Abstract
Purpose
To evaluate the potential effect of age and refractive error on visual acuity (VA) performance and quick contrast sensitivity function (qCSF) in normal Chinese adults.
Method
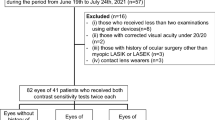
Ninety-two subjects with normal best corrected distance VA (BCDVA) were enrolled in this pilot study. Measurements included BCDVA, best corrected near VA (BCNVA), unaided VA (UNVA), habitual spectacle-corrected near VA (SCNVA) and qCSF. For analyses, subjects were categorized into three age groups (20~40 years, 41~60 year and >60 years) and four refractive groups (hyperopia, emmetropia, myopia and high myopia). Relationships between age, refractive error, types of VA and qCSF were tested using simple and multiple linear regressions analyses.
Result
Mean age and refractive error of the study participants were 44.04 ± 12.68 years and −1.86 ± 2.91D, respectively. Among the stratified age groups, a hyperopic shift of refraction (−3.24 ± 2.88D vs. −1.24 ± 2.64D vs. 0.39 ± 1.42D, respectively; P < 0.001) and a reduction in BCNVA (P = 0.014), SCNVA (P < 0.001) and cut-off spatial frequency (SF) (P = 0.032) were found with increasing age. Among the four refractive groups, the SCNVA and cut-off SF of hyperopia were worse compared to the other refractive statuses (all P < 0.05). Age was significantly associated with cut-off SF (standardized β = −0.29, P = 0.005) after adjustment for SER, gender and all types of VA.
Conclusion
For normal Chinese adults with normal BCDVA, age was the main factor associated with CSF, which may be independent of refractive error.
Similar content being viewed by others
Introduction
An aging population and increase in the prevalence of myopia are two main changes over the last decades. Presbyopia is an age-related loss of accommodation that results in near visual disturbance, and it was forecasted to affect an estimated 1.4 billion people by 2020 [1]. Myopia has become a worldwide public health issue and affects an estimated 22.9% of the world’s population, or 1.406 billion people [2, 3]. The myopia burst in East Asia may cause a significant hyperopic shift of spherical equivalent refractive error (SER) in elderly subjects. This demographic change may lead to a significant cohort effect on near visual performance of presbyopia because refractive error is associated with presbyopia onset [4].
The degeneration of near visual function is one of the main causes of visual impairment in older patients, but testing of the accommodation ability and conventional near vision may be insufficient to evaluate daily near visual performance because various factors, such as reduction in contrast sensitivity function (CSF) [5], pupil size [6] and increasing density of the crystalline lens [7], degrade near visual function with aging rather than an age-related loss of accommodation.
Visual acuity (VA) is the most commonly used psychophysical test, but it only utilize optotypes with high degrees of contrast which may not reflect actual visual performance in the real world [8]. In clinical practice, there are many patients whose subjective complaints do not often correspond with their VA test in the examining room. The CSF test has the advantage of evaluating the ability to see low and high contrast patterns, which tends to be more sensitive than VA assessment alone [9], especially for the presence of disease states when VA and fundus images appear normal. A variety of ophthalmic and neurological conditions may cause CSF deficits that do not depend on the patient’s overall level of visual deficits, such as dry eye [10], ocular hypertension [11] and myopia [12]. The potential inconsistency between VA and CSF deficits suggests that measurement of the full CSF over a wide range of frequencies is clinically important.
Methods of conventional CSF tests are not suitable in clinical practice because these tests are time-consuming (30–60 min). Lesmes et al. [13] recently developed a novel adaptive psychophysical procedure, the quick CSF (qCSF), which directly estimates the entire CSF curve rapidly (5–10 min) with reasonable precision. Research on CSF assessment of ocular diseases states, such as amblyopia [14], diabetic retinopathy [15] and multiple sclerosis [16], using this novel method have been reported, but there remains a need to identify the candidate population with normal corrected distance VA but abnormal CSF using this novel method.
To the best of our knowledge, the effect of demographic changes in the last decades, such as aging and the increasing prevalence of myopia, on visual function in normal East Asian population is not clear. The purposes of this pilot study were to assess the visual functions with qCSF method in normal Chinese adult population with a wide range of age and refractive status, and determine their relationship with age and refractive error to identify candidate subjects for qCSF testing in the future.
Material and methods
Study design
The current study was a pilot study performed at Zhongshan Ophthalmic Center (ZOC) in Guangzhou, China. The ZOC ethical committee approved this study, which was performed in accordance with the tenets of the Declaration of Helsinki. Written consent was obtained from all participants who did not receive any financial compensation.
In the current study, ophthalmic examination included slitlamp biomicroscopy of the anterior and posterior segments with pupillary dilation were performed to identify any eye diseases in each subject prior to enrollment. All participants had a with-the-rule astigmatism no greater than −2.00D and no eye diseases other than refractive error. The interocular difference in refractive error of each subject was less than 1.00D. Subjects were excluded if they had a best corrected distance VA (BCDVA) less than 20/25 in either eye, systemic diseases or use of systemic or topical medications that may affect accommodation and binocular vision. Only the right eye of each subject was included for analysis.
Assessment of refractive error
Before enrollment, cycloplegic refractions using the logMAR visual table at a 5 mm distance were measured in this study. Mydriasis was achieved with the installation of three drops of Guttae tropicamide (0.5% tropicamide plus 0.5% phenylephrine hydrochloride; Xing Qi Ophthalmic Co., Ltd., Shenyang, China) separated by 5 min. Cycloplegic refraction measurement commenced 30 min after the first drop of compound tropicamide instillation. The SER was calculated as the addition of the spherical power and half the magnitude of the cylinder power.
Assessment of VA
Visual acuity examinations included measurements of BCDVA, best corrected near VA (BCNVA), unaided VA (UNVA) and habitual spectacle-corrected near VA (SCNVA). All types of VA were measured using the logMAR VA chart. Subjective refraction was performed to determine VA at near (40 cm) or distance (5 m) via optimal refractive correction. To determine the daily near visual performance, near VA at distance of 40 cm with correction of habitual spectacles (myopes or hyperopia) or no spectacles (emmetropes or moderate hyperopia) was performed to obtain the SCNVA. All VAs were recorded as logMAR values for statistical analyses.
Assessment of CSF
All of the programs used in this study were coded in MATLAB (MathWorks Corp., Natick, MA, USA) using the Psychtoolbox subroutines [17, 18], and run on a PC computer. Stimuli were displayed on a NEC P463 monitor (Gension & Waltai Digital Video System Co., Ltd. China) with a display area of 105.5 × 60.9 cm, a resolution of 1920 × 1080, and a refresh rate of 60 Hz. A special circuit was used to achieve 14-bit grayscale resolution [19]. Participants with optimal refractive correction viewed the stimuli at a distance of 4 m in a dark room.
In each trial, stimuli were randomly presented for 120 ms, followed by a blank screen for 250 ms. A response screen with all ten numbers was shown for 500 ms, and participants were instructed to type the number they saw using the keyboard. No feedback was provided and a new trial started 500 ms after the subject’s response. The number of stimuli of number used in this study were arranged as a 1×3 matrix and presented in the center on the display. One experimental session consisted of 50 trials which took approximately 15 min for each subject.
The CS was estimated at six different spatial frequencies (1, 1.5, 3, 6, 12, and 18cpd). To characterize the CS difference among different categorized groups, the area under the CSF (AULCSF) which is a broad measure of spatial vision [20, 21] and the spatial frequency cutoff (cut-off SF) which characterizes the high-frequency resolution of the visual system [22, 23] were calculated for each subject.
Data analysis
In this study, data were statistically calculated based on gender, age and refractive error, respectively. Two gender groups (men and women), three stratified age groups (20~40 years, 41~60 year and >60 years) and four refractive groups (hyperopia, emmetropia, low and moderate myopia (L&M myopia) and high myopia) were categorized. Refractive statuses were defined based on the following SER: hyperopia, ≥0.50D; emmetropia, (−0.50D, 0.50D); L&M myopia, (−6.00D, −0.50D]; and high myopia, ≤−6.00D.
All statistical analyses were performed using SPSS Version 16.0 (SPSS 16.0, Inc., Chicago, IL, USA). Data were firstly tested for normality using the Sample Shapiro-Wilk test. Difference between gender groups were compared using an independent-samples t test. Difference among the three age groups or the four refractive groups were compared using one way ANOVA analyses. Simple and multiple linear regressions analysis were used to evaluate the potential association between gender, age, refractive errors, or VA with CSF, respectively. P < 0.05 at two tails was considered statistically significant.
Results
In this pilot study, a total of 92 subjects with a mean age of 44.04 ± 12.68 years (range, 25–69 years) were enrolled. The mean SER of this sample was −1.86 ± 2.91D (range, −8.00–3.00D) and 48 (52.17%) subjects were female. There was no significant difference in age (45.38 ± 13.76 years vs. 42.59 ± 11.37 years, respectively. P = 0.295) and SER (−1.47 ± 2.82D vs. −2.28 ± 2.97D, respectively. P = 0.184) between women and men. A hyperopic shift of SER was found as age increased in the three stratified age groups (−3.24 ± 2.88D vs. −1.24 ± 2.64D vs. 0.39 ± 1.42D, respectively. P < 0.001) and age was progressively older as SER increased in the four refractive groups (56.87 ± 8.64years vs. 47.54 ± 11.10 years vs. 40.39 ± 12.18 years vs. 34.87 ± 7.28 years, respectively. P < 0.001).
Table 1 summarizes the means of BCDVA, BCNVA, UNVA, SCNVA, AULCSF and cut-off SF in the whole study population according to gender, age and type of refractive error. There was no significant difference in BCDVA, BCNVA, UNVA, SCNVA, AULCSF or cut-off SF between men and women (all P > 0.05). Among the stratified age groups, no significant difference in BCDVA, UNVA and AULCSF were found (all P > 0.05), but the BCNVA (P = 0.014), SCNVA (P < 0.001) and cut-off SF (P = 0.032) gradually decreased with increasing age. There was no significant difference in BCDVA (P = 0.301) and AULCSF (P = 0.560) among different refractive status, but the BCNVA and UNVA were better in the emmetropia and myopia groups than that in hyperopia and high myopia groups (all P < 0.05). For hyperopia, the SCNVA and cut-off SF was significantly reduced compared to the other refractive statuses (all P < 0.05).
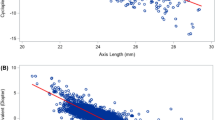
The mean CS values (log units) in spatial frequencies of 1.5, 3, 6, 12 and 18 cpd were 30.03 ± 11.43, 34.51 ± 11.85, 16.77 ± 9.70, 4.59 ± 3.31 and 1.71 ± 1.11, respectively. Comparison of levels of spatial frequency data revealed no statistically significant difference between women and men. As shown in Fig. 1, older subjects seemed to have a lower CS at each spatial frequency. As shown in Fig. 2, CS appeared reduced in hyperopic subjects.
Relationship of age, refractive errors, VA and CSF
As shown in Table 2, AULCSF and cutoff SF exhibited statistically significant association with age, BCNVA and SCNVA, but no significant associations were found between AULCSF and cutoff SF with gender, SER, BCDVA and UNVA. The multiple linear regression model demonstrated that SCNVA significantly contributed to AULCSF (standardized β = −0.24, P = 0.023) after adjustment for SER, gender, age and the other types of VA, and age significantly contributed to cut-off SF (standardized β = −0.29, P = 0.005) after adjustment for the other observed factors.
Relationship of age, SER, VA and CSF by type of refractive errors
For emmetropia (age, range 28–68 years), AULCSF had a statistically significant association with SCNVA (r = −0.39, P = 0.048), and cut-off SF had a statistically significant association with SCNVA (r = −0.40, P = 0.044) and age (r = −0.45, P = 0.020). After adjustment for age, cut-off SF had no statistically significant association with SCNVA (r = −0.22, P = 0.284).
For L&M myopia (age, range 25–67 years), AULCSF had a statistically significant association with DSNVA (r = −0.40, P = 0.015) and BCNVA (r = −0.52, P = 0.001), and cut-off SF had a statistically significant association with BCNVA (r = −0.48, P = 0.003).
For hyperopia (age, range 38–69 years) and high myopia (age, range 26 to 51 years), no significant association were found between AULCSF and cut-off SF with age, SER, and type of VA. The subjective refraction, which was performed to determine VA at near through optimal refractive correction, was significantly correlated to AULCSF in hyperopic subjects after adjustment for age (r = 0.66, P = 0.008).
Discussion
The current study showed that CSF significantly decreased with age at each spatial frequency in subjects across the life span (20–70 years of age) even though the BCDVA of these subjects was normal. The univariable and multivariable analyses demonstrated that age and the accompanied ability of near VA were significantly correlated to CSF after adjustment for gender and SER. Of the enrolled subjects, cut-off SF was likely reduced in hyperopia compared to the other refractive statuses, but no significant association was found between cut-off SF and refractive error after adjusting for age. For the treatment of functional presbyopia, the subjective refraction determining VA at near significantly correlated to AULCSF in hyperopic subjects. The current study is the first study to evaluate the potential effects of gender, age and refractive status on CSF using the quick CSF method, which promotes a better understanding of visual function in normal healthy adults and helps discover deficits in visual function in subjects with normal BCDVA.
The CSF, which describes visual sensitivity to narrow-band stimuli of a wide range of spatial frequencies, provides the ability to detect and interpret details of a visual scene in the real world [8, 9]. CSF appeared more sensitive in characterizing spatial vision deficits than letter acuity because patients may have CSF deficits even when their acuity looks normal [24]. This phenomenon was also found in the current study that the cut-off SF progressively decreased with increasing age in the sample age groups despite a normal BCDVA. The AULCSF showed a decreasing trend with increasing age increased though the statistical difference was not significant, which may result from the relatively small sample size. Among the different refractive statuses, AULCSF and cut-off SF seemed reduced in the hyperopia group when the BCDVA was normal.
Age influenced contrast sensitivity in many studies that found a generally lower CSF in older populations [25,26,27,28]. The refractive error may also affect CSF, but the reports are inconsistent between studies [25, 26, 29]. Hashemi et al. [25] found a lower CS values in myopes than hyperopes whereas Zocher et al. [26] demonstrated lower CS values in hyperopes than myopes. Xu et al. found no significant difference in CSF between myopes and emmetropes [29]. However, it should be noticed that in line with previous studies [26, 30, 31], the demographic data of the sample population in the present study, which may be influenced by population aging and myopia burst, demonstrated a hyperopic shift in the older age groups that resulted in more emmetropic or hyperopic eyes in older subjects. It is reasonable to speculate that the significant relationship of age and refractive error may cause a false correlation between CSF and refractive error. To distinguish the exact effect of age and refractive error on CSF, we performed univariable and multivariable correlation analyses which showed a significant correlation between age with CSF and no correlation between SER with CSF. Therefore, in consistent with Zocher et al.’s opinion [26], age rather than hyperopia may be the predominant factor for the lower CSF in hyperopic eyes than eyes with the other refractive statuses since hyperopia increased with age in the current study. However, it is hard to draw a conclusion that the refractive error had no effect on CSF in eyes with normal BCDVA, since their correlation may not be linear, which could not be determined using the simple and multiple linear regression analyses in the current study. Further prospective studies comparing CSF in different refractive status of normal eyes with age-matched subjects are warranted.
The epidemiological report that the prevalence of refractive visual impairment significantly increased with age, and uncorrected refractive error has been the leading cause of visual impairment in adults over the age of 40 years [32] indicates the important role of near visual assessment of adults in clinical practice. It also suggests that many subjects may only have one pair of corrective spectacles for one distance, especially in developing nations, such as China. To evaluate the whole visual performance, the near vision under correction of distance spectacles which reflects the daily visual status was also measured in addition to BCDVA, BCNVA and UNVA in the present study. We found that for eyes with normal BCDVA, SCNVA significantly contributed to AULCSF after adjusting for SER, gender, age and the other types of VA. This correlation was relatively higher in emmetropic and myopic eyes, which suggested that a low near vision with habitual spectacle may be associated with a deficit of CSF, especially for emmetropes and myopes, after excluding potential anatomical factors, such as abnormalities of the cornea, crystalline lens and fundus. This indication is meaningful for clinical practice, and suggests that CSF be measured when the DSNVA is low in eyes with normal BCDVA because the CSF measurement, which takes more time and is more complicated than the assessment of SCNVA, is not needed for every visiting patient.
Another interesting finding is that subjective refraction determining the near VA was significantly correlated to AULCSF in hyperopic subjects after adjustment for age. It is confirmed that near corrective refraction was associated with refractive error, but we found no significant correlation between SER with CSF. Previous studies reported the potential relationship of accommodation and CSF [33, 34], and near corrective refraction reflects the accommodation ability to some extent, which we speculated may be a potential factor for this finding. The results of our study suggested that an exceptionally high corrective spectacle prescription for presbyopia caused some deficits in CSF. However, this hypothesis must be verified in future studies with large sample sizes and more control of potential factors such as refractive error and age, since only 15 eyes were presbyopic in the present study.
One limitation of this study is the relatively small sample size, but as a pilot study, it provides the basis for a larger more definitive study. Another limitation of this study is that we could not further identify the underlying factors that caused the reduction in CSF since we only measured psychophysical vision which will be influenced by both optical and neural factors [35, 36]. Further studies combining objective and psychophysical tests with large sample size are warranted.
In conclusion, our study presented the distribution of visual functions, including CSF and types of VA, and verified their relationship with age and refractive error in healthy Chinese adult population. Although the BCDVA looks similar to normal, the CSF may significantly decreased with age, which is associated with the age-related reduction in near VA and may be independent of refractive error. Hyperopes with an exceptionally high subjective refraction that is needed to determine VA at near may have a reduced CSF which should cause notice when a prescription of add power is made for presbyopia. More studies are needed to establish an up-to-date reference of the candidate population that need CSF assessment, especially for those whose BCDVA is normal but with significant visual complaints.
Summary
What was known before
-
Population aging and increasing prevalence of myopia are two main changes over the last decades. Degeneration of near visual function is one of the main causes of visual impairment for older patients, but only the accommodation ability and conventional near vision testing may be insufficient to evaluate the daily near visual performance, since various possible factors, such as reduction in contrast sensitivity function (CSF), papillary size and increasing density of the crystalline lens etc., can degrade the near visual function with aging rather than age-related loss of accommodation. It has been reported that a variety of ophthalmic and neurologic conditions may cause CSF deficits which did not depend on patient’s overall level of visual deficits, such as dry eye, ocular hypertension and myopia etc. The potential inconsistency between VA and CSF deficits suggests that measuring the full CSF over a wide range of frequencies is clinically important. Methods of conventional CSF test, which are time-consuming (30–60 min), are not so suitable in clinical practice. Recently, Lesmes et al. developed a novel adaptive psychophysical procedure, the quick CSF (qCSF), which directly estimates the entire CSF curve rapidly (5–10 min) with reasonable precision. Researches on CSF assessment of diseases states, such as amblyopia, diabetic retinopathy and multiple sclerosis, using this novel method have been reported, but the candidate patients for normal population are still needed to explore. To the best of our knowledge, the effect of demographic changes in the last decades, such as aging and increasing prevalence of myopia, on visual functions for normal East Asian population remains unclear.
What this study adds
-
Our study presented the distribution of visual function, including CSF and types of VA, and verified their relationship with age and refractive error in healthy Chinese adult population. Even though the BCDVA looks like normal, the psychological vision, such as CSF can significantly decreased as age increases which is associated with the age-related reduction in near VA and may be independent of refractive error. Hyperopes with an exceptionally high subjective refraction needed to determine VA at near may have a reduced CSF which should cause notice when a prescription of add power is made for presbyopia. More studies are needed to establish up-to-date reference of candidate population needing CSF assessment, especially for those whose BCDVA is normal but with significant visual complaints.
References
Koretz JF, Kaufman PL, Neider MW, Goeckner PA. Accommodation and presbyopia in the human eye-aging of the anterior segment. Vis Res. 1989;29:1685–92.
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–42.
Rudnicka AR, Kapetanakis VV, Wathern AK, Logan NS, Gilmartin B, Whincup PH, et al. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol. 2016;100:882–90.
Nirmalan PK, Krishnaiah S, Shamanna BR, Rao GN, Thomas R. A population-based assessment of presbyopia in the state of Andhra Pradesh, south India: the Andhra Pradesh Eye Disease Study. Invest Ophthalmol Vis Sci. 2006;47:2324–8.
Owsley C. Vision aging. Annu Rev Vis Sci. 2016;2:255–71.
Birren JE, Casperson RC, Botwinick J. Age changes in pupil size. J Gerontol. 1950;5:216–21.
Cook CA, Koretz JF, Pfahnl A, Hyun J, Kaufman PL. Aging of the human crystalline lens and anterior segment. Vis Res. 1994;34:2945–54.
Marmor MF. Contrast sensitivity versus visual acuity in retinal disease. Br J Ophthalmol. 1986;70:553–9.
Arden GB. The importance of measuring contrast sensitivity in cases of visual disturbance. Br J Ophthalmol. 1978;62:198–209.
Rolando M, Iester M, Macrí A, Calabria G. Low spatial-contrast sensitivity in dry eyes. Cornea. 1998;17:376–9.
Gandolfi SA, Cimino L, Sangermani C, Ungaro N, Mora P, Tardini MG. Improvement of spatial contrast sensitivity threshold after surgical reduction of intraocular pressure in unilateral high-tension glaucoma. Invest Ophthalmol Vis Sci. 2005;46:197–201.
Collins JW, Carney LG. Visual performance in high myopia. Curr Eye Res. 1990;9:217–23.
Lesmes LA, Lu ZL, Baek J, Albright TD. Bayesian adaptive estimation of the contrast sensitivity function: the quick CSF method. J Vis. 2010;10:17.1–21.
Hou F, Huang CB, Lesmes L, Feng LX, Tao L, Zhou YF, et al. qCSF in clinical application: efficient characterization and classification of contrast sensitivity functions in amblyopia. Invest Ophthalmol Vis Sci. 2010;51:5365–77.
Joltikov KA, de Castro VM, Davila JR, Anand R, Khan SM, Farbman N, et al. Multidimensional functional and structural evaluation reveals neuroretinal impairment in early diabetic retinopathy. Invest Ophthalmol Vis Sci. 2017;58:BIO277–BIO290.
Shandiz JH, Nourian A, Hossaini MB, Moghaddam HO, Yekta AA, Sharifzadeh L, et al. Contrast sensitivity versus visual evoked potentials in multiple sclerosis. J Ophthalmic Vis Res. 2010;5:175–81.
Brainard DH. The psychophysics toolbox. Spat Vis. 1997;10:433–6.
Pelli DG. The VideoToolbox software for visual psychophysics: transforming numbers into movies. Spat Vis. 1997;10:437–42.
Li X, Lu ZL, Xu P, Jin J, Zhou Y. Generating high gray-level resolution monochrome displays with conventional computer graphics cards and color monitors. J Neurosci Methods. 2003;130:9–18.
van Gaalen KW, Jansonius NM, Koopmans SA, Terwee T, Kooijman AC. Relationship between contrast sensitivity and spherical aberration: comparison of 7 contrast sensitivity tests with natural and artificial pupils in healthy eyes. J Cataract Refract Surg. 2009;35:47–56.
Oshika T, Okamoto C, Samejima T, Tokunaga T, Miyata K. Contrast sensitivity function and ocular higher-order wavefront aberrations in normal human eyes. Ophthalmology. 2006;113:1807–12.
Zhou Y, Huang C, Xu P, Tao L, Qiu Z, Li X, et al. Perceptual learning improves contrast sensitivity and visual acuity in adults with anisometropic amblyopia. Vis Res. 2006;46:739–50.
Huang C, Tao L, Zhou Y, Lu ZL. Treated amblyopes remain deficient in spatial vision: a contrast sensitivity and external noise study. Vis Res. 2007;47:22–34.
Plainis S, Anastasakis AG, Tsilimbaris MK. The value of contrast sensitivity in diagnosing central serous chorioretinopathy. Clin Exp Optom. 2007;90:296–8.
Hashemi H, Khabazkhoob M, Jafarzadehpur E, Emamian MH, Shariati M, Fotouhi A. Contrast sensitivity evaluation in a population-based study in Shahroud, Iran. Ophthalmology. 2012;119:541–6.
Zocher MT, Rozema JJ, Oertel N, Dawczynski J, Wiedemann P, Rauscher FG. Biometry and visual function of a healthy cohort in Leipzig, Germany. BMC Ophthalmol. 2016;16:79.
Bühren J, Terzi E, Bach M, Wesemann W, Kohnen T. Measuring contrast sensitivity under different lighting conditions: comparison of three tests. Optom Vis Sci. 2006;83:290–8.
Schefrin BE, Tregear SJ, Harvey LO, Werner JS. Senescent changes in scotopic contrast sensitivity. Vis Res. 1999;39:3728–36.
Xu J, Zheng Z, Drobe B, Jiang J, Chen H. The effects of spatial frequency on the accommodation responses of myopes and emmetropes under various detection demands. Vis Res. 2015;115:1–7.
Bertelsen G, Erke MG, von HT, Mathiesen EB, Peto T, Sjølie AK, et al. The Tromsø Eye Study: study design, methodology and results on visual acuity and refractive errors. Acta Ophthalmol. 2013;91:635–42.
Williams KM, Verhoeven VJ, Cumberland P, Bertelsen G, Wolfram C, Buitendijk GH, et al. Prevalence of refractive error in Europe: the European Eye Epidemiology (E(3)) Consortium. Eur J Epidemiol. 2015;30:305–15.
Naidoo KS, Leasher J, Bourne RR, Flaxman SR, Jonas JB, Keeffe J, et al. Global vision impairment and blindness due to uncorrected refractive error, 1990-2010. Optom Vis Sci. 2016;93:227–34.
Katada Y, Negishi K, Watanabe K, Shigeno Y, Saiki M, Torii H, et al. Functional visual acuity of early presbyopia. PLoS ONE. 2016;11:e0151094.
Lin HT, Chan HJ, Ho CW, Tai MC, Chen JT, Liang CM. Impact of hypoxic and mesopic environments on visual acuity, contrast sensitivity and accommodation in subjects with LASIK surgery and aircrew candidate. J Chin Med Assoc. 2018;81:998–1007.
Mutyala S, McDonald MB, Scheinblum KA, Ostrick MD, Brint SF, Thompson H. Contrast sensitivity evaluation after laser in situ keratomileusis. Ophthalmology. 2000;107:1864–7.
Elliott DB. Contrast sensitivity and glare testing. in WJ Benjamin, editor, Borish’s clinical refraction, Philadelphia, Pa, USA: WB Saunders; 1998, pp. 203–41.
Acknowledgements
This work was supported by Science and Technology Program of Guangzhou, China (grant no. 201803010111).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, Z., Hu, Y., Yu, H. et al. Effect of age and refractive error on quick contrast sensitivity function in Chinese adults: a pilot study. Eye 35, 966–972 (2021). https://doi.org/10.1038/s41433-020-1009-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-1009-7
This article is cited by
-
The Characteristics of Quick Contrast Sensitivity Function in Keratoconus and Its Correlation with Corneal Topography
Ophthalmology and Therapy (2023)
-
A novel quick contrast sensitivity function test in Chinese adults with myopia and its related parameters
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)