of monoscopic versus stereoscopic viewing conditions on optic nerve evaluation. Am J Ophthalmol. 2014;157:936–44.
O’Neill EC, Gurria LU, Pandav SS, Kong YXG, Brennan JF, Xie J, et al. Glaucomatous optic neuropathy evaluation project factors associated with underestimation of glaucoma likelihood. JAMA Ophthalmol. 2014;132:560–6.
Kirwan JF, Gouws P, Linnell AET, Crowston J, Bunce C. Pharmacological mydriasis and optic disc examination. Br J Ophthalmol. 2000;84:894–8.
Yogesan K, Constable IJ, Barry CJ, Eikelboom RH, Morgan W, Tay-Kearney ML, et al. Evaluation of a portable fundus camera for use in the teleophthalmologic diagnosis of glaucoma. J Glaucoma. 1999;8:297–301.
Kumar S, Giubilato A, Morgan W, Jitskaia L, Barry C, Bulsara M, et al. Glaucoma screening: analysis of conventional and telemedicine-friendly devices. Clin Exp Ophthalmol. 2007;35:237–43.
Newman-Casey PA, Verkade AJ, Oren G, Robin AL. Gaps in glaucoma care: a systematic review of monoscopic disc photos to screen for glaucoma. Expert Rev Ophthalmol. 2014;9:467–74.
Miller SE, Thapa S, Robin AL, Niziol LM, Ramulu PY, Woodward MA, et al. Glaucoma screening in Nepal: Cup-to-disc estimate with standard mydriatic fundus camera compared to portable nonmydriatic camera. Am J Ophthalmol. 2017;182:99–106.
Parkin B, Shuttleworth G, Costen M, Davison C. A comparison of stereoscopic and monoscopic evaluation of optic disc topography using a digital optic disc stereo camera. Br J Ophthalmol. 2001;85:1347–51.
Chauhan BC, Burgoyne CF. From clinical examination of the optic disc to clinical assessment of the optic nerve head: a paradigm change. Am J Ophthalmol. 2013;156:218–27.
Myers JS, Fudemberg SJ, Lee D. Evolution of optic nerve photography for glaucoma screening: a review. Clin Exp Ophthalmol. 2018;46:169–76.
Maa AY, Evans C, Delaune WR, Patel PS, Lynch MG. A novel tele-eye protocol for ocular disease detection and access to eye care services. Telemed e-Health. 2014;20:318–23.
Wintergerst MWM, Brinkmann CK, Holz FG, Finger RP. Undilated versus dilated monoscopic smartphone-based fundus photography for optic nerve head evaluation. Sci Rep. 2018;8:2–8.
LaMonica LC, Bhardwaj MK, Hawley NL, Naseri T, Reupena MS, Cooper ML, et al. Remote screening for optic nerve cupping using smartphone-based non-mydriatic fundus photography. J Glaucoma. 2021;30:58–60.
Bhandary S, Rao L, Addoor K, Katte R, Kusumgar P, Kamath A. Efficacy of cost-effective, portable nonmydriatic fundus camera, manufactured in India, to detect retinal pathology in comparison with regular mydriatic fundus camera. Int J Med Sci Public Heal. 2015;4:835–40.
Parekh B, Venkatesh R. A novel outreach program-using a portable fundus camera for glaucoma screening. Invest Ophthalmol Vis Sci. 2019;60:5514. (abstract)
Kyari F, Gilbert C, on behalf of the Nigeria National Blindness. Agreement in measurement of optic cup-to-disc ratio with stereo biomicroscope funduscopy and digital image analysis: results from the Nigeria national blindness and visual impairment survey. Ophthalmic Epidemiol. 2017;24:57–62.
Acknowledgements
Supported by Glaucoma Research Foundation, San Francisco, CA, USA and Research to Prevent Blindness, New York, NY, USA
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shrestha, R., Budenz, D.L., Mwanza, JC. et al. Comparison of vertical cup-to-disc ratio estimates using stereoscopic and monoscopic cameras. Eye 35, 3318–3324 (2021). https://doi.org/10.1038/s41433-021-01395-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01395-3