Abstract
Background/objectives
The Arclight is a novel, low-cost, solar-powered direct ophthalmoscope developed for low resource settings as an alternative to more expensive, conventional devices. The Brückner reflex test (BRT) is a quick and effective means to screen for eye disease and amblyogenic risk factors. This test is however rarely performed in low resource settings due to the lack of access to ophthalmoscopes and trained health care workers. Our aim was to establish the sensitivity and specificity of the BRT when performed by a non-expert using an Arclight and compare to an expert as well as the results of a full clinic workup.
Subjects/methods
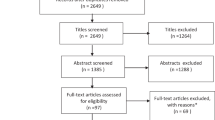
In this prospective, blinded study, 64 patients referred to a paediatric ophthalmology clinic had the BRT performed by a ‘non-expert’ observer (medical student) then an ‘expert’ observer (consultant ophthalmologist). These results were then compared against the ‘gold standard’ outcomes of a full clinical workup.
Results
BRT screening by the expert observer led to a sensitivity of 75.0% [95% CI: 57.9–86.8%] and a specificity of 90.6% [95% CI: 75.8–96.8%] in picking up media opacity, strabismus, refractive error or a combination of the above. For the non-expert, the sensitivity and specificity were 71.9% [95% CI: 54.6–84.4%] and 84.4% [95% CI: 68.3–93.1%], respectively.
Conclusions
The Arclight can be effectively used to perform the BRT and identify eye disease and common amblyogenic risk factors. Even when performed by a non-expert the results are highly specific and moderately sensitive. This study consequently offers support for the use of this low-cost ophthalmoscope in the expansion of eye screening by health care workers in low resource settings.
Similar content being viewed by others
Introduction
Sight loss is greatest in low and middle-income countries (LMIC’s) where eye health worker numbers and their access to diagnostic tools is least [1]. While childhood visual impairment is less prevalent than in adults, the overall loss of life years is second only to that of adult cataract. Importantly, if identified early nearly half of such disability is treatable and preventable by known cost-effective means [2].
The Brückner reflex test [3] (BRT) (Fig. 1) is a simple yet effective means to identify the early signs of childhood eye disease, such as corneal scarring, cataract and retinoblastoma as well as risk factors for amblyopia including strabismus, high refractive error and anisometropia.
Left panel; The room should be dimly lit and quiet. The child should be sat comfortably on parent’s lap with undilated pupils. The ophthalmoscope should be set at the brightest setting and lens at zero. It should be held at arm’s length away and the reflex viewed simultaneously in both eyes. Right panel; A Normal: central corneal reflections, symmetrical brightness and colour. B Media opacity left eye: dark reflex. C Esotropia left eye: corneal reflection displaced temporally and reflex lighter. D Exotropia right eye: corneal reflection displaced nasally and reflex lighter. E Hypermetropia right: prominent bright crescent superiorly and myopia left: prominent bright crescent inferiorly.
The BRT is performed using a direct ophthalmoscope (DO), ideally in a dim room at arm’s length, illuminating both eyes of the patient at the same time. The child should be seated comfortably ideally on a parent’s lap. The reflected light (reflex) from both eyes is observed simultaneously. The relative colour, brightness and position of the crescents within the pupil space are compared. This is called the ‘red reflex’ test. It is important to note that the colour of the central ‘red’ reflex can be very variable and although orange–red in Caucasians can be almost blue–white in darker pigmented eyes [3]. In addition, the centration of the small ‘corneal’ reflex is noted. This is known as the Hirschberg Test [4]. The combination of these two tests is the BRT.
This non-touch arm’s length combination test lets users make swift on-the-spot decisions, to identify disease early for better outcomes. Despite the benefits of routinely performing the BRT, in LMIC’s it is rarely performed by primary or mid-level health care workers; with disease presenting often sadly very late [5, 6]. Absence of appropriate frugal kit and the circular lack of teaching of practical and interpretation skills are perpetual well-observed challenges.
The Arclight [7,8,9] (Fig. 2) is a DO developed specifically with the needs of users in low resource settings in mind. Low cost (~£10), portable, LED illuminated and solar powered: it does not rely on expensive and hard to find consumables, such as batteries and bulbs. Studies amongst mid-level eye care workers in LMIC’s have demonstrated it to be easier to use than more expensive traditional devices yet remaining as effective for fundoscopy and ‘red’ reflex examination [9, 10].
Our study aims to describe the effectiveness in children, of the BRT in identifying eye disease that can lead to amblyopia, using this new low-cost Arclight ophthalmoscope. The results of an ‘expert’ ophthalmology consultant and a ‘non-expert’ medical student were compared with each other, and then against the results of a ‘gold standard’ full clinic workup.
Materials and methods
This blinded, prospective study was approved by the institutional review board of LV Prasad Eye Institute and the ethics review committee of the University of St Andrews. Signed informed consent was obtained from the parents of all study participants. Children between the ages of 3 months and 14 years presenting consecutively to the paediatric ophthalmology clinic at LV Prasad Eye Institute were enroled in the study. Patients previously known to the expert observer were excluded.
Prior to the study, the non-expert examiner participated in an Arclight training workshop on how to use the device as well as perform and interpret the BRT. This included 1 h with a paediatric ophthalmologist familiar with the device and then examination of simulation red reflex eyes displaying pathology as well as normal adult eyes.
Study participants were seated comfortably, typically on a parent’s lap in a dimly lit room. Using the brightest light on the Arclight with the lens set to zero both eyes were observed undilated at arm’s length. The expert and non-expert examiners recorded their observations as either normal or abnormal. If abnormal, the examiners classified their observations into further subcategories of media opacity, strabismus, refractive error or a combination of the above.
After the BRT each patient underwent routine full clinic workup involving history taking, orthoptic assessment, slit-lamp examination, dilated fundoscopy and refraction. The findings of the ‘gold standard’ full clinic workup were then used to classify the cases into the same subcategories described above by a different and independent experienced paediatric ophthalmologist.
Results
Overall, 64 patients (36 male and 28 female) were enroled into the study. The participants ranged from 8 months to 14 years with a mean age of 6 years. Three patients were excluded as they were previously known to the expert observer. Full clinic workup identified 32 patients having either media opacity, strabismus, anisometropia (≥1.00D SPH) or high refractive error (>+5.00 D SPH or <−5.00 D SPH). The remaining 32 participants based on the full clinic workup were deemed to have findings that would be consistent with a normal BRT.
The results of both examiners BRT and the ‘gold standard’ full clinic workup are summarised in Table 1. Table 2 displays the results of the non-expert and expert’s BRT findings.
The non-expert and expert BRT findings produced similar sensitivities and specificities to each other (Table 3). Both observers despite their difference in the level of experience achieved sensitivities of over 70% and specificities of over 80% compared to the ‘full clinic workup’ with the expert being statistically higher at 90.6% [95% CI: 75.8–96.8%]. As a consequence, good agreement between both observers was found with a Cohen’s kappa of 0.71 [95% CI: 0.47–0.96]. Cohen’s kappa showed moderate agreement with the gold standard results of the full clinic workup: 0.56 [95% CI: 0.32–0.81] for the non-expert observer and slightly higher agreement of 0.66 [95% CI: 0.41–0.89] for the expert.
Of the 24 cases that the expert observer felt had abnormal BRTs 23 were correctly subclassified based on the results of the full clinic workup. The non-expert observer identified 23 cases with abnormal BRT and subclassified 17 of these correctly.
Of the eight patients incorrectly identified by the expert as having a normal reflex (false negatives) when based on the findings of the full clinic work up they were classified as an ‘abnormal’ BRT, one had anisometropia, two had symmetrical significant refractive error, three patients had esotropia of 10PD, 12PD and 35PD, and two had a combination of anisometropia (dominant pathology) and strabismus. The non-expert observer incorrectly identified nine patients as having a normal reflex (false negatives). Seven of these cases were the same as the expert with the other two being anisometropia with strabismus and anisometropia only.
Discussion
Our results show that the BRT when performed with the Arclight ophthalmoscope can be used as a quick means to identify risk factors for amblyopia in a high-volume paediatric ophthalmology clinic. When performed by an expert, it has a sensitivity of 75% and a specificity of 91%. An important finding of this study is that the non-ophthalmic medical student observer’s performance was statistically comparable to the expert observer. This is consistent with a previous study where Gole et al. [11] reported 85.6% sensitivity and 65% specificity when the BRT was performed by a non-ophthalmologist with an experienced ophthalmologist reporting 73% sensitivity and 87% specificity. Closer analysis of the cases identified and missed suggests that the BRT is best suited to the identification of media opacities and larger angled strabismus (>35PD). The BRT as expected, was less effective at identifying cases of smaller strabismus (<35PD) and refractive error with clear media. Symmetrical refractive errors were typically hard to identify. For example, two patients with symmetrical myopia of −4.00 dioptres as well as a patient with a refraction of −5.00 dioptres in the right eye and −6.00 in the left eye were falsely classified as normal by both observers. These patients were noted to demonstrate an increasingly dim reflex but the brighter lower crescent associated with myopia was not appreciable [12,13,14]. Another group of patients with a combination of both strabismus and refractive error were also found in the false negative results. This could be due to the brighter reflex from the manifestly squinting eye being neutralised by the dimming effect of a high refractive reflex.
A similar study from Pakistan assessed the effectiveness of the BRT in identifying refractive errors in children. They reported sensitivity of 97% and specificity of 79% [12], higher than in our study. Another study reported similarly accurate detection rates of refractive errors with a sensitivity of 91% and specificity of 72.9% [13]. One study [14] evaluated the BRT of paediatric patients using a camera (in place of a direct ophthalmoscope) and reported 86% sensitivity and 85% specificity. There are a number of possible reasons for these different findings including different age groups of participating children, varying degrees of appreciable pathology and the use of different brands of ophthalmoscope. Even though there are differences in sensitivity and specificity they are generally high and clinically useful confirming the potential benefits of using this simple and non-invasive the test more widely. This is especially the case now that a low cost and consumable independent device, such as the Arclight is available.
Performing a formal comprehensive eye examination in babies and young children is challenging. The attraction of the BRT reflex lies in its simplicity; it takes just a few seconds of the child looking straight at the light to make an assessment. Non-ophthalmic staff who provide care to children, such as paediatricians, staff delivering immunisation programmes and neonatal/obstetric nurses could be trained to perform the BRT both opportunistically and systematically in their daily work. The feasibility of this approach has recently been evaluated in Tanzania demonstrating the Arclight to have sensitivity and specificity of over 90% [15]. This could lead to earlier identification of eye conditions benefiting from intervention potentially improving outcomes of treatment and reducing the burden of visual impairment in children.
Importantly the Arclight can also be attached to the camera of a mobile phone to acquire an image or video [8, 16]. Telemedicine could complement the expansion of the use of the BRT with electronic transfer of suspect findings to remote experts for an opinion or interpretation of the images in real time by an algorithm within the mobile phone. This approach could further assist in reducing the burden of eye disease and associated visual impairment amongst children particularly in low resource settings where local access to paediatric ophthalmology services can be limited.
The main limitations of this study include the small number of very young participants (who would benefit most from early diagnosis) and of performing the ‘screening’ in a contrived ‘pathology-rich’ paediatric ophthalmology clinic. Future work should aim to assess the real-world feasibility of implementing high-volume screening of infants and babies in immunisation clinics [17], birthing facilities and child health clinics by primary health care workers (PHCWs). These are settings where it would be more beneficial to screen but also challenging to successfully implement. One such initiative which piggybacks onto routine national child health surveillance programmes has been rolled out in Kenya and Uganda [18], with positive results [19] and is now being expanded to Tanzania.
Overall, these findings raise the prospect of being able to equip at low cost and effectively train non-expert PHCWs to perform the BRT in LMICs complementing other ongoing blindness reduction strategies.
Summary
What was known before
-
The Brückner reflex test using a traditional direct ophthalmoscope, is a well-established means to identify eye disease and risk factors for amblyopia.
-
The burden of childhood blindness is greatest in low-income countries where access to diagnostic tools and trained health workers is least.
-
The Arclight is a low-cost direct ophthalmoscope that has been shown to be as effective as more expensive orthodox devices in both simulated and healthy eyes.
What this study adds
-
This is the first study to evaluate the performance of the BRT using the Arclight in patients with eye disease.
-
Using the Arclight, a non-expert with basic training can perform the Brückner reflex test with comparable results to an expert.
-
Broadening the delivery of eye screening using this frugal ophthalmoscope could make a valuable addition to ongoing blindness reduction strategies in low resource settings.
References
Bastawrous A, Hennig BD. The global inverse care law: a distorted map of blindness. Br J Ophthalmol. 2012;96:1357–8. http://bjo.bmj.com/content/96/10/1357.2.abstract.
Gilbert C, Foster A. Childhood blindness in the context of VISION 2020—the right to sight. Bull World Health Organ. 2001;79:227–32. https://pubmed.ncbi.nlm.nih.gov/11285667.
Brückner R. Exakte Strabismusdiagnostik bei 1/2–3jährigen Kindern mit einem einfachen Verfahren, dem >Durchleuchtungstest<. Ophthalmologica. 1962;144:184–98. https://www.karger.com/DOI/10.1159/000304320.
Kanski JJ, Bowling B. Clinical Ophthalmology: a systematic approach. Edinburgh, Elsevier/Saunders; 2015. p. 316.
Sheeladevi S, Lawrenson JG, Fielder A, Kekunnaya R, Ali R, Borah RR, et al. Delay in presentation to hospital for childhood cataract surgery in India. Eye. 2018;1811–8. https://doi.org/10.1038/s41433-018-0176-2.
Bronsard A, Geneau R, Shirima S, Courtright P, Mwende J. Why are children brought late for cataract surgery? Qualitative findings from Tanzania. Ophthalmic Epidemiol. 2008;15:383–8. https://doi.org/10.1080/09286580802488624.
Blaikie A, Sandford-Smith J, Tuteja SY, Williams CD, O’Callaghan C. Arclight: a pocket ophthalmoscope for the 21st century. BMJ. 2016;355. http://www.bmj.com/content/355/bmj.i6637.
Kousha O, Blaikie A. The Arclight and how to use it. Community Eye Heal. 2019;32:50–1. https://pubmed.ncbi.nlm.nih.gov/32123473.
Dooley E, Kousha O, Msosa J, Ndaule E, Abraham C, Parr J, et al. Comparative evaluation of a low cost direct ophthalmoscope (Arclight) for red reflex assessment among healthcare workers in Malawi. BMJ Innov. 2020. http://innovations.bmj.com/content/early/2020/04/09/bmjinnov-2019-000361.abstract.
Blundell R, Roberts D, Fioratou E, Abraham C, Msosa J, Chirambo T, et al. Comparative evaluation of a novel solar powered low-cost ophthalmoscope (Arclight) by eye healthcare workers in Malawi. BMJ Innov. 2018;4:98–102.
Gole GA, Douglas LM. Validity of the Bruckner reflex in the detection of amblyopia. Aust N. Z J Ophthalmol. 1995;23:281–5.
Jalis M, Ashfaq MW, Imdad A. Use of Bruckner test for the detection of significant refractive errors in children. J Rawalpindi Med Coll. 2015;19:200–3. https://pdfs.semanticscholar.org/7ab0/a5ca99ecf21c28bce70cd09c79f5f5cd8e17.pdf.
Kothari M. Can the Bruckner test be used as a rapid screening test to detect significant refractive errors in children? Indian J Ophthalmol. 2007;55:213–5. http://www.ijo.in/article.asp?issn=0301-4738.
Bani SAO, Amitava AK, Sharma R, Danish A. Beyond photography: evaluation of the consumer digital camera to identify strabismus and anisometropia by analyzing the Bruckner’s reflex. Indian J Ophthalmol. 2013;61:608–11. http://www.ijo.in/article.asp?issn=0301-4738.
Mndeme FG, Mmbaga BT, Kim MJ, Sinke L, Allen L, Mgaya E, et al. Red reflex examination in reproductive and child health clinics for early detection of paediatric cataract and ocular media disorders: cross-sectional diagnostic accuracy and feasibility studies from Kilimanjaro, Tanzania. Eye. 2020. https://doi.org/10.1038/s41433-020-1019-5.
Wu GT, Kang JM, Mirza RG, Bidwell AE, Gray JP. The use and evaluation of an inexpensive eye model in direct ophthalmoscopy training. J Acad Ophthalmol. 2014;1:e21–5.
Jac-okereke CC, Jac-okereke CA, Ezegwui IR, Okoye O. Vision screening in infants attending immunization clinics in a developing country.J Prim Care Community Health. 2020;11:2150132720907430. https://pubmed.ncbi.nlm.nih.gov/32100627.
Sense International. Sense International launches pioneering screening programme for infant deafblindness in Kenya and Uganda. 2017. https://senseinternational.org.uk/news/sense-international-launches-pioneering-screening-programme-infant-deafblindness-kenya-and.
Sense International. Celebrating the results of the screening and early intervention programme funded by the ‘Finding Grace’ appeal. 2020. https://www.senseinternational.org.uk/news/celebrating-results-screening-and-early-intervention-programme-funded-finding-grace-appeal.
Acknowledgements
We would like to thank William J Williams for his assistance in preparing illustrations and all of our colleagues at L V Prasad Eye Institute, Hyderabad, India for their support in carrying out this study.
Funding
This study was performed as part of an undergraduate medical elective. It was not funded by any specific grant-awarding body.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AB is seconded to the University of St Andrews from NHS Fife. The University owns a social enterprise subsidiary company, for which he acts as an unpaid adviser. The social enterprise business sells the Arclight to users in high resource countries with all profits being used to fund distribution and education exercises of the device in low-income countries via the Global Health Implementation team at the University of St Andrews. Both SYT and AB have previously published on the topic of the Arclight. RK does not declare any potential conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tuteja, S.Y., Blaikie, A. & Kekunnaya, R. Identification of amblyogenic risk factors with the Brückner reflex test using the low-cost Arclight direct ophthalmoscope. Eye 35, 3007–3011 (2021). https://doi.org/10.1038/s41433-020-01341-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01341-9