Abstract
Background/Objectives
Patients undergoing intravitreal injections for nAMD are often anxious about early detection of nAMD in their fellow eyes. The purpose of this study was to evaluate a home-based telephone method for helping patients to monitor for symptoms of second eye involvement.
Subjects/Methods
Using a five-staged evaluation tool, telephone-assisted evaluations were repeatedly performed on the patients’ fellow eyes every 4 weeks for 1 year. A decision on presence or absence of nAMD was made after each telephone evaluation. Slitlamp examination and OCT scan were performed at 3, 6, 9 and 12 months or whenever nAMD was suspected from the telephone evaluation. The sensitivity and specificity values were calculated from the true and false positive and negative rates of each of the five composite stages.
Results
In total, 514 telephone episodes comprising 2570 evaluations were conducted on fellow eyes of 50 patients over one year. Three patients (6%) developed nAMD in fellow eyes. The sensitivity of all of the stages was low (33.3%). The specificity of the five stages ranged from 91.3% to 98.6%. The highest specificity was achieved by the near acuity component of the tool.
Conclusions
We were unable to demonstrate a high sensitivity for the five-staged tool but the near acuity component of this tool had a very high specificity. This could have potential for “ruling out” nAMD and reducing the burden of false positive episodes for a large group of patients who are at risk of developing nAMD in their second eyes.
Similar content being viewed by others
Introduction
Neovascular Age Related Macular Degeneration (nAMD) is a major cause of vision loss [1]. The era of intravitreal therapy has significantly reduced the burden of severe visual loss as evidenced by data from multiple countries showing a reduction in the incidence of legal blindness in recent years [2,3,4,5]. Despite treatment, however, significant numbers of patients still suffer moderate visual loss overtime as well as loss of functional skills such as reading ability, ability to drive or other daily activities [6]. This can be associated with a reduction in quality of life and depression [7, 8].
nAMD often occurs in one eye initially but there is an estimated 10–12% risk of second eye involvement every year, with some studies suggesting over 50% involvement over 3–5 years [9,10,11,12]. The onset of second eye involvement is often a devastating blow for the patient not only because of the need for bilateral intravitreal injections and more frequent hospital visits, but also the prospect of severe visual loss in both eyes and reduction in quality of life.
Numerous studies have shown that early detection and intervention with intravitreal therapies is associated with a better final visual acuity [11, 13,14,15,16]. More recently, studies using Optical Coherence Tomography Angiography have shown the presence of latent, occult choroidal neovascularisation (CNV) which may cause more subtle symptoms and be more difficult for patients to monitor [17, 18]. The emergence of longer acting agents and longer intervals between hospital visits may increase the risk of missing early activity in the fellow eye. Recent recommendations suggest examination of fellow eye every 3–4 months, including OCT assessments, with self-monitoring at home in between visits [19]. There is an unmet need for effective home monitoring for early symptoms of nAMD especially for second eyes of patients with unilateral nAMD.
Methods for self-detection of nAMD have been evaluated by several, however, no gold standard exists [20,21,22,23,24]. We report the findings of a pilot study which evaluated the usefulness of a 5 component telephone evaluation method for detecting the presence or absence of nAMD in the second eyes of patients undergoing therapy for nAMD in their first eyes.
Methods
Prior approval from our local ethics committee was obtained for this single centre, prospective study. Patients attending regular visits for treatment of unilateral nAMD were given an information sheet and invited to participate. Patients had to have reduced vision in one eye due to nAMD but better vision in the fellow eye which had not been affected by nAMD (study eye). After written, informed consent was obtained from each participant; their eligibility was determined by evaluating both eyes using LogMAR ETDRS charts (distance acuity), Bailey-Lovie reading charts (near acuity), dilated slit-lamp examination, OCT scan and fundus fluorescein angiography.
For this pilot study design, the established second eye conversion rate of 10% per year was expected and a sample size of 50 patients was used to yield about 5 conversions in 12 months of prospective follow up. During the study, patients were contacted by telephone every 4 weeks to determine if they had symptoms of CNV in their study eyes. They also attended hospital for examination and OCT scan every 3 months. To reduce the burden of visits for patients, the study eye visits were scheduled to coincide with fellow eye visits whenever possible as the majority of patients still had frequent visits for their first (fellow) eyes on a treat and extend or PRN regimen. Telephone consultations continue independently of the scheduled hospital visits. Any suspicion of nAMD in the second eye from a telephone enquiry or a hospital visit would trigger an OCT scan with or without another fluorescein angiogram to determine the presence or absence of second eye involvement in the study eye. Patients with nAMD in their second eyes, diagnosed during the study, would exit from the study and immediately transferred to our hospital macular service for treatment of their first and second eyes with bilateral intravitreal anti-VEGF injections.
A standard five component evaluation was used for each telephone contact to determine if patients had symptoms of nAMD in their study eye. The first three stages were history based and involved asking the following questions: (1) Have you experienced any symptoms of increased blurring of vision recently?, (2) Have you experienced any symptoms of increased difficulty with reading recently?, (3) Have you experienced any symptoms of increased distortion recently? An affirmative response to any of these three questions would trigger a hospital visit.
The fourth component was the Amsler chart test with the patient seated at a table or desk, the nonstudy eye covered with a patch and using their habitual reading spectacles with a reading lamp. They were then asked if they were aware of any new distortion whilst looking at the centre spot on the Amsler grid. Any existing distortion was described by the patient and documented on a mark sheet by the interviewer for future reference. To determine whether distortion was new or pre-existing during a telephone call, the patient was asked to mark the area of distortion and to locate the area of any distortion by counting the squares from the vertical and horizontal edges. If distortion was present, the patient would describe the location and size of the distorted area by number of squares so that this could be documented on the Amsler chart in the clinical record form. This enabled the examiner to remind the patient what they had described the previous month and to compare for any potential change. Any new distortion would trigger a hospital check-up.
The fifth component was a quantitative reading test administered by the patients themselves, immediately following the Amsler test, using the same reading spectacles and the patch over the nonstudy eye, and using an A4 modified Bailey-Lovie reading test designed specifically for the study. The reading test design composed of three paragraphs of random text composed of a combination of four, seven, and ten letter words taken from the oxford concise dictionary. The font size of the reading test was individually tailored to the patient based on the near visual acuity of their study eye as measured using the Bailey-Lovie word reading chart at screening. The modified reading test composed of one paragraph in the font size of their near acuity as well as one paragraph in 0.1 LogMAR (VAR) larger font and one in 0.1 LogMAR (VAR) smaller font. These measurements were based on a testing distance of 25 cm to enable them to be converted from LogMAR (VAR) to point sizes between N4 and N80. Line spacing was fixed to match the size of the font to reduce any variability caused by crowding. Responses were scored out of ten for each font size and this was documented by the interviewer along with the best corrected near visual acuity in N point. Any drop in the near visual acuity of >10 words (equivalent to 0.1 LogMAR (VAR) at 25 cm) triggered a hospital visit.
For the telephone evaluations, patients were issued with a screening pack including a copy of the Amsler grid and the modified Bailey-Lovie reading test charts. An example of the modified Bailey-Lovie reading chart is shown in Fig. 1. Patients were called within the first week of the first hospital baseline visit to run through the telephone evaluation and to establish baseline “at home” status. If the patient was unable to read at least ten words a larger reading test was sent out through the post and the home baseline test was repeated.
For the hospital visits at months 3, 6, 9 and 12, full ophthalmic examination and OCT scans were also performed to look for nAMD conversion.
Using this 5 component telephone evaluation for each episode of telephone contact, followed by hospital visits, outcomes of every telephone episode could therefore be evaluated from subsequent visits as either being true or false positive or negative. The primary outcomes for this study were the number of true and false positives and number of true and false negatives. Secondary analyses were done to explore the reasons for false positives or negatives.
Results
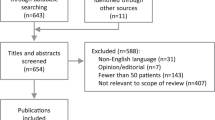
Case notes of 665 patients were reviewed and, from these, 206 were approached for screening and given a patient information sheet. Sixty two patients agreed to be screened but only the first 50 patients (mean age 79 years, 29 F) were recruited as this was the sample size that was proposed and approved by the ethics committee. At baseline, 100% of study eyes did not have nAMD and had mean distance acuity of 75.82 L (44–85) and mean near acuity of N6.1 (N4 to N20). At the final 12 month visit, the study eyes had mean distance acuity of 73.21 L (30–85). All the fellow eyes had received therapy for nAMD and had mean distance acuity 54.5 L (0–85) at baseline and a final mean distance acuity at 12 months of 52.0 L (0–85).
Out of a total of 50 patients, five withdrew before the end of the study (3 for personal reasons and 2 passed away) and three patients exited early due to development of CNV in the study eyes during the study period (annual conversion rate of 6%). Surprisingly, of these five patients who exited early, two developed nAMD after exiting the study. If these two patients had not withdrawn from the study, the annual conversion rate would have been the expected 10% instead of 6%. The other 47 patients did not develop CNV in their study eyes during the study. Data from all 50 patients for all telephone and hospital study visits were used for analysis. Out of a possible maximum of 600 telephone episodes comprising 3000 evaluations, only 514 telephone episodes comprising 2570 evaluation points were performed due to earlier departure of the eight patients. Of the 514 telephone episodes, only three coincided with the development of CNV (positive) and 511 episodes coincided with no development of CNV (negative).
With respect to the three telephone episodes of CNV development only one was a true positive (Fig. 2) and two were neither true positives nor false negatives as both patients missed the telephone episode prior to their hospital visits. Consequently, there was more than one month between their most recent telephone episodes and the hospital visits. Because both of these patients were completely asymptomatic, they were regarded as false negatives for the purpose of analysis.
With respect to the 511 episodes for which there was no development of CNV, 419 were true negatives and 92 were false positives. Table 1 shows the true and false positives and negatives of the 514 telephone episodes.
When the telephone episodes were broken down to individual component evaluations, the distribution of true positive and false negatives were similar across all five points for those episodes that coincided with CNV development. Of the 2750 evaluations, there were 149 positives and 2421 negatives. As one or more evaluation components could trigger a single positive telephone episode, the denominator for calculating sensitivity or specificity was the number of episodes (n = 3 or n = 511) and not evaluations (n = 149 or n = 2421). The sensitivity was therefore 33% for each of the five components. However, when the negative episodes were broken down to the individual component evaluations, the false positives ranged from 9.4 to 1.4%. The specificity was best at 98.6% with the self-administered reading acuity evaluation component (Table 2) i.e., the proportion of episodes without CNV development correctly identified as negative was 98.6% using the self-administered near acuity reading test compared to only 90.6% using the subjective response from asking a patient if they had any reading difficulty. Table 2 shows the true and false positive and negative rates and specificity of each of the five components from 2570 component evaluations captured over 514 telephone episodes.
Impact of visual acuity on false positive rates of telephone episodes
The 93 episodes when patients reported some symptoms led to 93 episodes of face to face reviews and 92 of these were false. Sub-dividing all 50 patients into three baseline visual acuity strata; Group A with <70 Letters (n = 9), Group B with 71 to 84 letters (n = 32) and Group C with 85 L (n = 9). Groups A, B and C completed 91, 423 and 120 telephone episodes respectively. The false positive rate in Group A was 22.0% (20/91). The false positive rate in Group B was 17.0% (71/423) and the false positive rate in Group C was 0.8% (1/120). The number of patients who had repeated false positives in Groups A, B and C were 77.8% (7/9), 53.7% (22/41) and 0% respectively. This shows that patients with good visual acuities were less likely to produce false positive responses.
Impact of visual acuity on false positive rates of evaluations components
Table 3 shows the distribution of false positive rates in all patients across the three visual strata for the five component evaluations. The group with the best visual acuity had the lowest false positive responses for all five evaluation components and in those groups with poorer vision, the near acuity reading test had much lower false positive rates. Notably, the Amsler chart had a high false positive rate in the groups with poorer vision (28.1–40%)
Discussion
The specificity value indicates the proportion of the patients who do not have the disease that are correctly identified with a negative test. Our results showed that the telephone method had quite a high specificity especially with the self-administered reading test component of the telephone evaluation. Although specificity was good, there was a high level of false positives. This means that the near acuity test could potentially be useful for ruling out the presence of nAMD if negative. We can estimate the confidence of the specificity result, using the tables from Bujang and Adnan and a prevalence rate of 5%. A sample size of 52 patients is needed to provide 80% power to test the Null hypothesis at a probability level of 5% [25]. Therefore, the specificity value of our test should be statistically significant with p value between 0.039 to 0.044. Our specificity result means that if the near acuity test administered to the second eye via a telephone call is negative, there is a 98.6% chance that the patient does not have CNV in the second eye.
The sensitivity value indicates the proportion of people correctly identified as having the disease when the test is positive. When evaluating a test to determine its sensitivity, it is necessary to have a sufficient sample size for the expected prevalence. There were only three instances in the study population when we could have detected CNV, which meant that the prevalence of second eye involvement in this cohort was very low. Again, using the tables provided by Bujang and Adnan we can estimate that a sample size of 980 patients would be required to provide 90% power of obtaining sensitivity values with 95% confidence intervals [25]. From our sample size of 50 patients it would have required 10 patients out of 50 (20% prevalence) to provide 80% power to test the Null hypothesis with a probability of 4%. Therefore, our study was severely underpowered to test the statistical significance of the sensitivity value, even if the two patients who developed CNV did not miss their telephone visits and could be classed as true positives and additionally even if the two patients who developed nAMD after exiting the study were included.
Therefore, unfortunately, in this pilot study we did not have sufficient power or prevalence to demonstrate a high sensitivity value of this test, so it cannot be used as screening tool to ‘rule in’ the diagnosis of CNV if the test is positive.
Many patients who have symptoms of blurring, distortion and difficulty reading seek frequent hospital visits for examination and imaging. The majority of these hospital visits turn out to be false alarms or false positives. Patients are usually reassured after having had an OCT scan in the hospital clinic, however, these false positives create an unnecessary burden to often already overloaded ophthalmology departments. In our study, although the telephone evaluation was reliable for ruling out nAMD if negative, there were a high number of false positives. Out of a total of 93 positive telephone episodes, 92 were false. There was a degree of overlap between the component evaluations in that a patient was only required to a positive response in one of the five component evaluations to be classed as a positive response. Table 2 shows the distribution of false positives across the five components of evaluations. The false positive rate for the near acuity component was very low at 1.4% or 7 false positives out of 511 evaluations. This component is, therefore, likely to lead to the least number of false alarms and unnecessary hospital visits. Furthermore, the false positive rates were the lowest in the stratum with best visual acuity. This correlates with findings from the Irish Longitudinal Study on Ageing, reported by Whillan and Nazroo, that found normal vision was identified well with a subjective response but that there was over-identification of visual impairment using subjective testing [26]. Thus, although subjective testing may well be useful in those with better visual acuity, this may not be the case in those with lower visual acuities.
In the setting of short term monitoring between hospital visits over intervals of 2–6 months, it is important to have a test that has a low rate of false positives to minimise the need for extra visits for hospital scans and the burden on patients, their relatives and carers as well as hospital resources. The Amsler chart test is known to have high sensitivity but low specificity and is popular with many patients because it is quick and easy to perform [20]. Although, in this study, Amsler chart testing did not show a high sensitivity, as we have discussed already, it was significantly underpowered to comment on this. It may be beneficial to use a highly specific test additionally to reduce false positives when patients find that their Amsler testing has been positive. The combined use of a high sensitivity/low specificity test followed by a low sensitivity/high specificity test in this way has been proposed as a particularly effective way of reducing false positives in the absence of a perfect diagnostic tool with high sensitivity and high specificity [27]. Therefore, the use of the highly specific near acuity reading test on patients who find that they have distortion on Amsler chart testing should be useful for eliminating most of the false positives.
The field of home testing for patients with nAMD is rapidly developing with advances in modern technology. Recently we have seen studies evaluating the compliance of the myVisionTrack system™ (mVT; Vital Art and Science Inc, Richardson TX), a health management tool administered via handheld mobile devices. In this study, the workers reported a high compliance of about 80% using the device daily especially amongst patients with bilateral nAMD [22]. We also experienced a good level of compliance with only 10% withdrawal rate. The ForseeHome (Notal Vision, Ltd., Tel Aviv, Israel) preferential hyperacuity perimeter has shown promise with an 85% sensitivity and specificity in differentiating between patients with intermediate AMD and early CNV [24]. However, authors note 15% exclusion rate due to inability to pass the tutorial and a further 8% excluded due to unreliable home device tests. High prices and issues regarding computer or smartphone-based tests in this patient population may also be barriers to their use [19]. Near reading VA charts are easily accessible, suitable for home use and as we have alluded to have a high compliance and specificity [19].
Recent recommendations for fellow eyes monitoring have suggested home testing in between hospital visits [19]. Lack of an ideal monitoring test means that no single test is currently recommended. In fact, a combination of home devices and reading charts are suggested where available. Of the areas looked at in this study, the near visual acuity reading component showed the highest specificity as well as good compliance. In combination with other higher sensitivity tests, this may represent an easily accessible and patient friendly monitoring test for fellow eye monitoring. This may even be applicable for monitoring of lower risk categories such as those patients with bilateral early dry AMD and in the primary care setting. Recently during the global pandemic, changes and reduction in clinical visits in hospitals, and the need to maintain social distancing for patients coming to hospital, has been very challenging for patients, carers and health professionals. Reliable home monitoring devices are, therefore, particularly important given the current situation and may provide reassurance to patients who are shielding and unable to come urgently for hospital visits.
Conclusion
A reliable diagnostic tool for nAMD in second eyes should detect the onset of nAMD (high sensitivity), to prevent delayed commencement of therapy, and also the absence of nAMD (high specificity) to reduce the burden of false positive visits to hospitals for patients, carers and health professionals. A self-administered near acuity test conducted in patients’ homes with telephone guidance may have potential in reducing the burden of false positive episodes in the large group of patients who are at risk of developing nAMD in their second eyes.
Summary
What is known
-
There is a 10–12% risk of second eye involvement every year in patients with unilateral nAMD. Patients undergoing intravitreal injections for nAMD are often anxious about early detection of nAMD in their fellow eyes, however, no gold standard for home monitoring exists.
What this study adds
-
This study evaluated the usefulness of a 5 stage home-based telephone evaluation method for detecting the presence or absence of nAMD in the second eyes of patients undergoing therapy for nAMD in their first eyes. A self-administered near acuity test conducted in patients’ homes with telephone guidance may have potential in reducing the burden generated by false positive reporting of new nAMD symptoms in the second eyes of of patients with nAMD in their first eyes.
References
Al-Zamil WM, Yassin SA. Recent developments in age-related macular degeneration: a review. Clin Interv Aging. 2017;12:1313.
Bloch SB, Larsen M, Munch IC. Incidence of legal blindness from age-related macular degeneration in Denmark: year 2000 to 2010. Am J Ophthalmol. 2012;153:209–13.e2.
Belkin M, Kalter-Leibovici O, Chetrit A, Skaat A. Time trends in the incidence and causes of blindness in Israel. Am J Ophthalmol. 2013;155:404.
Mitchell P, Bressler N, Doan QV, Dolan C, Ferreira A, Osborne A, et al. Estimated cases of blindness and visual impairment from neovascular age-related macular degeneration avoided in Australia by ranibizumab treatment. PloS One. 2014;9:e101072.
Bressler NM, Doan QV, Varma R, Lee PP, Suner IJ, Dolan C, et al. Estimated cases of legal blindness and visual impairment avoided using ranibizumab for choroidal neovascularization: non-Hispanic white population in the United States with age-related macular degeneration. Arch Ophthalmol. 2011;129:709–17.
Rofagha S, Bhisitkul RB, Boyer DS, Sadda SR, Zhang K, Seven-Up Study Group. Seven-year outcomes in ranibizumab-treated patients in ANCHOR, MARINA, and HORIZON: a multicenter cohort study (SEVEN-UP). Ophthalmology. 2013;120:2292–9.
Brody BL, Gamst AC, Williams RA, Smith AR, Lau PW, Dolnak D, et al. Depression, visual acuity, comorbidity, and disability associated with age-related macular degeneration. Ophthalmology. 2001;108:1893–900.
Rovner BW, Casten RJ. Activity loss and depression in age-related macular degeneration. Am J Geriatr Psychiatry. 2002;10:305–10.
Maguire MG, Daniel E, Shah AR, Grunwald JE, Hagstrom SA, Avery RL, et al. Incidence of choroidal neovascularization in the fellow eye in the comparison of age-related macular degeneration treatments trials. Ophthalmology. 2013;120:2035–41.
Wong T, Chakravarthy U, Klein R, Mitchell P, Zlateva G, Buggage R, et al. The natural history and prognosis of neovascular age-related macular degeneration: a systematic review of the literature and meta-analysis. Ophthalmology. 2008;115:116–26.
Zarranz-Ventura J, Liew G, Johnston RL, Xing W, Akerele T, McKibbin M, et al. The neovascular age-related macular degeneration database: report 2: incidence, management, and visual outcomes of second treated eyes. Ophthalmology. 2014;121:1966–75.
Cornish EE, Teo KY, Nguyen V, Squirrel D, Young S, Gillies MC et al. Five-year incidence and visual acuity outcomes for intravitreal therapy in bilateral neovascular age-related macular degeneration: Fight Retinal Blindness! Project. Retina 2020. https://doi.org/10.1097/IAE.0000000000002798. [E-pub ahead of print]
Kaiser PK, Brown DM, Zhang K, Hudson HL, Holz FG, Shapiro H, et al. Ranibizumab for predominantly classic neovascular age-related macular degeneration: subgroup analysis of first-year ANCHOR results. Am J Ophthal. 2007;144:850–7.
Boyer DS, Antoszyk AN, Awh CC, Bhisitkul RB, Shapiro H, MARINA Study Group. Subgroup analysis of the MARINA study of ranibizumab in neovascular age-related macular degeneration. Ophthalmology. 2007;114:246–52.
Canan H, Sızmaz S, Altan-Yaycıoğlu R, Sarıtürk Ç, Yılmaz G. Visual outcome of intravitreal ranibizumab for exudative age-related macular degeneration: timing and prognosis. Clin Interv Aging. 2014;9:141–5.
Ying GS, Huang J, Maguire MG, Jaffe GJ, Grunwald JE, Toth C, et al. Baseline predictors for one-year visual outcomes with ranibizumab or bevacizumab for neovascular age-related macular degeneration. Ophthalmology. 2013;120:122–9.
Uchida A, Manjunath D, Singh RP, Rachitskaya AV, Kaiser PK, Srivastava SK, et al. Optical coherence tomography angiography in eyes with indeterminate choroidal neovascularization: results from the AVATAR Study. Ophthalmol Retin. 2018;2:1107–17.
Bailey ST, Thaware O, Wang J, Hagag AM, Zhang X, Flaxel CJ, et al. Detection of nonexudative choroidal neovascularization and progression to exudative choroidal neovascularization using oct angiography. Ophthalmol Retin. 2019;3:629–36.
Wong TY, Lanzetta P, Bandello F, Eldem B, Navarro R, Lövestam-Adrian M, et al. Current concepts and modalities for monitoring the fellow eye in neovascular age-related macular degeneration: an expert panel consensus. Retina. 2020;40:599.
Crossland M, Rubin G. The Amsler chart: absence of evidence is not evidence of absence. Br J Ophthalmol. 2007;91:391–3.
Chew EY, Clemons TE, Bressler SB, Elman MJ, Danis RP, Domalpally A, et al. Randomized trial of a home monitoring system for early detection of choroidal neovascularization home monitoring of the Eye (HOME) study. Ophthalmology. 2014;121:535–44.
Kaiser PK, Wang YZ, He YG, Weisberger A, Wolf S, Smith CH. Feasibility of a novel remote daily monitoring system for age-related macular degeneration using mobile handheld devices: results of a pilot study. Retina. 2013;33:1863–70.
Keane PA, De Salvo G, Sim DA, Goverdhan S, Agrawal R, Tufail A. Strategies for improving early detection and diagnosis of neovascular age-related macular degeneration. Clin Ophthalmol. 2015;9:353–66.
Schwartz R, Loewenstein A. Early detection of age related macular degeneration: current status. Int J Retin Vitreous. 2015;1:1–8.
Bujang MA, Adnan TH. Requirements for minimum sample size for sensitivity and specificity analysis. J Clin diagnostic Res. 2016;10:YE01–YE06.
Whillans J, Nazroo J. Assessment of visual impairment: the relationship between self-reported vision and ‘gold-standard’measured visual acuity. Br J Vis Impairment. 2014;32:236–48.
Lalkhen AG, McCluskey A. Clinical tests: sensitivity and specificity. Continuing Educ Anaesth Crit Care Pain. 2008;8:221–3.
Funding
Funded in part by the Tripartite grant from three charitable bodies South Staffordshire Medical FoundationReg. Charity No: 1075209 Rotha Abraham Bequest Reg. Charity No: 509234 The Royal Wolverhampton Hospitals NHS Trust Charity Reg. Charity No: 1059467.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fusi-Rubiano, W., Webb, R., Narendran, N. et al. Identifying early symptoms of choroidal neovascularisation in second eyes of patients with unilateral wet age related macular degeneration using a telephone evaluation method. Eye 35, 3028–3034 (2021). https://doi.org/10.1038/s41433-020-01364-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01364-2