Abstract
Objectives
To evaluate the safety, efficacy, and feasibility of an endoscopic transconjunctival inferior fornix and precaruncular approach for repair of combined orbital medial wall and floor fractures involving the inferomedial strut.
Methods
A retrospective study was performed in 84 patients with combined orbital medial wall and floor fractures involving the inferomedial strut. All patients underwent surgery by endoscopic transconjunctival inferior fornix and precaruncular approach. A large polyester mesh plate was implanted to cover the fracture defect. The enophthalmos, diplopia, and surgical complications were evaluated pre- and postoperatively. Patients were followed for at least 6 months.
Results
A total of 84 patients (55 men and 29 women) with a mean age of 36.88 ± 12.95 years were included in this study. Preoperatively, all 84 patients had an enophthalmos >2 mm, and the mean exophthalmometry measurement was 11.6 ± 2.14 mm. Diplopia was presented in 33 patients. Postoperatively, good symmetry was acquired in 81 of 84 patients, with a mean improvement of 3.02 ± 0.99 mm in the enophthalmos (P < 0.05). Recovery from diplopia occurred in 32 of 33 patients. A new onset of diplopia occurred postoperatively in 13 of the remaining 51 patients, only to recover spontaneously after 1 month. One patient suffered retrobulbar hemorrhage after surgery and was cured by conservative therapy. No other serious complications occurred.
Conclusions
The endoscopic transconjunctival inferior fornix and precaruncular approach is a promising management technique for combined orbital medial wall and floor fractures involving the inferomedial strut.
Similar content being viewed by others
Background
Isolated orbital floor and medial wall fractures occur frequently. Pain, diplopia, and enophthalmos are the most common presenting symptoms. The main aim in treating orbital fracture is to reconstruct the orbital anatomy, prevent from late functional and esthetic problems. Orbital reconstruction surgery of orbital fracture requires a precise assessment of the fracture extent and restoration of the orbital anatomical structure. Compared with isolated orbital medial wall or floor fracture, combined orbital floor and medial wall fractures (COF-MWFs), particularly those fractures involving the inferomedial strut, are more likely to be complex, and consequent treatment is even more challenging [1, 2] because of the compromised inferomedial strut between the medial wall and the orbital floor. The inferomedial strut when compromised is shown to determine the stability of the implant [3], and an unstable support may lead to an undesirable secondary change of the reconstruction, including implant migration or residual enophthalmos. Although some modified approaches have been applied to reconstruct COF-MWFs [4,5,6,7,8], few studies have been reported and surgical results were normally unsatisfactory, because of the limited exposure and absence of bony structures to support the implant [9,10,11].
Therefore, we developed an endoscopic transconjunctival inferior fornix and precaruncular approach (ETIF-PA) for the reconstruction of COF-MWFs involving the inferomedial strut. This retrospective study aimed to evaluate the safety, efficacy, and feasibility of this approach.
Methods
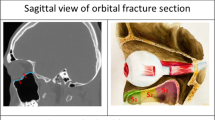
This retrospective study was performed in 103 patients who underwent repair of COF-MWFs involving the inferomedial strut by the ETIF-PA at the Eye Hospital of Wenzhou Medical University between July 2015 and December 2019. The study followed the principles of the Declaration of Helsinki and was approved by the local ethics committee (Medical Ethics Committee, Wenzhou Medical University, Wenzhou, China). Informed consent was obtained from all patients. Preoperatively, a COF-MWBOF involving the inferomedial strut was confirmed in all patients by orbital computed tomography (CT) (Fig. 1A, B). The indications for an operation included evident enophthalmos >2 mm, persistent diplopia caused by trauma, and/or limitation of ocular motility. The enophthalmos was measured using a Hertel exophthalmometer. Diplopia was determined as double vision in the primary gaze and/or within the 30° visual field of the gaze by the Hess chart, forced duction test was performed to assess limitation in extraocular muscle motility. Patients with a combined orbital rim fracture, cranial or maxillofacial fractures, and injuries of the optic nerve, lacrimal system, or the globe were excluded. A large polyester mesh plate (Inion, Tampere, Finland; thickness 1.0 mm) was used as an implant to reconstruct the fracture defect for all patients. All patients were followed up for at least 6 months.
Surgical procedure
All surgery was performed under general anesthesia by a surgeon (WW). As previously described, a standard transconjunctival inferior fornix incision was made at the inferior margin of the tarsus, then blunt dissected through the orbital fat directly to the inferior orbital rim [12, 13]. The periorbita of the infraorbital rim was incised and raised to prepare a subperiosteal cavity. Subsequently, a standard precaruncular incision was created between the edge of the medial canthal skin and the caruncle [14, 15], and the incision was extended inferiorly to meet the conjunctival inferior fornix incision, dissecting medially and posteriorly to access the medial wall. A malleable brain spatula was inserted into the incision to retract the soft tissue, enabling identification of the posterior lacrimal crest and exposure of the adjacent periorbita. The medial periorbita was incised and elevated from the orbital medial wall to form a subperiosteal cavity, which was connected with the subperiosteal cavity of the orbital floor. Following completion of the incision and subperiosteal cavity formation, a standard 0-degree endoscope (Karl Storz, Tuttlingen, Germany) was introduced into the cavity for subsequently accurate manipulation under direct vision. The subperiosteal dissection was extended laterally, medially, posteriorly, superiorly, and inferiorly under endoscopic visualization to expose all the boundaries of the fracture, particularly its far posterior border. At the same time, an assistant inserted a thin brain spatula into the subperiosteal cavity to retract the orbital tissues. During dissection, entrapped and herniated tissues were released gently and maintained intact. Special care was taken to protect the infraorbital nerve, which may run inferiorly within or above the orbital floor, and was frequently involved with the fracture (Fig. 2A). Furthermore, the anterior and posterior ethmoid vessels were carefully identified (Fig. 2C) and cauterized to avoid uncontrollable bleeding and to facilitate further exposure. Once the entrapped and herniated orbital tissues were released, and the full boundaries of the fracture were delineated (Fig. 2B, D, E), the extent of the fracture was determined, and the size of defect was measured and recorded. Subsequently, a large polyester mesh plate (thickness 1.0 mm) was cut to fit the bony defect, and the implant was curved to copy the shape of the contralateral orbital wall. Otherwise, we cut and curved the implant according to the templet, which was designed and manufactured using three-dimensional (3D) printing technology (Fig. 3). To avoid the risk of compression of the optic nerve when the implant was placed over the bony defect, the posterior edge of implant was shaved, tapered, and slightly curved. Finally, the implant was inserted through the transconjunctival inferior fornix–precaruncular incision and covered the bony defect (Fig. 2F, G). It was important that the surgeon ensured under endoscopic vision the absence of herniated orbital tissues and that the implant was placed accurately to cover all borders of the fractures to entirely reconstruct the bony defect. Biomedical EC-ear–brain glue (Guangzhou Baiyun Medical Glue Company, Guangzhou, China) was injected between the implant and the orbital wall for fixation. Finally, the periorbit and the incision were closed using 6-0 absorbable sutures (Vicryl, Ethicon, Johnson and Johnson (Shanghai) Ltd, Shanghai, China). During the entire procedure, the pupil of the operated eye was closely monitored to look for any sign of undesired optic nerve compression.
A The infraorbital nerve involving the orbital floor fracture was identified (black arrow). B After complete reduction of the intraorbital content entrapment or herniation, the full boundary of the orbital floor fracture defect was exposed adequately. C Precise subperiosteal dissection to define and reduce the entrapped or herniated orbital tissues, in which the anterior ethmoid vessel (black arrow) was identified. D After the anterior ethmoid vessel was cauterized, full boundary of the medial wall fracture defect was exposed adequately (black arrow) after complete reduction of the intraorbital content entrapment or herniation. E The compromised inferomedial strut of the transition zone between the medial wall and the orbital floor was identified (black arrow). F, G One single large implant was placed into the subperiosteal cavity was observed to cover the full boundary of COF-MWFs stably. H The infraorbital nerve was placed under the implant without any compression (black arrow).
Postoperatively, all patients were given corticosteroids (500 mg/day) for 3 days and broad-spectrum antibiotics for 5–7 days [5, 7]. Patients were encouraged to practice their ocular motility. Patients were followed for a minimum of 6 months and the follow-up was performed at 2 weeks, 1 month, 2 months, and 6 months after surgery, and thereafter as needed. An orbital CT scan was performed at 6 months after surgery to evaluate the adequacy of reconstruction. Exophthalmometry, diplopia, and complications were determined at each follow-up.
Statistical analysis
SPSS software (version 21.0; IBM Corporation, NY, USA) was used to perform statistical analyses. A paired t-test was used to assess significance (p < 0.05) of the mean improvement in exophthalmometry pre- and postoperatively.
Results
From July 2015 to December 2019, a total of 103 patients with COF-MWFs underwent repair by the ETIF-PA. In these patients, seven patients with a combined maxillofacial fractures, and injuries of the optic nerve, lacrimal system, or the globe, five patients with incomplete clinical records, and seven patients with incomplete follow-up were excluded. Therefore, 84 patients (55 men and 29 women) with a mean age of 36.88 ± 12.95 years (range, 14–76 years) were included in this study. The right orbit was involved in 36 patients and the left orbit in 48 patients. The trauma types included violence (n = 11), traffic accidents (n = 40), falls (n = 24), and others (n = 9) (Table 1). The postoperative follow-up time ranged from 6 to 18 months. Preoperative, the COF-MWFs were demonstrated to involve the inferomedial strut by CT scan (Fig. 1A, B). This was confirmed by direct endoscopic viewing during surgery (Fig. 2E). During surgery, all boundaries of the fracture were fully exposed, and the herniated or entrapped tissues were completely freed and restored (Fig. 2A–D). A single large polyester mesh plate was implanted in all cases and was placed on the entire boundary of the fractures to completely cover the bony defects (Fig. 2F, G). This was confirmed by the orbital CT at 6 months after surgery (Fig. 1C, D).
Preoperatively, all patients (n = 84) had enophthalmos >2 mm, with a mean exophthalmometry measurement of 11.6 ± 2.14 mm; the opposite eye had a mean exophthalmometry measurement of 14.39 ± 1.91 mm. Postoperatively, 81 of 84 patients acquired good symmetry (Fig. 4), the mean exophthalmometry measurement was 14.62 ± 1.98 mm, with a mean improvement of 3.02 ± 0.99 mm in the enophthalmos (P < 0.05; Table 1). Therefore, 81 of 84 patients (96.4%) with a preoperative enophthalmos >2 mm achieved correction, and only three patients had a residual enophthalmos >2 mm. Preoperative diplopia and limitation of ocular motility were found in 33 patients (39.3%) because of entrapped or herniated orbital tissues. Six months after surgery, 32 of these patients had completely recovered, and only one patient had residual diplopia and limitation of ocular motility in the medial gaze because of partial paralysis of the medial rectus muscle. Of the other 51 patients, 13 suffered a new onset of diplopia after surgery, but recovery from these diplopia occurred spontaneously after 1 month. One patient suffered retrobulbar hemorrhage after surgery and was resolved with conservative therapy (Table 1). There were no other serious complications, including uncontrollable bleeding, implant migration, visual impairment, cerebrospinal fluid leakage, and injury of the lacrimal system.
Left column: preoperatively, the left eye presented enophthalmos (>2 mm) and normal ocular motility, the exophthalmometry of left eye was 10 mm, the exophthalmometry of right eye was 13 mm; right column: postoperatively, good symmetry was acquired, the exophthalmometry of both eye were 13 mm, and the ocular motility was still normal.
Discussion
The key elements of surgical success include adequate exposure and visualization of the entire orbital defect, atraumatic restoration of the herniated or entrapped intraorbital tissues, and reconstruction of the orbital anatomy, particularly the inferomedial strut, because the support was crucial as described above. Therefore, some combined approaches have been developed to enhance exposure, and instrumentation was used for further exposure [4,5,6,7,8]. Endoscopy has been widely applied to repair orbital fracture in previous reports [4,5,6,7,8]. The potential benefits of endoscopy include easier access and maximum and direct visualization of the fracture, in addition to equally accurate reconstruction compared with the conventional techniques [4,5,6,7,8]. The endoscopic technique is very useful in releasing entrapment or herniation of the tissues, enabling exposure of the posterior border, restoring the orbital contents, and accurate implant placement. In a previous study [7], we performed endoscopic transethmoidal and transconjunctival inferior fornix approaches for repairing COF-MWFs, and obtained considerable improvement in enophthalmos and diplopia. This approach provides more surgical views compared with conventional approaches, which allowed complete repair, no scar, and a shorter recovery time. Although the fracture defects were extensive and close to the orbital apex, the entire boundary of the COF-MWFs was exposed adequately and the entrapped or herniated tissues were repaired completely without loss. However, a nasal manipulation was necessary for this approach, such as septoplasty or partial ethmoidectomy, which may result in additional nasal complications. Therefore, Chang et al. described an endoscopic transconjunctival and transcaruncular approach to avoid a nasal operation [8]. Although previously modified approaches were advantageous, the inferomedial strut was not involved, and subsequent-suspected instability of reconstruction was more likely to occur. The reconstruction of extensive COF-MWFs involving the inferomedial strut was still very difficult. On the one hand, the incision of the above approaches was too limited to insert a sufficiently large implant to cover a large fracture defect; thus, two or more implants were needed to entirely cover the bony defect, which may increase the risk of implant migration. On the other hand, the inferomedial strut was frequently broken in patients with COF-MWFs, such that it was too weak to support multiple individual implant, and the suspected instability may lead to implant migration. Therefore, the consequent complications, including residual enophthalmos, diplopia and compression of the optical nerve, were more likely to occur.
Thus, we performed an ETIF-PA to insert a single large implant for reconstruction of extensive COF-MWFs. Compared with a transconjunctival or subciliary approach, we preferred the transconjunctival inferior fornix approach to expose the orbital floor, because it protected the orbital septum and avoided herniation, ectropion, and lid retraction, and it could be combined with a precaruncular incision for improved exposure [12]. The precaruncular incision provided an optimal and rapid dissection plane of the orbital medial wall by entering the avascular plane behind the Horner’s muscle and directly reaching the posterior lacrimal crest, with dissection posterior to the Horner’s muscle preventing damage to the lacrimal sac. This incision could also be lengthened inferiorly into the inferior conjunctival fornix to provide surgical access for a large implant [14, 15]. By entering into the subperiosteal plane through the ETIF-PA, the orbital floor and medial wall can be exposed with limited dissection, minimal blood loss, and excellent exposure. This approach not only provided direct access for adequate exposure of the fracture border and its extent, but also avoided most complications, including cutaneous scar, caruncular edema, orbital fat herniation, and injury of extraocular muscle.
The present study demonstrated that our approach may be very useful in enabling exposure of the posterior fracture border, restoring the intraorbital tissues, and placing the implant accurately. In extensive COF-MWFs, particularly when the edge of the fracture was close to the orbital apex, full exposure of the posterior border of the fracture for complete tissue release and accurate implant placement were extremely difficult. To prevent potential injury to the optic nerve, some surgeons were frequently unwilling to fully expose the posterior border. Therefore, the repair of such a fracture was imperfect [16,17,18,19]. However, in the present case series, the fracture defects were relatively wide, all boundaries of the fracture were adequately exposed, and the entrapped or herniated tissues were restored completely without loss. Surgeons were unable to absolutely confirm the absence of entrapment or herniation, because after the orbital contents were reposited and the implant was placed, the subperiosteal optical cavity was obliterated, but the visualization provided by the endoscope could overcome this problem. Furthermore, endoscopic visualization enabled confirmation that the implant covered all the borders of the fractures, particularly the posterior edge, and complete repair of the defects. Therefore, after the orbital tissues were reposited over the implant, residual entrapment or herniation was unlikely. Instead of multiple individual implants, we prefer to place a single large implant for the reconstruction of COF-MWFs. We presumed that the stabilization of a single large implant was not likely to be influenced by the inferomedial strut, thereby avoiding the instability caused by the weak support of a compromised inferomedial strut. Furthermore, a single large implant provided better integration and avoided the instability caused by probable migration of multiple implants, and may more likely have achieved the desired reconstruction. After the placement of implant, the biomedical EC-ear–brain glue was used for fixation, because the orbital floor and medial wall are usually too thin to support the screws. According to our past experience [5, 7], the glue provided reliable fixation and safety, and reduced the surgical manipulation and cost. These advantages may account for the improvement of enophthalmos and diplopia in the present case series when compared with previous studies [9,10,11].
During the surgery, particular attention should be paid to prevent injury of the optic nerve, lacrimal system, and infraorbital nerve. For large COF-MWFs, particularly when the posterior border is close to the orbital apex, the fracture border should be identified before dissection, and all manipulation must be performed gently. It is crucial that the posterior edge of implant is shaved, tapered, and slightly curved to avoid the risk of migration into the orbital apex or compression of the optic nerve. Then, the implant is carefully placed to cover the fracture defect under endoscopic visualization. The pupil of the operated eye should be closely monitored during the procedure, which is a significant indicator for optic nerve injury. To avoid lacrimal injury, a lacrimal probe could be placed into the lacrimal canal for protection, and the dissection plane should be directed toward the posterior lacrimal crest and through the avascular surgical plane behind the Horner’s muscle [12]. The infraorbital nerve traverses the orbital floor in the infraorbital sulcus before dividing into the orbital floor near the rim and exits the orbit through the infraorbital foramen. When patients present with facial hypoesthesia, and the infraorbital sulcus is involved with the fracture on the preoperative CT image, the fracture may interfere with the infraorbital nerve. Any dissection near the nerve should be performed with care to avoid injury (Fig. 2H). Fortunately, owing to the advantages of this approach, and our precaution and experience, we have never experienced a major complication. Therefore, we believed that the ETIF-PA is a safe approach for the reconstruction of COF-MWFs.
With advances in 3D-printing technology and computer-aided design, precise preoperative planning for orbital reconstruction has become feasible. Computer-aided design software can be used for reconstructing preoperative 3D images of the orbit, customizing surgical planning, and manufacturing personalized implant templets [20, 21]. In the present study, we used 3D-printing technology in some patients to optimize the presurgical planning, communicate with the patients, and manufacture personalized templates (Fig. 3). During the surgery, the implant was cut and curved to duplicate the template, and was placed to accurately cover the bony defects. In all patients who underwent this procedure, satisfied reconstruction was obtained (Fig. 4). Considering this marked advantage, we believe that 3D-printing technology may provide geometric information regarding orbital fractures and allow anatomical placement of the implant with the greatest precision possible, which may be a promising way to achieve optimal reconstruction of an orbital fracture.
In summary, the surgical approach presented here appears to be an excellent approach for repair of COF-MWFs involving the inferomedial strut. Endoscopic visualization facilitated adequate exposure of all the fracture borders and, in particular, the posterior border. It also enabled restoration of all the herniated and entrapped infraorbital tissues and ensured the placement of implants over the posterior edge so that complete fracture correction could be achieved in all cases. Moreover, the instability caused by a compromised inferomedial strut was avoided by using a single larger implant. This technique resulted in excellent outcomes and low morbidity, suggesting that it is a promising alternative for this specific fracture. We believe that this method has great potential for clinical use. The present study only provided preliminary results. Limitations of our study were inevitable because of its retrospective nature, the sample size is limited, we failed to record the number of patients with herniation or entrapment, the size of the fractures, and the time of injury in our cases. Besides, this approach requires sufficient caution, technique and experience, and should be performed only after comprehensive assessment. Large-sampled, controlled prospective research studies are needed to further prove the rationality and to determine the exact surgical indication.
Summary
What was known before
-
The combined orbital floor and medial wall fractures, particularly those fractures involving the inferomedial strut, are more likely to be complex, and consequent treatment is even more challenging.
What this study adds
-
The ETIF-PA is a promising management technique for combined fracture. Endoscopic visualization facilitated adequate exposure of all the fracture borders. Moreover, the instability caused by a compromised inferomedial strut was avoided by using a single larger implant.
References
Nagasao T, Miyamoto J, Jiang H, Tamaki T, Kaneko T. Interaction of hydraulic and buckling mechanisms in blowout fractures. Ann Plast Surg. 2010;64:471–6.
Su GW, Harris GJ. Combined inferior and medial surgical approaches and overlapping thin implants for orbital floor and medial wall fractures. Ophthalmic Plast Reconstr Surg. 2006;22:420–3.
Cole P, Boyd V, Banerji S, Hollier LH Jr. Comprehensive management of orbital fractures. Plast Reconstr Surg. 2007;120 7 Suppl 2:57S–63S.
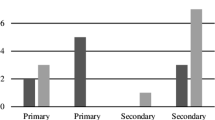
Chen CT, Pan CH, Chen CH, Shyu VB, Wu JC, Kang GC. Clinical outcomes for minimally invasive primary and secondary orbital reconstruction using an advanced synergistic combination of navigation and endoscopy. J Plast Reconstr Aesthet Surg. 2018;71:90–100.
Wu W, Jing W, Selva D, Cannon PS, Tu Y, Chen B. Endoscopic transcaruncular repair of large medial orbital wall fractures near the orbital apex. Ophthalmology. 2013;120:404–9.
Kim K, Song K, Choi S, Bae Y, Choi C, Oh H, et al. Endoscopic transnasal approach for the treatment of isolated medial orbital blow-out fractures: a prospective study of preoperative and postoperative orbital volume change. Ann Plast Surg. 2012;68:161–5.
Wu W, Yan W, Cannon PS, Jiang AC. Endoscopic transethmoidal and transconjunctival inferior fornix approaches for repairing the combined medial wall and orbital floor blowout fractures. J Craniofac Surg. 2011;22:537–42.
Chang M, Yang SW, Park JH, Lee J, Lee H, Park MS, et al. Using the endoscopic transconjunctival and transcaruncular approach to repair combined orbital floor and medial wall blowout fractures. J Craniofac Surg. 2017;28:963–6.
Cho RI, Davies BW. Combined orbital floor and medial wall fractures involving the inferomedial strut: repair technique and case series using preshaped porous polyethylene/titanium implants. Craniomaxillofac Trauma Reconstr. 2013;6:161–70.
Hur SW, Kim SE, Chung KJ, Lee JH, Kim TG, Kim YH. Combined orbital fractures: surgical strategy of sequential repair. Arch Plast Surg. 2015;42:424–30.
Nam SB, Bae YC, Moon JS, Kang YS. Analysis of the postoperative outcome in 405 cases of orbital fracture using 2 synthetic orbital implants. Ann Plast Surg. 2006;56:263–7.
Bevans SE, Moe KS. Advances in the reconstruction of orbital fractures. Facial Plast Surg Clin North Am. 2017;25:513–35.
Westfall CT, Shore JW, Nunery WR, Hawes MJ, Yaremchuk MJ. Operative complications of the transconjunctival inferior fornix approach. Ophthalmology. 1991;98:1525–8.
Moe KS. The precaruncular approach to the medial orbit. Arch Facial Plast Surg. 2003;5:483–7.
You HJ, Kim DW, Dhong ES, Yoon ES. Precaruncular approach for the reconstruction of medial orbital wall fractures. Ann Plast Surg. 2014;72:652–6.
Harris GJ. Orbital blow-out fractures: surgical timing and technique. Eye. 2006;20:1207–12.
Nowinski D, Messo E, Hedlund A. Treatment of orbital fractures: evaluation of surgical techniques and materials for reconstruction. J Craniofac Surg. 2010;21:1033–7.
Edgin WA, Morgan-Marshall A, Fitzsimmons TD. Transcaruncular approach to medial orbital wall fractures. J Oral Maxillofac Surg. 2007;65:2345–9.
Lee CS, Yoon JS, Lee SY. Combined transconjunctival and transcaruncular approach for repair of large medial orbital wall fractures. Arch Ophthalmol. 2009;127:291–6.
Oh TS, Jeong WS, Chang TJ, Koh KS, Choi JW. Customized orbital wall reconstruction using three-dimensionally printed rapid prototype model in patients with orbital wall fracture. J Craniofac Surg. 2016;27:2020–4.
Park SW, Choi JW, Koh KS, Oh TS. Mirror-imaged rapid prototype skull model and pre-molded synthetic scaffold to achieve optimal orbital cavity reconstruction. J Oral Maxillofac Surg. 2015;73:1540–53.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, G., Tu, Y., Yu, B. et al. Endoscopic repair of combined orbital floor and medial wall fractures involving the inferomedial strut. Eye 35, 2763–2770 (2021). https://doi.org/10.1038/s41433-020-01304-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01304-0