Abstract
Objectives
To ascertain adherence to an international consensus target of ≤7.5 mg/day of prednisolone for maintenance systemic corticosteroid (CS) prescribing in uveitis and report the frequency of courses of high-dose systemic CS in the UK.
Methods
We conducted a national, multicentre audit of systemic CS prescribing for uveitis at 11 UK sites between November 2018 and March 2019. High-dose CS was defined as (1) maintenance >7.5 mg prednisolone for >3 consecutive months, or (2) >1 course ≥40 mg oral CS or ≥500 mg intravenous (IV) methylprednisolone in the past 12 months. Case notes of patients exceeding threshold CS doses were reviewed by an independent uveitis specialist and judged as avoidable or not, based upon a scoring matrix.
Results
Of 667 eligible patients, 285 (42.7%) were treated with oral or IV CS over the preceding 12 months; 96 (33.7%) of these exceeded the threshold for high-dose CS. Twenty-five percent of prescribing in patients on excess CS was judged avoidable; attributed to either prescribing long-term CS without evidence of consideration of alternative strategies, prescribing error or miscommunication. More patients received immunomodulatory therapy (IMT) in the group treated with CS above threshold than below threshold (p < 0.001) but there was no significant difference in doses of IMT.
Conclusion
33% of patients had been prescribed excessive corticosteroid when compared to the reference standard. An analysis of decision-making suggests there may be opportunity to reduce excess CS prescribing in 25% of these patients.
Similar content being viewed by others
Introduction
Corticosteroids (CS) have been the mainstay of treatment for non-infectious uveitis (NIU) and scleritis since the middle of the 20th century. NIU is often a chronic disease characterised by remission and relapses affecting vision. Systemic CS are a highly effective first line in therapy which rapidly and inexpensively control active disease and prevent relapses. The medium and long-term risk profile of systemic CS is well-known and includes weight gain, thrombotic venous occlusions, hypertension, diabetes, osteoporosis and adrenal insufficiency. Within the eye, their use results in secondary complications such as glaucoma and cataract [1]. A daily oral prednisolone dose in excess of 7.5 mg/day is associated with a greater than twofold increase in risk of cardiovascular events [2]. Although the exact relation between dose and adverse effects remains unknown, significant reductions in bone mineral density are associated with doses ≥5 mg/day [1]. In the context of biologic therapies, a large registry study showed that the risk of infection was directly related to the dose of systemic CS [3].
Consensus guidelines for NIU published in 2000 recommend a maximum maintenance (>3 consecutive months) dose of 10 mg/day oral prednisolone and steroid-sparing immunomodulatory therapy (IMT) in patients requiring more than 10 mg/day [4]. This principle was reiterated by an international consensus group, recommending IMT for relapses after reduction of oral CS dose to 7–10 mg/day [5]. Other speciality groups within the UK, including rheumatology have guidelines for CS use in clinical practice to minimise the burden of side effects [6]. Consequently, a maintenance dose of ≤7.5 mg/day CS, usually prednisolone in the UK, is considered an acceptable target for maintenance treatment by uveitis specialists and other physicians treating autoimmune diseases [6, 7]. However, adherence to a consensus target by practising uveitis specialists is unknown. High dose systemic CS contribute to cumulative CS exposure [1] but no study to date has reported upon the frequency with which courses of high dose systemic CS are prescribed in uveitis.
The Ocular Inflammation Steroid Toxicity Risk (OSTRICH) study was conducted to evaluate patterns of CS use in uveitis and scleritis through the UK National Uveitis Clinical Study Group [8], a clinical research network of uveitis specialists based within the UK. We wished to determine the proportion of patients prescribed excess of 7.5 mg of prednisolone for 3 months, and the number of episodes of high dose systemic CS use for relapses or poorly controlled disease amongst participating centres.
Methods
The OSTRICH study was conducted as a national, multicentre audit at eleven sites in the UK. All members of the UK Uveitis National Clinical Study Group [8], a national clinical research organisation for ophthalmologists managing uveitis patients in secondary and tertiary institutions, were invited to participate in this study. Ten out of eleven participating sites were tertiary uveitis centres, representing half of all tertiary centres in the UK.
Institutional Caldicott Guardian approval was obtained at each site; ethical approval was not required by our institutional review board. The study was carried out in two phases; the output from Phase 1 was utilised in Phase 2. Anonymised site and subject data were collected and stored securely using a REDCap database (v8.10 © 2020 Vanderbilt University, Nashville, TN, USA) held at the University of Oxford [9, 10].
Phase 1: CS data collection
We wished to determine the proportion of patients with non-infectious uveitis or scleritis who met criteria for excess systemic CS in the past 12 months. The criteria for excess CS were (1) a maintenance dose of >7.5 mg prednisolone for >3 consecutive months or (2) >1 course of rescue CS therapy (≥40 mg oral CS or ≥500 mg intravenous methylprednisolone), in the past 12 months. For the purposes of this study, we adopted a threshold of one course of high dose systemic CS per year from the British Society of Gastroenterology guidelines as acceptable [7].
Uveitis specialists at eleven sites across the UK completed questionnaires for consecutive non-infectious uveitis and scleritis patients attending clinic for a 6-week period between November 2018 and March 2019. Data collected included diagnosis, the presence of active uveitis or scleritis, sight-threatening complications, and all treatments received in the past 12 months (Table 1, Supplementary information).
Subjects meeting eligibility criteria were (1) over 16 years old, (2) had a diagnosis of non-infectious chronic anterior uveitis, intermediate uveitis, posterior uveitis, panuveitis or non-infectious scleritis and (3) had been followed up for at least 6 months. Patients who were prescribed CS for systemic disease rather than ocular inflammation were removed from the study.
Phase 2: Scoring matrix for CS prescribing
Case notes from a sample of 52 subjects in 5 sites, meeting the criteria for excess CS in the past 12 months, were reviewed by an independent uveitis expert, either at the same or a different site and were masked to identifying data if at a different site. The notes were placed in two categories, either avoidable or unavoidable excess steroid prescribing, according to a scoring matrix. (Table 1 shows the reasons for avoidable and unavoidable excess CS prescribing).
Phase 1 and Phase 2 are summarised in the algorithm in Fig. 1.
11 centres participated in Phase 1 where data from 692 patients were included in analysis. 5 centres participated in Phase 2 where the clinical record for 52 cases were assessed to determine whether there was avoidable or unavoidable excess corticosteroid prescribing. Case records from centres who did not participate in Phase 2 is marked as ʻmissing dataʼ. CS systemic corticosteroid, IMT Immunomodulatory Therapy.
Statistical analysis
Data were analysed using statistical software (R v3.3.3; R development Core Team 2013, University of Auckland, New Zealand) [11]. For non-parametric continuous data, between group comparisons were analysed using the Mann Whitney U test. Comparison of proportions between groups was analysed using Pearson’s Chi-squared test statistic. Alpha was set at 0.05.
Results
Phase 1
Questionnaires completed by uveitis specialists for 892 patients from eleven different centres treating uveitis and scleritis patients were entered into Phase 1 of the study, of which 667 (74.8%) fulfilled the eligibility criteria (Fig. 1). The mean age of patients was 50.5 years (range: 17–94 years). Uveitis involving the posterior segment of the eye was present in 16.5% of patients and the most common cause of sight threatening disease was cystoid macular oedema (Table 2 patient demographics and clinical characteristics).
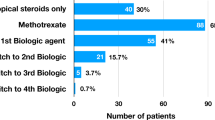
A total of 285 subjects (42.7% of eligible patients) were treated with oral or intravenous CS in the past 12 months (Table 2, Supplementary Information). We recorded several other treatments: immunomodulatory therapies (IMT) including biologic therapies (54.4%), intravitreal CS (6.4%), periocular CS (5.2%) and anti-VEGF therapies (1.7%)
Analysis of patients on CS
Out of 285 patients treated with CS in this study, 96 (33.7%) met the criteria for excess CS (Fig. 1) after exclusion of 9 cases who were treated with high dose CS for other systemic indications. Of those, 84 (29.5%) were treated with a maintenance dose of >7.5 mg prednisolone continuously for longer than a 3-month period and 23 (8.1%) were treated with more than 1 course of high dose CS within a 12-month period (Fig. 2).
Both the median CS dose at the current consultation and the median maximum CS dose in the past 12 months were significantly higher in the group treated with CS above threshold (10 mg and 40 mg respectively) than in the group treated with CS below threshold (5 mg and 10 mg, respectively) (p < 0.001, Mann–Whitney U test). Of the 96 patients treated with CS above threshold, 82 (85.4%) had active uveitis in the past 12 months, compared with only 51.9% of those treated with CS below threshold (p < 0.001, Pearson’s chi-squared test). Figure 2 shows the distribution of CS use over 12 months.
Panuveitis was the most common type of uveitis for those patients treated with CS, either above or below threshold. Of the patients treated with CS above threshold, 52.1% were also taking calcium and 19.8% were taking bisphosphonates, compared to 47.6% and 16.9%, respectively, in patients treated with sub-threshold CS (these differences were not statistically significant). We did not record vitamin D prescriptions. Cystoid macular oedema was the most common sight-threatening feature. Cystoid macular oedema and peripheral retinal vasculitis were significantly more common in patients treated with CS above threshold than those treated below threshold (p = 0.042, Pearson’s chi-squared test) and (p = 0.0288, Pearson’s chi-squared test) respectively (Table 2).
Out of 96 patients who were prescribed above threshold CS, 66 (68.8%) received immunomodulatory therapy (IMT) in the past 12 months. By comparison, a significantly lower proportion of patients (88/189, 46.6%) treated with below threshold CS, received IMT (p < 0.001, Pearson’s chi-squared test). (Table 3, Supplementary Information). Patients in both groups (above and below threshold) took biologic therapies and conventional IMTs at similar frequencies and doses respectively (Tables 3 and 4, Supplementary information). The doses of IMT reported were within standard therapeutic dosing ranges in the above threshold CS group.
Phase 2
A second uveitis expert reviewed clinical records using a semi-objective scoring matrix from a total of 52/96 patients who met criteria for above threshold CS prescribing from 5 participating centres to a) identify reasons for excess CS prescribing and b) to determine whether this might have been avoided. (Table 1). The use of excess CS was judged avoidable in 13/52 patients (25%), typically when there was an opportunity to reasonably curtail CS dose (Table 1). Of those 13 patients, 12 were treated with an excess maintenance dose of CS, as opposed to 1 treated with >1 rescue therapy of systemic CS (Table 1).
Discussion
This cross-sectional study included 667 patients, from 11 uveitis practices in the UK and is the first attempt at a country-wide analysis of CS prescribing practices, made possible by The Uveitis Clinical Study Group [8], a large clinical research network of uveitis specialists within the UK.
Overall, 42.7% of patients were treated with oral CS for non-infectious uveitis excluding acute anterior uveitis and masquerade syndromes in the 12 months preceding their entry into the study. Of patients treated with CS (n = 285) within this cohort, more than a third (38.9%) received at least one systemic course of high dose CS on one occasion over the preceding 12 months. The extent to which systemic CS is prescribed partly reflects that it is first-line therapy for ocular inflammation during induction or for flares of sight-threatening uveitis [12]. The use of intraocular CS implants was small (5.2%) over the preceding 12 months.
Using criteria for excess maintenance CS endorsed by international consensus guidance and a pragmatic criterion for excess courses of high dose steroids adopted from British Society of Gastroenterology guidelines [7], we found that a third of patients (33.7%) taking CS within this study met the criteria for excess CS prescribing for ocular inflammation. Most excess steroid prescribing was for maintenance treatment (n = 84, 29.5% of patients treated with CS). In a study on CS-induced osteoporosis in 2002 in 129 uveitis patients from five tertiary referral uveitis centres in England, treatment time with prednisolone varied from 13 weeks to 31 years. The mean dose was 13.6 mg/day (range 2.8–41) with a mean cumulative dose of 16,849 mg. Bone density was abnormally low in 44.2%, and 15.5% had osteoporosis. Bone loss correlated with total steroid dose, mean dose, duration of treatment and the presence of pre-existing risk factors [13]. In a survey of prescribing practices of 63 US physicians treating patients with uveitis published in 2011, the mean initial dose of CS prescribed was 44 mg, tapered to 34 mg/day as a maintenance dose. Interestingly, 75% of surveyed physicians in this study were unaware of consensus guidelines [14]. In our cohort, the median maximum dose of CS prescribed in the past 12 months was 10 mg for those treated below threshold (mean 23 mg) and 40 mg for those treated above threshold (mean 40 mg). At the ‘study visit’, the median dose was 5 mg for those treated below threshold and 10 mg for those treated above threshold.
We did not find evidence for under-treatment with IMTs in patients who exceeded the threshold for high dose CS with respect to dose or number of immunomodulatory agents. (Tables 3 and 4, Supplementary Information). In the UK, adalimumab is the only licensed systemic therapy for use in non-infectious uveitis, although conventional IMTs are widely used off-label. Other biologic agents are not licensed and are only available in very limited circumstances such as Behcet’s disease [15]. Our data support the contention that there are insufficient therapies routinely available to spare CS exposure in uveitis. In the US, an evaluation of insurance claims, pointed to more ocular complications in uveitis patients than age-matched controls, reflecting insufficient available therapy [16]. Thus, uveitis and scleritis remain areas of unmet need particularly compared to other inflammatory diseases.
The analysis during phase 2 of this study found that excess CS prescribing might be avoided in one quarter of cases. These results suggest that there is opportunity to reduce the proportion of those exposed to large doses of CS, particularly as part of maintenance therapy. It is possible that greater awareness among prescribers of consensus guidance, greater utilisation of steroid-sparing therapies, local therapies, and increased communication with patients may reduce exposure to CS where they are not clinically necessary.
Although there is no specific consensus guidance for courses of high dose systemic CS therapy in patients with uveitis or scleritis, a small percentage (8.1%) of the cohort receiving CS, were prescribed more than 1 course of high dose CS within a year. In the context of well-established risks of CS therapy, guidance on a desirable limit to the number of courses of high dose CS is appropriate. Attempting to limit CS to 1 high dose course per year and a maximal maintenance dose of 7.5 mg prednisolone/day would serve as a pragmatic means of minimising excess exposure to CS within uveitis practice and also reflects current prescribing for the majority of patients in the UK.
This is the first study to investigate adherence to international consensus guidance for CS prescribing. We demonstrate significant dependence on CS in uveitis patients at maintenance doses of more than a dose of 7.5 mg/day prednisolone and identify opportunity for reduction in CS exposure. We also recommend a modification of current guidelines to include a maximum of 1 high dose CS course per year. The high rate of concomitant use of immunomodulatory therapy in those meeting the criteria for excess systemic CS exposure, suggests that in some cases, a higher dose of CS may be necessary due to inadequate control of intraocular inflammation despite existing immunosuppressive strategies. This underlines the need for greater availability of therapies to treat ocular inflammation.
The strengths of this study were that: a large number of consecutive uveitis patients were included, from multiple centres, data were collected during the preceding 12 months and reflect prescribing practices in principally tertiary uveitis centres in England. A possible limitation of this study is that the 6-week period of patient enrolment may have been too short, and a longer window would have generated a larger cohort of patients that could have been more representative of clinical practice. The study did not mandate how consecutive uveitis patients were identified, which varied between sites, and may have introduced bias if patients were missed. It is possible that CS prescribing practice within non-specialist centres and in other countries may differ from the findings in this study and that our findings are an underestimate of excessive corticosteroid prescribing.
Using a national clinical network of uveitis specialists [8], we were able to report prescribing practices for CS, a medication class which is associated with both a poor tolerability profile in patients and significant long-term morbidity. Our data reflects the role of systemic CS in the current management of chronic non-infectious uveitis and offers insights into both adherence to existing CS prescribing guidance and the clinical settings in which prescribing decisions are made. Using a target maximum maintenance dose of 7.5 mg/day, or equivalent, of prednisolone, which is consistent with international consensus guidelines [5], and a pragmatic target of no more than a single rescue treatment of CS over a 12-month period, about one third of patients received excess CS. A closer assessment of clinical decision-making suggests that there may be opportunity to reduce excess CS prescribing in a quarter of cases. This study also highlights that uveitis remains an area of unmet medical need, where CS may be over-utilised as a means of reducing the risk of sight loss in the absence of a sufficient range of effective therapies.
Summary
What was known before
-
Corticosteroids are widely used for the treatment of uveitis and scleritis and are associated with a poor tolerability profile in patients and significant long-term morbidity.
-
International consensus guidelines recommend a maximum target of 7–10 mg, or equivalent, of prednisolone per day.
What this study adds
-
This study offers insight into the adherence to existing CS prescribing guidance, with one third of patients receiving excess CS for uveitis or scleritis.
-
There may be opportunity to reduce excess CS prescribing in a quarter of cases.
-
Uveitis remains an area of unmet medical need, where CS may be over-utilised as a means of reducing the risk of sight loss in the absence of a sufficient range of effective therapies.
References
Liu D, Ahmet A, Ward L, Krishnamoorthy P, Mandelcorn ED, Leigh R, et al. A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy. Allergy, Asthma Clin Immunol. 2013. https://doi.org/10.1186/1710-1492-9-30.
Wei L, MacDonald TM, Walker BR. Taking glucocorticoids by prescription is associated with subsequent cardiovascular disease. Ann Intern Med. 2004. https://doi.org/10.7326/0003-4819-141-10-200411160-00007.
Kremer JM. The CORRONA database. Autoimmun Rev. 2006. https://doi.org/10.1016/j.autrev.2005.07.006.
Jabs DA, Rosenbaum JT, Foster CS, et al. Guidelines for the use of immunosuppressive drugs in patients with ocular inflammatory disorders: Recommendations of an expert panel. Am J Ophthalmol. 2000. https://doi.org/10.1016/S0002-9394(00)00659-0.
Dick AD, Rosenbaum JT, Al-Dhibi HA, et al. Guidance on Noncorticosteroid Systemic Immunomodulatory Therapy in Noninfectious Uveitis: Fundamentals Of Care for UveitiS (FOCUS) Initiative. Ophthalmology. 2018. https://doi.org/10.1016/j.ophtha.2017.11.017.
Hoes JN, Jacobs JWG, Boers M, et al. EULAR evidence-based recommendations on the management of systemic glucocorticoid therapy in rheumatic diseases. Ann Rheum Dis. 2007. https://doi.org/10.1136/ard.2007.072157.
Lamb CA, Kennedy NA, Raine T, et al. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut. 2019. https://doi.org/10.1136/gutjnl-2019-318484.
Uveitisstudygroup.org. 2018. Uveitis National Clinical Study Group. http://www.uveitisstudygroup.org/.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009. https://doi.org/10.1016/j.jbi.2008.08.010.
Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019. https://doi.org/10.1016/j.jbi.2019.103208.
R Development Core Team 3.0.1. A language and environment for statistical computing. R Found. Stat. Comput. 2013.
Rothova A. Corticosteroids in uveitis. Ophthalmol Clin North Am. 2002. https://doi.org/10.1016/S0896-1549(02)00023-8.
Jones NP, Anderton LC, Cheong FM, Whallet A, Stanford MR, Murray PI, et al. Corticosteroid-induced osteoporosis in patients with uveitis. Eye. 2002. https://doi.org/10.1038/sj.eye.6700163.
Nguyen QD, Hatef E, Kayen B, MacAhilig CP, Ibrahim M, Wang J, et al. A Cross-sectional study of the current treatment patterns in noninfectious uveitis among specialists in the United States. Ophthalmology. 2011. https://doi.org/10.1016/j.ophtha.2010.03.029.
Nguyen QD, Merrill PT, Jaffe GJ, et al. Adalimumab for prevention of uveitic flare in patients with inactive non-infectious uveitis controlled by corticosteroids (VISUAL II): a multicentre, double-masked, randomised, placebo-controlled phase 3 trial. Lancet. 2016. https://doi.org/10.1016/S0140-6736(16)31339-3.
Dick AD, Tundia N, Sorg R, Zhao C, Chao J, Joshi A, et al. Risk of ocular complications in patients with noninfectious intermediate uveitis, posterior uveitis, or panuveitis. Ophthalmology. 2016. https://doi.org/10.1016/j.ophtha.2015.10.028.
Acknowledgements
Dr Timothy Raine, Addenbrooke’s Hospital, The Uveitis National Clinical Study Group.
Funding
Fight for Sight funds the Uveitis National Clinical Study Group. Dr Srilakshmi Sharma receives funding from the Medical Research Council (grant number: MR/T024682/) and the National Institute for Health Research.
Uveitis National Clinical Study Group
Lorna Leandro1, Nicholas Beare2, Kanchan Bhan3, Philip I. Murray4, Colm Andrews5, Erika Damato6, Alastair K. Denniston7, Nitin Gupta8, Periyasamy Kumar9, Archana Pradeep10, Fahd Quhill11, Adam Ross12, Amira Stylianides2, Srilakshmi M. Sharma13, Tasanee Braithwaite14, Amy Price15, Claire Arthur15
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Study Attribution Statement
SMS: lead author, study design, data interpretation, drafted and edited manuscript; LL: coordinated study, data analysis, contributed to the manuscript; NB: contributed to manuscript, study investigator; KB: contributed to manuscript, study investigator; PIM: manuscript review, study investigator; CA: statistical support; ED: study investigator; AKD: study investigator; NG: study investigator; PK: study investigator; AP: study investigator; FQ: study investigator; AR: study investigator; AS: study investigator.
Conflict of interest
SMS: Paid advisory boards for Alimera Sciences, Gilead, Abbvie and Allergan; NB: paid advisory boards for Alimera Sciences and Gilead. NB’s institution has received funds from Allergan.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the Uveitis National Clinical Study Group are listed below Acknowledgements.
Supplementary information
Rights and permissions
About this article
Cite this article
Leandro, L., Beare, N., Bhan, K. et al. Systemic corticosteroid use in UK Uveitis practice: results from the ocular inflammation steroid toxicity risk (OSTRICH) study. Eye 35, 3342–3349 (2021). https://doi.org/10.1038/s41433-020-01336-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01336-6