Abstract
Purpose
To determine if the presence or absence of retinal and choroidal folds on SD-OCT imaging can distinguish between mild papilloedema and pseudopapilledema.
Design
Cross-sectional cohort study
Methods
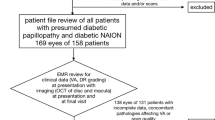
Subjects with optic disc elevation (Frisen grades 1 and 2 only) were eligible to be enrolled prospectively. Pseudopapilledema was defined as a lack of change in optic disc appearance between two visits <6 months apart, and papilloedema was defined as change in optic disc appearance between two visits <6 months apart determined by review of fundus photographs by a masked neuro-ophthalmologist. Three masked neuro-ophthalmologists independently reviewed en face and axial optical coherence tomography (OCT) images of the optic nerve of the study subjects for the presence or absence of retinal and choroidal folds. Concordance was determined when there was agreement between at least 2 of the 3 observers.
Results
Forty-five subjects (78 eyes) met inclusion criteria. There were 32 eyes with papilloedema and 46 eyes with pseudopapilledema. Choroidal and/or retinal folds were detected in 38% of eyes (12/32) with papilloedema and 19.6% of eyes (9/46) with pseudopapilledema. Post-hoc analyses eliminated six questionable cases of pseudopapilledema that had ancillary testing suggestive of elevated intracranial pressure and resulted in one remaining eye (2%) with more certain pseudopapilledema that was found to have folds. En face OCT imaging was more sensitive (71%) in detection of folds than axial OCT imaging (57%).
Conclusions
Choroidal and/or retinal folds on OCT are commonly observed in patients with mild papilloedema and are uncommon in those with pseudopapilledema. The presence of folds on OCT in patients presenting with disc elevation suggests papilloedema.
Similar content being viewed by others
Introduction
The differentiation between papilloedema versus pseudopapilledema remains a diagnostic dilemma when the optic disc elevation is mild and when signs and symptoms of raised intracranial pressure (ICP) are minimal. In these patients, ancillary test results such as signs of raised ICP on magnetic resonance imaging (MRI) and opening pressure measurements on lumbar puncture (LP) may be equivocal.
Retinal and choroidal folds have been observed in patients with papilloedema due to idiopathic intracranial hypertension (IIH) and are more frequently observed with higher grades of swelling [1,2,3]. Peripapillary wrinkles and outer retinal folds are more commonly seen with higher grades of papilloedema (Frisen grades 3–5), and choroidal folds are more commonly seen in patients with higher ICP [1, 4].
In 2015 spectral-domain optical coherence tomography (SD-OCT) was used to primarily investigate the frequency, types, and patterns of retinal and choroidal folds in patients with papilloedema who were enrolled in the IIH treatment trial (IIHTT) [1, 5]. Sibony et al. found that by OCT, choroidal and retinal folds were found in 73% of patients with papilloedema, and that OCT was more sensitive than fundus photographs in the detection of folds [1].
On the other hand, it is generally believed that folds are not a feature of pseudopapilledema and may, in fact, be pathognomonic of true papilloedema, although this has not been studied prospectively or in a masked fashion. Carta et al. looked at specific signs on fundoscopy to differentiate optic disc oedema from pseudopapilledema; however, this study was neither masked nor prospective, and OCT imaging was not utilized [6].
While pseudopapilledema follows a relatively benign course, true papilloedema requires timely evaluation including neuroimaging and LP. We sought to determine if the presence of retinal and choroidal folds can be a distinguishing feature between mild papilloedema versus pseudopapilledema by using both axial and en face SD-OCT imaging.
Materials and methods
A previous study from our institution prospectively enrolled patients with optic disc elevation [7]. Approval by the Institutional Review Board at University of Pennsylvania was obtained prior to the study. In the previous study, the sensitivity and specificity of ocular ultrasonography in papilloedema and pseudopapilledema were studied in patients presenting with optic nerve elevation [7]. By the study criteria, pseudopapilledema was defined as optic disc elevation with a lack of change in optic disc appearance between two visits <6 months apart, and papilloedema was defined as optic disc elevation with a change in optic disc appearance between two visits <6 months apart determined by review of fundus photographs by a masked neuro-ophthalmologist [7]. We utilized these same definitions for our study.
In our study, patients with Frisen grades 1 and 2 optic nerve elevation were included while grades 3–5 were excluded, since in higher grades of optic nerve swelling there is less ambiguity in differentiating between true papilloedema versus pseudopapilledema. In addition, all patients with visible optic disc drusen (ODD) were excluded. Patients with other causes of optic disc elevation (i.e., ischemic, compressive, inflammatory) based on clinical presentation and examination were excluded from the study.
Patients underwent standard work up including MRI and/or LP, as deemed necessary by the examining neuro-ophthalmologist. Findings suggestive of increased ICP on MRI included an empty sella, flattening of the posterior globes, optic nerve sheath distension and/or transverse sinus stenosis. An LP opening pressure of ≥25 cm H2O was considered elevated.
Digital fundus photography was performed by a technician using the IIHTT protocol [8]. The Zeiss FF450 camera was used with a 30-degree field angle. Photos were taken with a resolution of 2400 × 2048 pixels with this fundus camera combined with Merge Healthcare software and 5 megapixel backing camera.
The photographs were uploaded to a Windows 7 Professional SP1 PC and contained within the WinStation version 11.4 program provided by Merge Healthcare. The images were visualized under dim room illumination by a masked neuro-ophthalmologist. The photographs contained an image centered on the optic disc at the retinal plane, on the plane of highest disc elevation, as well as the papillomacular area. All photographs were included with the exception of those containing artifacts or capture errors.
All subjects were imaged on the same Cirrus 5000 SD-OCT (8.1.0.117) using the IIHTT OCT acquisition protocol [8]. Five types of scans were performed: two 200 × 200 optic disc cube scans, two macular cube scans 200 × 200 centred on the fovea, and one high definition (HD) five-line raster scan of the optic disc horizontally oriented and separated by 0.5 mm imposed on the disc. The cube scans were generated from a 6 mm square grid composed of 200 horizontal lines containing 200 A-scans.
Three masked neuro-ophthalmologists (PAS, RAA, MT) were instructed to identify retinal and choroidal folds using SD-OCT images as previously described by Sibony et al. [1]. Anonymized SD-OCT images (en face and axial images, separately) were presented in random order to each masked evaluator who individually evaluated each image for the presence or absence of folds. For the axial images, five raster images were grouped together for each eye (Fig. 1a). Only one en face image was used for each eye (Fig. 1b). Concordance was determined when there was agreement among at least 2 of the 3 reviewers. Results were collected and recorded by an unmasked evaluator (SNR).
Pairwise agreement between the graders viewing en face and axial OCT images was assessed using kappa statistics. Sensitivity and specificity were calculated, and logistic regression with generalized estimating equations to account for the correlation between eyes in the same person was used to construct 95% confidence intervals [9]. All statistical computations were performed with SAS 9.4 (SAS Inc, Cary, NC).
Results
In the forty-five subjects (78 eyes) who met inclusion criteria, 32 eyes had papilloedema (Frisen grade 1 or 2), and 46 eyes had pseudopapilledema. Thirty-eight subjects (92.6%) were female. Pairwise agreement between the three evaluators using kappa statistics ranged from 0.65 to 0.80 for en face OCT images and ranged from 0.16 to 0.45 for axial OCT images.
Retinal and choroidal folds were detected in 38% of eyes with papilloedema (12/32) and in 19.6% of eyes with pseudopapilledema (9/46) based on the aforementioned definitions of papilloedema and pseudopapilledema. There were three eyes from two patients that had buried ODD confirmed with B scan ultrasonography. None of these three eyes had folds.
Based upon review of the en face OCT images, folds were observed in 10 out of 32 eyes with papilloedema (sensitivity 31% [95% confidence interval 16, 53%]; p = 0.09) and 6 out of 46 eyes with pseudopapilledema (specificity 87% [69–95%]; p < 0.001).
Based upon review of the axial OCT images of the 5-line raster scan, folds were observed in 8 of 32 eyes with papilloedema (sensitivity 25% [12–45%]; p = 0.02) and in 6 of 46 eyes with pseudopapilledema (specificity 87% [75–94%]; p < 0.001). Eight eyes had folds on both en face and axial OCT imaging (six true papilloedema and two pseudopapilledema).
A post-hoc review of the medical records of the seven patients (nine eyes) with pseudopapilledema noted to have folds was performed. Six of the seven patients had at least one ancillary test result suggestive of elevated ICP which included one or more of the following: LP opening pressure >25 cm of H20, an empty sella visualized on brain MRI, abnormal optic nerve sheath fluid on B scan ultrasound, or a greater than 10-micron change between initial and follow-up OCT peripapillary RNFL thickness.
After excluding these six patients, there was one patient (#1) who had peripapillary wrinkles and no suggestion of true elevated ICP or papilloedema on ancillary testing. (Table 1 and Fig. 2a, b).
There were 28 patients (52 eyes) from both the papilloedema and pseudopapilledema groups that had signs of elevated ICP: LP opening pressure >25 cm of H20 empty sella visualized on brain MRI, positive optic nerve sheath fluid on B scan ultrasound, or a >10-micron change between initial and follow-up OCT peripapillary RNFL thickness. Of these patients with suspected elevated ICP, 25% (13 eyes) had folds on en face OCT imaging (p value = 0.01) and 21% (11 eyes) had folds on axial OCT imaging (p value < 0.001).
Discussion
Retinal and choroidal folds, originally described by Nettleship in 1884 [10], are seen in many ophthalmic conditions, such as hyperopia, ocular hypotony, uveitis, orbital tumors, scleral buckles, epiretinal membranes, maculopathies, and papilloedema [1, 11,12,13,14]. Elevated ICP can be accompanied by a corresponding increase in the cerebrospinal fluid pressure within the optic nerve sheaths [15]. The increased pressure within the sheath can in turn be transmitted directly to the globe, causing flattening of the sclera and subsequent formation of choroidal and/or retinal folds [1,2,3, 6, 11].
Four types of folds have been described in papilloedema: peripapillary wrinkles (similar to previously described “Paton’s lines”), inner retinal folds, outer retinal folds, and choroidal folds [1, 4]. In our study, retinal and/or choroidal folds were observed in 38% of those with mild papilloedema (Frisen grades 1 and 2) using SD-OCT. Our lower number compared to the 73% in the IIHTT is likely due to inclusion of only Frisen grades 1 and 2 of papilloedema in our study, while the IIHTT considered all grades of papilloedema [5, 8]. Based on an unpublished sub-analysis of the IIHTT data (by PS), 57/125 patients in the IIHTT cohort had grade I or II papilloedema. Nineteen of those 57 (33%) had peripapillary wrinkles on OCT imaging, similar to our findings.
We acknowledge that the criteria utilized for this study (i.e., a change in optic disc swelling between initial and follow-up visits) is not a perfect method to diagnose papilloedema. A change in lower grades of disc swelling may not occur, and/or mild papilloedema may not change in the 6 months follow-up interval that was set for the study purposes. Some patients who had an undetectable change in disc swelling could have been misclassified as having pseudopapilledema, especially when high opening pressure on LP and MRI signs of raised ICP were also observed in some subjects in the pseudopapilledema group. In addition, discrete changes in RNFL thickness are easily missed using fundus photos alone without the use of OCT analysis.
We chose a definition of papilloedema based on the appearance of the optic disc alone, which is often the defining exam feature, without the possible bias and often inconclusive results of other ancillary testing. Examiner bias was minimized by choosing three neuro-ophthalmologists, separate from the original treating neuro-ophthalmologist, to review the OCT images. We acknowledge that there can be inherent variability in interpretation of optic disc oedema, even by experienced neuro-ophthalmologists [7].
There have been limited studies looking for the presence of folds in pseudopapilledema. Carta et al. performed an observational study to assess the accuracy, sensitivity, and specificity of fundoscopy in differentiating between pseudopapilledema and true papilloedema. They found that the presence of retinal and choroidal folds appeared to be pathognomonic for true optic disc oedema; however, OCT imaging was not used to detect the folds in this study. In addition, although sensitivity was 100%, folds were only found in 23% of patients with true optic disc oedema [6].
While patients with visible surface ODD had previously been excluded from our cohort, there were 3 of 46 eyes (6.5%) of patients with pseudopapilledema who had buried ODD confirmed on B scan ultrasonography. A recent study has shown that folds may be present in up to 13% of patients with ODD; however, the majority of those patients had coexistent papilloedema or non-arteritic anterior ischemic optic neuropathy [16]. Two patients in this cohort had folds with ODD, and the authors surmised that perhaps these two patients likely had prior papilloedema or anterior ischemic optic neuropathy [16]. In our cohort, there was a single patient with pseudopapilledema who had folds. Therefore it is conceivable that she may have had previous papilloedema or previous anterior ischemic optic neuropathy unbeknownst to the authors, especially since folds can remain long after disc swelling resolves [17].
Numerous investigators have utilized circumpapillary RNFL thickness and peripapillary total retinal volume on OCT imaging in an attempt to distinguish between papilloedema and pseudopapilledema, all producing different results [18,19,20]. Fard et al. reported that while both papilloedema and pseudopapilledema have a statistically significant thicker circumpapillary RNFL thickness than normal subjects, the average outer peripapillary total retinal volume was greater in papilloedema versus pseudopapilledema [19]. In contrast, there have been studies which found that OCT cannot clearly differentiate between individuals with mild papilloedema and those with congenitally crowded discs [21]. Other studies have stated that OCT can be used to differentiate between true papilloedema, pseudopapilledema and normal eyes when the nasal RNFL quadrant is analyzed [18]. It is worth noting that previous studies evaluating OCT imaging for retinal and choroidal folds were not masked, and observers already had knowledge of the subjects’ diagnosis of papilloedema.
In our study, agreement among reviewers was relatively high with en face imaging (0.65–0.80 pairwise agreement) versus axial imaging (0.16–0.45 pairwise agreement), suggesting en face may be a more reliable imaging modality for observing folds. This may be due to a greater amount of artifact observed with axial imaging due to retinal vasculature.
We found that folds were present in 38% of eyes with true papilloedema in our cohort with lower grades of disc swelling (Frisen grades 1 and 2). After excluding subjects initially diagnosed with pseudopapilledema but then having at least one ancillary test suspicious of raised ICP, one eye from one patient remained who may have had true pseudopapilledema and folds detected on OCT. Thus, the presence of folds in pseudopapilledema appears to be uncommon. It is important to remember that MRI signs of raised ICP and borderline elevated opening pressure on LP are not in and of themselves diagnostic of clinically significant ICP. For the purposes of this study, we excluded patients from the pseudopapilledema group that had one or more positive ancillary test results in order to completely eliminate the possibility of such patients having true papilloedema. This underscores the need to have more stringent definitions, which are currently lacking, of papilloedema versus pseudopapilledema.
Upon review of all patients in our cohort that demonstrated signs of raised ICP on ancillary testing (28/52), 46% had folds observed on SD-OCT in one or both eyes. Therefore, in subjects with mild grades of disc elevation, the presence of folds seen on OCT, along with signs of raised ICP, may help to provide yet another data set to help make the diagnosis of papilloedema. When analyzing folds in this patient population, there was an 87% specificity of folds in both the axial and the en face group.
In conclusion, while the absence of retinal and choroidal folds on OCT may not help to distinguish between papilloedema and pseudopapilledema, their appearance in patients with a mild degree of optic nerve elevation suggests papilloedema. Future studies will need to determine more stringent definitions of pseudopapilledema and true papilloedema in order to ascertain if the presence of folds on OCT are indeed unique to patients with papilloedema.
Summary
What was known before
-
Retinal and choroidal folds identified on OCT are associated with papilloedema but have never been evaluated in pseudopapilledema in a masked fashion.
What this study adds
-
Retinal and choroidal folds identified on OCT can help distinguish between mild papilloedema and pseudopapilledema.
References
Sibony PA, Kupersmith MJ, Feldon SE, Wang JK, Garvin M. Retinal and choroidal folds in papilledema. Investig Ophthalmol Vis Sci. 2015;56(Sep):5670–80.
Griebel SR, Kosmorsky GS. Choroidal folds associated with increased intracranial pressure. Am J Ophthalmol. 2000;129(Apr):513–6.
Jacobson DM. Intracranial Hypertension and the Syndrome of Acquired Hyperopia with Choroidal Folds. J Neuroophthalmol. 1995;15(Sep):178–85.
Sibony PA, Kupersmith MJ. Patons folds revisited: raster and en face OCT of peripapillary wrinkles, folds, and creases. Ophthalmol. 2016;123:1397–9.
Smith SV, Friedman DI. (2017). The Idiopathic Intracranial Hypertension Treatment Trial: a Review of the Outcomes. Headache. 2017;57(Sep):1303–10.
Carta A, Favilla S, Prato M, Bianchi-Marzoli S, Sadun AA, Mora P. Accuracy of Funduscopy to identify true Edema versus Pseudoedema of the optic disc. Investig Ophthalmol Vis Sci. 2012;53(Jan):1–6.
Kohli, AA, Pistilli, M, Cruz, CA, Ross AG, Jivraj I, Bagchi S et al. The role of ocular ultrasonography to distinguish papilledema from pseudopapilledema. J Neuroophthalmol. 2020. https://doi.org/10.1097/WNO.0000000000000984. Online ahead of print.
Wall M, McDermott MP, Kieburtz KD, Corbet JJ, Feldon SE, Friedman DI, et al. Effect of acetazolamide on visual function in patients with idiopathic intracranial hypertension and mild visual loss: the idiopathic intracranial hypertension treatment trial. JAMA. 2014;31(Apr):1641–51.
Zeger SL, Liang K-Y. Longitudinal Data Analysis for Discrete and Continuous Outcomes. Biometrics. 1986;42(Mar):121–30.
Nettleship E. Peculiar lines in the choroid in a case of postpapillitic atrophy. Trans Ophthalmol Soc U K. 1884;4:167–71.
Bird AC, Sanders MD. Choroidal folds in association with papilloedema. Br J Ophthalmol.1973;57(Feb):89–97.
Bullock JD, Egbert PR. The origin of choroidal folds a clinical, histopathological, and experimental study. Doc Ophthalmol. 1974;37(Nov):261–93.
Friberg TR. The etiology of choroidal folds - A biomechanical explanation. Graefes Arch Clinl Expl Ophthalmol. 1989;227:459–64.
Mader TH, Gibson CR, Pass AF, Kramer LA, Lee AG, Fogarty J, et al. Optic disc edema, globe flattening, choroidal folds, and hyperopic shifts observed in astronauts after long-duration space flight. Ophthalmol. 2011;118(Oct):2058–69.
Paton L. Papilledema and optic neuritis. Can Med Assoc J. 1936;34(May):555–63.
Abazari A and Sibony PA. The etiology of retinal and choroidal folds in optic disc drusen (ODD). Ophthalmol. 2020. https://doi.org/10.1016/j.ophtha.2020.05.022. Online ahead of print.
Kupersmith MJ, Sibony PA, Feldon SE, Wang JK, Garvin M, Kardon R. The effect of treatment of idiopathic intracranial hypertension on prevalence of retinal and choroidal folds. Am J Ophthalmol. 2017;176:77–86.
Bassi S, Mohana K. Optical coherence tomography in papilledema and pseudopapilledema with and without optic nerve head drusen. Indian J Ophthalmol. 2014;62(Dec):1146–51.
Fard MA, Fakhree S, Abdi P, Hassanpoor N, Subramanian PS. Quantification of peripapillary total retinal volume in pseudopapilledema and mild papilledema using spectral-domain optical coherence tomography. Am J Ophthalmol. 2014;158(Jul):136–43.
Kardon R. Optical coherence tomography in papilledema: what am i missing? J Neuroophthalmol. 2014;34(Sep):S10–7. Suppl
Karam EZ, Hedges TR. Optical coherence tomography of the retinal nerve fibre layer in mild papilloedema and pseudopapilloedema. Br J Ophthalmol. 2005;89(Mar):94–8.
Author information
Authors and Affiliations
Contributions
SNR was responsible for designing the review protocol, writing the protocol and report, extracting and analyzing data, interpreting results, and writing the paper. RAA was responsible for reviewing images in a masked fashion, interpreting results, and editing the paper. JCB was responsible for designing the review protocol and editing the paper. IJ was responsible for designing the review protocol and editing the paper. CA was responsible for designing the review protocol and editing the paper. MP was responsible for analyzing data and producing statistics for the paper. AAK was responsible for designing the review protocol and editing the paper. GTL was responsible for designing the review protocol, interpreting results and editing the paper. KSS was responsible for designing the review protocol, interpreting results, and editing the paper. AGR was responsible for designing the review protocol, interpreting results, and editing the paper. RHK was responsible for designing the review protocol, interpreting results, and editing the paper. PAS was responsible for designing the review protocol, interpreting results, and editing the paper. MT was responsible for designing the review protocol, reviewing images in a masked fashion, writing the protocol and report, extracting and analyzing data, interpreting results, and editing the paper.
Corresponding author
Ethics declarations
Conflict of interest
Author RHK receives an unrestricted grant for OCT research funded by Heidelberg Engineering, although this was not utilized in his involvement of this manuscript. No other authors have any conflicts of interest related to this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Reggie, S.N., Avery, R.A., Bavinger, J.C. et al. The sensitivity and specificity of retinal and choroidal folds to distinguish between mild papilloedema and pseudopapilledema. Eye 35, 3131–3136 (2021). https://doi.org/10.1038/s41433-020-01368-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01368-y
This article is cited by
-
Chorioretinal abnormalities in idiopathic intracranial hypertension: case reports
International Journal of Retina and Vitreous (2022)