Abstract
Background and objectives
There exists a long-standing perception that diminished stereoacuity has a detrimental effect on microsurgical ability and skills acquisition. This has potential implications on the enrolment of surgical trainees into ophthalmology and other microsurgery specialities. However, strong evidence in this area is lacking. This case–control study aims to establish the exact level of stereopsis impairment at which a statistical drop in surgical performance occurs.
Methods
Fifty participants were enrolled from the University of Dundee Medical School and the NHS Tayside Foundation Doctor programme. Participants were assessed for their stereopsis level before completing an orientation module on an ophthalmic surgical simulator. They were then required to repeat a task four times. Automated and objective performance levels were recorded and analysed.
Results
Nineteen (38%) had stereopsis lower than the defined normal of 60 seconds of arc (arcsec). Statistical analysis found no correlation between visual acuity and surgical performance. No statistical difference was found between performance scores and stereoacuities of 30, 60 and 120 arcsec. A statistically significant difference was discovered in the surgical performance of participants with a stereoacuity worse than 120 arcsec (total score = −69.85) as compared to the ones with a stereoacuity of 120 arcsec or better (total score = −42.23) with p = 0.010.
Conclusions
This study provides evidence of a specific level of stereopsis where statistical degradation of surgical performance occurs. The findings of this work may help formulate policy on stereoacuity standards required to commence microsurgical training.
Similar content being viewed by others
Introduction
Stereopsis, colloquially known as ‘3D vision’, is regarded as crucial for performing microsurgery such as cataract surgery [1, 2]. Stereopsis is defined as the ability to perceive depth secondary to binocular retinal disparity caused by an object within an area called Panum’s fusional space [3]. Panum’s fusional space can be defined as an area in the horizontal plane, where a locus of points in space have the same disparity as fixation and as such appear single [3]. Stereopsis provides information on instrument depth, which is vital to understanding the relative position of intraocular instruments to adjacent structures within the eye. In cataract surgery, it is known that trainees have more complications, and close to 10% of trainees struggle with intraocular surgical training [4]. Previous studies have shown that there is a drop in microsurgical performance when stereoacuity is significantly impaired [1, 2].
There are several methods of clinically assessing stereoacuity. TNO testing is one such method that utilises anaglyphic random dot stereograms and requires red-green filters placed in front of the eyes. When stereoacuity is measured using this method, 60 seconds of arc (arcsec) of stereopsis is considered as the normal cut-off [5].
There is ongoing interest in whether or not deficient stereopsis should be a barrier to ophthalmic surgical training [6]. A relative lack of understanding about the effect of poor stereoacuity on a person’s ability to perform microsurgery has repercussions for the recruitment of trainees. These budding microsurgeons could be advised about their training potential based on their stereoacuity before enrolling in arduous training programmes. The Royal College of Ophthalmologists in the United Kingdom gives the following advice to potential entrants into ophthalmology, ‘good binocular vision and stereopsis is considered to be an advantage for all ophthalmologists in surgical procedures, clinical assessment and in the interpretation of some investigations. You are strongly advised to seek an assessment from an optometrist or orthoptist who will be able to measure your visual acuity and stereovision’, whilst the American Academy of ophthalmology suggests ‘an ophthalmologist will have good fine motor skills, depth perception, and colour vision. Impairment of these abilities may interfere with the effective use of essential ophthalmic instruments, such as the indirect ophthalmoscope and the operating microscope’ [7, 8].
We aim to establish the exact level of stereoacuity at which surgical performance suffers in a microsurgical simulator. This study aims to do this in an age-appropriate cohort, with comparisons made between individuals with normal stereoacuity and those with long-standing deficit.
Methods
We recruited participants in this case–control study between April 2018 and January 2019 (Tables 1 and 2). Given the relative lack of data in this new area of concern, the number of participants enrolled was decided upon by considering the number of recruited individuals reported by previous similar studies [1, 2] to provide the preliminary and seminal data. The prevalence of significant stereopsis deficit in the general population is thought to be relatively low [9]. In order to ensure the enrolment of a significant number of participants with impaired stereoacuity, we advertised for individuals with poor sight in one eye or known deficient stereopsis to take part.
The study took place in the Department of Ophthalmology, Ninewells Hospital, Dundee. The enrolled cohort consisted of medical students and foundation doctors with the potential to pursue a career in microsurgery. Informed consent was obtained from the subjects after explanation of the nature and possible consequences of the study.
All participants had to be able to carry out bi-manual tasks using a surgical simulator. We required that included participants were either a matriculated medical student at the University of Dundee or a qualified junior doctor within the NHS Tayside foundation programme. Participants with more than 2 h of microsurgical simulation experience within the last 12 months were excluded from the study. An experienced orthoptist measured the visual acuity using a Snellen chart, and stereoacuity was assessed using the well-established TNO stereo card testing [7].
Participants carried out several surgical tasks using the VRMagic Eyesi® Ophthalmosurgical Simulator (VRmagic Holding AG, Mannheim, Germany) [10]. Three familiarisation tasks lasting 3 min each were initially completed. These tasks included pointer control and forceps training. Participants were then asked to repeat a forceps manipulation task (Forceps Level 4 module) four times. This task involved the grasping of several three-dimensional cubes and the placement of these cubes in a central sphere.
The Eyesi® simulator software carried out a simultaneous and objective assessment of each participant using multiple data fields (corneal injury area, corneal injury events, lens injury events, lens injury area, tissue treatment, odometer, rotometre, efficiency, time and total score). Only the data acquired from the repeated forceps task was used for comparative analysis.
Ethical approval was granted by a regional ethics committee (18/NE/0059).
Statistical analysis
The data were collated in a spreadsheet and analysed using IBM SPSS Statistics for Windows, Version 22. The tests were two tailed, and type 1 error was set at α = 0.05. Pearson correlation was used to test the correlation between continuous data. Student’s t test was used to compare the two independent variable means of continuous data. When analysing continuous data, one-way analysis of variance (ANOVA) was used to ascertain the difference in means of three or more independent variables.
Results
Table 1 summarises the participant characteristics. Impaired stereopsis is defined as a stereoacuity of worse than 60 arcsec; 19 (38%) participants met these criteria. Table 2 summarises the participants’ Snellen visual acuity in LogMar and stereoacuity, along with their performance scores in different surgical facets. Irrespective of their visual acuity and stereoacuity, all the participants caused some degree of tissue injury during the task performance.
A statistically significant improvement in total score was seen between the first and the fourth attempts of the participants (−70.1 vs. −33.9, p value = 0.009). There was no statistically significant difference between male and female average total scores (−44.9 vs. 50.2, p value = 0.428). No correlation between age (r = 0.22, p value = 0.124) or training stage (r = 0.20, p value = 0.175) and average total scores was seen. There was no statistically significant difference in average total scores based on prior experience with Eyesi®.
There was no statistically significant correlation between best binocular visual acuity and performance scores in different surgical facets in this cohort (Table 3). The best binocular visual acuity ranged −0.20 of LogMAR to 0.20 of LogMAR. The mean best binocular visual acuity was −0.10 of LogMAR with a standard deviation of 0.11 of LogMAR. The one-way ANOVA test demonstrated no statistically significant difference in best binocular visual acuity between the groups of participants with different stereoacuities (F(4, 45) = 0.509, p = 0.729). The one-way ANOVA test did not reveal any statistically significant performance difference between stereoacuities of 30, 60 and 120 arcsec while carrying out different surgical facets.
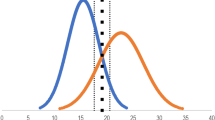
There was a statistically significant difference in the surgical performance of participants with stereoacuity worse than 120 arcsec as compared to the ones with stereoacuity of 120 arcsec or better, which was independent of best binocular visual acuity (Table 4). Participants with stereoacuity worse than 120 arcsec had a statistically significant worse score in tissue treatment, corneal injury event and corneal injury area as compared to the participants with stereoacuity of 120 arcsec or better (Fig. 1a). The average total score of the participants with stereoacuity worse than 120 arcsec was also statistically significantly poorer than the participants with stereoacuity of 120 arcsec or better (Fig. 1b). However, all participants demonstrated learning effect with consistent improvement in total scores between attempts (Fig. 1b).
a Tissue treatment, corneal injury event and corneal injury area scores for participants with stereoacuity better than and worse than 120 seconds of arc. b The average total score is compared with the total scores for each repetition for participants with stereoacuity better than and worse than 120 seconds of arc.
Discussion
Synopsis of key findings
One of the pertinent questions at the forefront of a potential microsurgical candidate’s and their recruiter’s mind is whether the candidate has the physical attributes to embark on a surgically demanding training programme such as ophthalmic specialist training. Conventional wisdom dictates that stereopsis plays an important role when performing microsurgery such as cataract surgery [4, 7, 8]. Although 60 arcsec is considered as the ‘normal’ level of stereoacuity, the precise threshold of stereoacuity needed for these tasks is unknown. This study provides evidence that microsurgical performance suffers once the level of stereoacuity is below 120 arcsec, rather than 60 arcsec. It should be noted that only ten participants were recorded as having a stereoacuity below this threshold.
Unsurprisingly, the aspects of microsurgery that require good depth perception to accurately manipulate the surgical instruments in three-dimensional space inside the eye suffered the most from deteriorating stereopsis. The participants with stereoacuity below 120 arcsec damaged the corneal endothelium, and other intraocular tissues, more frequently and severely as they could not judge the depth of the tip of their instrument (Fig. 1a). The duration and efficiency of task completion tended to be worse in participants with a stereoacuity worse than 120 arcsec, although this did not reach statistical significance (Table 3). Crucially, the total score, which is a composite score of the overall surgical performance, was almost two-fold worse in participants with stereoacuity below 120 arcsec (Fig. 1b). All participants showed learning effect with improvement in performance at each subsequent attempt, however, participants with stereoacuity below 120 arcsec always performed worse (Fig. 1b). Our study was not designed to specifically assess if learning effect and a large number of repetitions can overcome the deficiency in stereoacuity when performing surgical tasks.
The odometry and rotometry findings, which quantify the velocity, the linear and rotational acceleration of the instrument tip, were independent of stereopsis. We speculate that odometry and rotometry are related to manual dexterity rather than stereopsis.
In our study, the level of best binocular visual acuity was unrelated to surgical performances as all participants had close to normal best binocular visual acuity, and the variation in the binocular visual acuity were evenly distributed among the participants with different stereoacuity. In fact, 60% of the participants with stereoacuity worse than 120 arcsec, had a visual acuity of 0.00 of LogMAR or better in each eye. Most of the participants did not have any prior microsurgical experience (Table 1) and no improvement in performance was seen in the few participants with a very limited prior experience. Surgical performance was not affected by age, gender or stage of training and thus these were not considered as confounding factors.
Strengths of this study
Qualified and experienced orthoptists carried out the assessment of the participant’s stereopsis. These ensured accurate and reliable measurements were recorded. The use of orthoptists in this context helps to reduce bias by removing the investigating team from the stereopsis assessment process.
Orthoptists used TNO stereoacuity assessment to test and record the level of stereopsis for each participant. TNO is a reliable, tried and tested method of measuring a broad range of stereoacuities, from complete absence to 5 arcsec [11]. We define the normal level of stereoacuity as 60 arcsec. This is a robust, test specific value, derived from previously published data supporting its use as representing normal stereoacuity [7].
The effect of stereopsis on the ability to perform simulated microsurgery is assessed in an age-appropriate cohort with long-standing stereopsis impairment such as amblyopia. Our work is, therefore, more clinically applicable than previous similar studies, which have either covered one eye of a participant or used an inappropriately aged cohort [2, 4].
We utilised automated recording software to provide a truly objective and reliable form of surgical performance measurement [10].
Study limitations
The relatively small number of participants limits the effect of the outcome in this study. However, in mitigation, the cohort selection was from a small population of individuals with the potential to become future microsurgeons. Of the 50 participants, 19 (38%) had impaired stereopsis. In the general population, reduced stereopsis is relatively rare (3.7% in a study of 2343 children) [9]. A cohort of 38% with impaired stereopsis is therefore a significant proportion of the overall number of participants.
The learned adaptations that an individual with impaired stereoacuity makes when judging depth were not considered in this work. It does not therefore make assumptions on the level of benefit inferred by such adaptations. All the individuals with stereopsis impairment had long-standing reduced stereoacuity, and it is therefore assumed that any such adaptations are equal across participants.
Comparisons with other studies
Waqar et al. [12] showed that junior doctors with one eye occluded performed statistically worse with microsurgical simulation tasks than with both eyes open. This highlights the strength of this study to consider the detrimental effects of a long-term loss of stereoacuity on microsurgical performance.
Sachdeva and Traboulsi [2] investigated the ability of individuals to undertake microsurgery simulation tasks with long-standing impaired stereopsis. They found a decrease in simulated surgical performance in those with impaired stereopsis. Forty-two participants were included in the authors’ analysis and the age range was between 10 and 64. This age range is not applicable to potential ophthalmic trainees. There could therefore be confounding factors that are contributing to the conclusions of the authors’ work. The participants in our cohort were either medical students or junior doctors with the potential to start ophthalmic training.
Selvander and Åsman [4] illustrated that impairment in stereopsis at the start of training may lead to a slower and more difficult training. However, we do not know if the effects of reduced stereopsis are long term and whether or not surgical experience can partially or completely offset this deficit. Further studies would be required to assess the effect of training and experience.
More recently, Dutton et al. [13] evaluated the influence of stereopsis on the ability to perform simulated microsurgery. They recruited participants with normal stereopsis levels and artificially degraded their stereopsis. This was achieved by the placement of a band-pass filter over the non-dominant eye, reducing stereopsis to 150 arcsec, or occluding the vision in this eye completely to attain an absence of stereoacuity. They demonstrate a reduced ability to perform microsurgery at the pre-selected level of 150 arcsec. They also show that this ability is further reduced with a complete absence of stereoacuity. In comparison, we evaluate microsurgical ability in participants with long-term stereopsis impairment with presumed adaptation. We also evaluate performance across all levels of stereopsis deficit as opposed to an arbitrarily selected value.
Clinical applicability
The Royal College of Ophthalmologists in the United Kingdom recommends that stereopsis is assessed before embarking on ophthalmic training [9]. No specific level of stereoacuity impairment is given as a cut-off for entry to training, it does, however, state that good stereopsis is considered to be an advantage in performing surgical procedures. The Netherlands is the only European country to insist on stereopsis assessment in aspiring ophthalmologists [4].
It would seem logical to suggest any proposed cut-off to surgical ophthalmic training should be enforced at the current level of defined impairment (worse than 60 arcsec using TNO assessment). However, any move to insist on such a prerequisite would require robust evidence, which has been absent. We contribute by providing evidence that the level of stereoacuity at which a reduction in surgical ability occurs is worse than 120 arcsec. Emphasis should be made that only ten participants were found to have a stereopsis of <120 arcsec. This study provides evidence that surgical performance improves with repetition and does not assess if long-term learning effect can overcome a deficiency in stereoacuity when performing surgical tasks.
Conclusions
This study aids in the understanding of the role of stereoacuity in performing microsurgical tasks. In an appropriate cohort of participants, this work has shown that there is a statistical drop-off in performance when stereoacuity is assessed to be worse than 120 arcsec. This is a significant outcome and addresses a gap in the current literature by highlighting a specific level of stereopsis where degradation of surgical performance occurs. The findings of this study may help formulate policy on stereoacuity standards required to commence surgical ophthalmic training. It is important to recognise that the effect of training and experience on the statistical differences found in this surgically naïve cohort is not understood. Further studies are required focusing on the effects of training in individuals with poor stereoacuity.
Summary
What was known before
-
Stereopsis plays a major role in the ability of an individual to judge the position of surgical instruments in relation to adjacent structures within the eye.
-
Participants with monocular occlusion and subsequent stereopsis impairment perform poorly when undertaking simulated microsurgery.
-
Long-term, adapted deficit of stereoacuity is correlated with a statistical drop in microsurgical performance when compared with individuals with normal levels of stereoacuity.
What this study adds
-
For the first time, a stereoacuity of worse than 120 seconds of arc is shown to be the specific level of stereoacuity at which individuals demonstrate a statistical drop in simulated microsurgical performance.
-
All participants studied are surgically naive potential microsurgeons. Any impairment of stereoacuity in these participants is long-standing, and therefore adaptations to spatial awareness are ubiquitous in this cohort.
-
With a growing body of evidence that shows a deficit in stereoacuity effects surgical ability, the findings of this study help to potentially formulate ophthalmic training admission standards.
Data availability
Available on request.
References
Nibourg LM, Wanders W, Cornelissen FW, Koopmans SA. Influence of stereoscopic vision on task performance with an operating microscope. J Cataract Refract Surg. 2015;41:1919–25.
Sachdeva R, Traboulsi EI. Performance of patients with deficient stereoacuity on the EYESi microsurgical simulator. Am J Ophthalmol. 2011;151:427–33.
Bishop PO. Binocular vison. In: Moses RA, Hart WM, editors. Adler’s physiology of the eye: clinical application. St Louis: CV Mosby, 1987. p. 619e89.
Selvander M, Åsman P. Stereoacuity and intraocular surgical skill: effect of stereoacuity level on virtual reality intraocular surgical performance. J Cataract Refract Surg. 2011;37:2188–93.
Piano ME, Tidbury LP, O’Connor AR. Normative values for near and distance clinical tests of stereoacuity. Strabismus. 2016;24:169–72.
Wong NW, Stokes J, Foss AJ, McGraw PV. Should there be a visual standard for ophthalmologists and other surgeons? Postgrad Med J. 2010;86:354–8.
Royal College of Ophthalmologists. Royal College of Ophthalmologists.ac.uk. 2020. https://www.rcophth.ac.uk/curriculum/ost/entering-ost/.
American Academy of Ophthalmology. American Academy of Ophthalmology.org. 2020. https://www.aao.org/medical-students/practice-of-ophthalmology.
Robaei D, Huynh SC, Kifley A, Gole GA, Mitchell P. Stereoacuity and ocular associations at age 12 years: findings from a population-based study. J Am Assoc Pediatr Ophthalmol Strabismus. 2007;11:356–61.
VRMagic. EYESi ophthalmic surgery simulator user guide. Mannheim: VRMagic; 2006. p. 58e9.
Simons K. A comparison of the Frisby, Random-Dot E, TNO, and Randot circles stereotests in screening and office use. Arch Ophthalmol. 1981;99:446–52.
Waqar S, Williams O, Park J, Modi N, Kersey T, Sleep T. Can virtual reality simulation help to determine the importance of stereopsis in intraocular surgery? Br J Ophthalmol. 2012;96:742–6.
Dutton J, Watkins A, Henderson J, Burgess FR, Tint NL, Dhillon B, et al. Influence of stereopsis on the ability to perform simulated microsurgery. J Cataract Refract Surg. 2020;46:549–54.
Acknowledgements
We would like to acknowledge the funding from the Royal College of Surgeons Edinburgh.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Burgess, S., Kousha, O., Khalil, M. et al. Impact of stereoacuity on simulated cataract surgery ability. Eye 35, 3116–3122 (2021). https://doi.org/10.1038/s41433-020-01346-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01346-4