Abstract
Background/objectives
Geographic atrophy (GA) is a common cause of visual loss. The UK population prevalence is unknown. We studied GA prevalence, characteristics, and associations in an elderly UK population.
Methods
Masked grading of colour fundus photographs from 3549 participants in the cross-sectional study of Bridlington residents aged ≥65 years. GA size, shape and foveal involvement were correlated with demography and vision.
Results
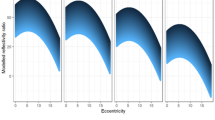
GA was detected in 130 eyes (101 individuals) of 3480 participants with gradable images (prevalence 2.90%; 95% CI 2.39–3.52 either eye), was bilateral in 29/3252 subjects (0.89%, 95% CI 0.62–1.28) with bilateral gradable photos, with mean age of 79.26 years (SD 6.99, range 67–96). Prevalence increased with age, from 1.29% (95% CI 0.69–2.33) at 65–69 to 11.96% (95% CI 7.97–17.50) at 85–90 years. Mean GA area was 4.51 mm2 (SD 6.48, 95% CI 3.35–5.66); lesions were multifocal in 47/130 eyes (36.2%; 95% CI 28.4–44.7). Foveal involvement occurred in 41/130 eyes (31.5%; 95% CI 24.2–40.0). In eccentric GA, mean distance from circumference to fovea was 671μm (SD 463; 95% CI 570–773). Older age (OR 1.10/year increase; 95% CI 1.06–1.14), RPD (OR 1.87; 95% CI 1.10–3.19) and large drusen/RPD ≥ 125 μm (OR 6.16; 95% CI 3.51–10.75) were significantly associated with GA in multivariate analysis. GA lesions (18/31 eyes; 58%; 95% CI 40.7–73.6) had U-shape configuration more frequently in RPD subjects than those without (9/99 eyes, 9.1%; 95% CI 4.66–16.6) (p = 0.0001).
Conclusion
GA, commonly solitary and eccentric, occurred in the perifovea. However, one third of GA eyes had foveal and bilateral involvement. Possible association of RPD with GA phenotype exists. Population multimodal imaging studies may improve understanding further.
Similar content being viewed by others
Introduction
Geographic atrophy (GA) is the late stage of non-neovascular AMD (non-nAMD). While nAMD is the commonest cause of severe sight loss, GA accounts for 20% of AMD blindness [1,2,3]. GA is characterised by areas of well-defined loss of retinal pigment epithelium (RPE)/underlying choriocapillaris, such that larger choroidal vessels become visible. Gass originally applied the term to the late manifestation of nAMD, where areas of atrophy occurred with enlargement towards the fovea [4]. However, recent evidence suggests spread appears faster peripherally [5]. Risk factors for GA and nAMD are similar, but unlike nAMD, no treatments currently exist for GA.
Visual loss from GA is profound with foveal involvement, whilst foveal-sparring GA often remains asymptomatic. In GA, visual acuity (VA) measurements do not adequately represent visual impairment, and difficulties associated with daily tasks [6,7,8,9,10]. Individuals with foveal-sparring GA may have reduced reading speed, and magnification is sometimes detrimental as text becomes too large to avoid pericentral scotomas. It has been suggested treatments aimed at slowing GA progression would less likely benefit eyes with large lesion size (≥17.5 mm2) [11]. As such, quantifying population GA frequency, along with lesion characteristics, including area, frequency of foveal involvement and/or distance from fovea, are important in estimating disease burden, and potential number of treatable patients.
GA prevalence/incidence has been studied in populations outside the UK [12,13,14,15]. Large natural history population based studies, including the Beaver Dam Eye Study (BDES) [16] and Blue Mountains Eye Study (BMES) [17] are available and supplemented with hospital based cohorts [3, 6, 9, 17,18,19,20]. However, there is a paucity of detailed UK studies on GA, except our earlier report of a prevalence of 2.5% in individuals aged ≥65 years [21].
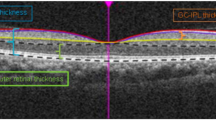
With multimodal imaging, GA is recognised as more heterogeneous than previously reported. Different phenotypes are described, including the ‘diffuse-trickling’ subtype identified with fundus autofluorescence (FAF) [22], which appears associated with reticular pseudodrusen (RPD) which are significantly associated with AMD [23,24,25,26]. Similarly, single round vs. multifocal lesions are described, whilst in subgroups of GA patients, coalescence of atrophic areas may form ‘horseshoe’, ‘U’ or later ‘ring’ configurations [5, 6] (Fig. 1). Foveal-sparing GA, with late central vision involvement has been described [3, 5, 6]. Xu et al. reported an almost universal presence of RPD in multilobular GA, with lobule enlargement into RPD areas [25]. Multilobular GA appears more prevalent in patients with RPD [25, 26]. Progression rates appear higher in eyes with multilobular GA or large initial area [24].
The preserved fovea and surrounding retina, although not affected by the GA, has diffuse and widespread hyperpigmentary changes. The rim of the GA lesion has a cuff of hyperpigmentary changes. The U-shape of the GA mirrors that of the known topographical distribution of RPD in the fundus. Features of age-related choroidal atrophy, including peripapillary atrophy and rarefaction of the fundus are also seen, with few visible choroidal vessels between the optic disc and fovea. Outside the GA, there are no large drusen, but a predominance of RPD.
GA phenotypic and size variations reportedly have different prognosis [7, 9, 11, 22, 27, 28]. However, minimal data exists on prevalence of different phenotypes and other associated phenomena from population based studies [29,30,31].
The present study investigated GA characteristics of eyes in the Bridlington Eye Assessment Project (BEAP) population cohort. We report GA prevalence, area, distance from the fovea, phenotypic characterisation, perilesional area analysis, and VA. We explore relationships between GA and RPD, in order to inform potential treatment load in the UK and elsewhere.
Methods
The BEAP study methodology, including image acquisition/analysis has been reported elsewhere [21]. To summarise, this was a single-centre population based prevalence study in an elderly population ≥65 years, using clinical examination and digital imaging. All individuals registered with a General Practitioner in Bridlington and ≥65 years were eligible. Subjects known to be moving during the study, those registered blind/partially sighted, bed bound or with dementia were excluded. All participants were interviewed by a research nurse, and examined by trained optometrists. Non-stereoscopic mydriatic fundus photography was performed. Each eye had 30° colour fundus photograph (CFP) taken centred on the macula. Local ethics committee approval (Ref no. PB/RH/02/288) was obtained. Research adhered to the tenets of the Declaration of Helsinki. All subjects provided informed consent.
Masked image grading was performed using the International Classification System of AMD by a single ophthalmologist (CW) who was trained in image grading at the Central Angiographic Reading Facility, Belfast, Northern Ireland. Image review and adjudication proceedings were as previously described [21].
GA was diagnosed in the presence of a roughly round/oval sharply demarcated area of RPE loss, ≥175 µm in diameter, within the ETDRS grid, with at least two of the following features: scalloped edges, visible choroidal vessels (more prominent than in the surrounding areas) and well-defined margins in keeping with CFP clarity. Where GA was contiguous with peripapillary atrophy, the lesion was not graded as GA. Any eye with combined GA and nAMD was graded as the latter. If doubt existed as to whether lesions resembled GA or other pathology (diabetic retinopathy, pathological myopia, chorioretinitis or laser burns), it was not graded as GA. All BEAP data was reviewed retrospectively for GA subjects ensuring none had recorded histories of diabetic retinopathy/previous macula laser, making mis-classification unlikely.
Digital images were analysed using IMAGEnet 2000 programme. GA area was outlined and measured (mm2) using the proprietary draw tool to trace the circumference. Digital enhancement was permitted if margins were not easily identified within certain regions, by reduction of colour channels to increase contrast allowing more accurate margin identification. GA was categorised as solitary with one isolated area of RPE loss and multifocal with more than one non-contiguous area of RPE loss (Fig. 2). If GA spread circumferentially around the fovea with a pattern subjectively appearing to resemble a horseshoe shape, it was recorded as U-shaped GA as opposed to round (Fig. 1). Lesions were categorised regarding foveal involvement and recorded as eccentric where the GA did not encroach the fovea. The shortest linear distance from GA circumference to the fovea were measured (μm). GA perilesional areas were assessed for pigmentary changes and subjective observations recorded with free text. GA eyes were assessed for the presence/absence of RPD, which were considered present if there was a definite reticular pattern of round/oval yellow-white lesions that formed an ill-defined network of broad, interlacing ribbons. CFP was graded initially without digital alteration, and subsequently adjusted to the red free and the blue channels for RPD identification. After image grading, LogMAR VA (corrected with current glasses and pinhole) were correlated for each eye. The presence of large drusen (≥125 μm) was recorded, which could include large conventional drusen or RPD.
Data were entered and checked with internal quality control and discrepancies corrected. Statistical analysis was performed using Stata 12.0 (StataCorp, College Station, TX, USA). Prevalence of GA was calculated as percentages of the total population with cases defined as being present in either eye. χ2 tests were used to assess the significance of univariate associations. All P values of <0.05 were considered statistically significant. Logistic regression models were used to determine the independence of potential risk factors. All the statistical tests were two sided at the 5% significance level.
Results
Of 3480 participants with gradable photographs in at least one eye, 101 persons had GA in either eye, giving a prevalence of 2.90% (95% CI 2.39–3.52) in this population of ≥65-year olds. GA was present in 130 eyes, including 67 right eyes (2.00%, 95% CI 1.58–2.54) and 63 left eyes (1.86%; 95% CI 1.45–2.38) (Table 1), and in more females than males (57 subjects [56.4%] vs. 44 subjects [43.6%]). Gender specific prevalence did not differ, at 2.94% (95% CI 2.27–3.79) in females and 2.86% (95% CI 2.13–3.83) in males. The age of GA subjects ranged from 67 to 96 years, with a mean of 79.26 (SD 6.99, 95% CI 77.88–80.64), and prevalence increasing with age (Table 1). Increasing age was associated with increased likelihood of GA in either eye (OR 1.10, 95% CI 1.06–1.14, per year increase) after adjusting for RPD and large drusen ≥125 μm.
GA was bilateral in 29 (28.7%) of 3252 with gradable photographs in both eyes, a population prevalence of 0.89%, (95% CI 0.62–1.28). Fourteen (14) GA subjects (13.9%) had contralateral nAMD, whilst another had contralateral peripapillary choroidal neovascularization (0.99%). BCVA ranged from LogMAR −0.1 to perception of light, depending on GA location (Table 2). Among eyes with vision better than LogMAR 1.0 (Snellen 6/60) mean VA was 0.35 (95% CI 0.30–0.40). Nineteen (19) of 130 GA eyes (14.6%; 95% CI 9.45–21.78) had LogMAR VA of 1.0 or worse. Mean VA for eyes with extrafoveal GA was 0.29 (95% CI 0.23–0.35).
Mean GA area for right and left eyes were 5.28 mm2 (SD 7.27; 95% CI 3.40–7.16) and 3.72 mm2 (SD 5.27; 95% CI 2.35–5.10) respectively; mean area was 4.51 mm2 (SD 6.38; 95% CI 3.35–5.66) for all eyes. Nine (9) eyes had GA area ≥17.5 mm2. Multifocal GA (Fig. 2) was identified in 47 eyes (36.2%; 95% CI 28.4–44.7), with similar prevalence in right (37.3%) and left (34.9%) eyes. Mean GA area was similar in eyes with multifocal (4.03 mm2; SD 5.13) vs. solitary GA (4.75 mm2; SD 6.94), with no statistically significant difference between the groups (p = 0.56). Subfoveal GA occurred in 41 eyes (31.5%; 95% CI 24.2–40.0), including 22 right (32.8%) and 19 left eyes (30.2%). For eyes with eccentric GA, mean distance from fovea to GA circumference was 671 µm (SD 463; 95% CI 570–773) compared to 449 µm (SD 494; 95% CI 362–537) for all GA eyes (including subfoveal GA).
Of the 101 subjects with GA, 25 (24.8%; 95% CI 17.4–34.0) had RPD in either eye (p = 0.000). Amongst 44 males with GA in either eye, 10 had RPD (22.7%; 95% CI 12.7–37.2) while 15 females with GA had comorbid RPD (26.3%; 95% CI 16.6–39.1). No statistically significant difference in gender specific prevalence for GA with RPD was identified (p = 0.82). Eyes with GA and RPD were on average older than those without RPD (83.4 years [SD 5.9; 96% CI 81.0–85.9] vs. 77.9 years [SD 6.8; 95% CI 76.3–79.4], p = <0.05). RPD were associated with an increased likelihood of GA in a crude analysis (OR 6.36, 95% CI 3.91–10.35). After adjusting for age and large drusen/RPD ≥125 μm the odds ratio was 1.87 (95% CI 1.10–3.19). The presence of large drusen/large RPD ≥125 μm was associated with increased likelihood of GA (OR 6.15, 95% CI 3.51–10.75) after adjusting for age and RPD.
Among subjects with RPD, multifocal GA was more frequent (14/31 eyes; 45.2%) than in subjects without RPD (33 of 99 eyes; 33.3%), although this difference was not statistically significant (p = 0.29). GA area among subjects with RPD (5.84 mm2; SD 7.36) was greater than in those without RPD (4.15 mm2; SD 6.09) but the difference was not statistically significant (p = 0.24). The mean shortest linear distance from GA circumference to the fovea was similar for subjects with/without RPD (458 μm; SD 367 vs. 447 μm; SD 525). In 25 GA subjects with RPD in either eye, GA was subfoveal in 6 of 31 eyes (19.4%) compared to subfoveal GA in 35 of 99 eyes (35.4%) amongst 76 subjects without RPD; the difference in proportions was not statistically significant (p = 0.12).
Subjectively, GA associated with RPD often had a distinctive U-shaped appearance, with areas of either solitary or multifocal GA, often associated with more widespread hyperpigmentary/hypopigmentary RPE changes adjacent to the GA lesion/s (Figs. 1, 3). Frequently, the perilesional areas continued as diffuse hypopigmentation in a U-shape. Among subjects with RPD, the majority of GA (18 of 31 eyes; 58%; 95% CI 40.7–73.6) conformed to a U-shape configuration when combined with these perilesional hypopigmentary changes (Fig. 1). Eyes with U-shaped GA and RPD frequently appeared to share fundus characteristics of age-related choroidal atrophy. This U-shaped GA and associated perilesional changes was infrequent in subjects without RPD (9 of 99 eyes, 9.1%; 95% CI 4.66–16.6), with the difference being statistically significant (p = 0.0001). Round, non-U shaped GA was the predominant GA phenotype among subjects with no RPD (90 of 99 eyes; 90.9%; 95% CI 83.4–95.3). The association between RPD and U-shaped GA remained after adjusting for age and the presence of large drusen ≥125 μm (OR 12.31, 95% CI 4.16–36.43).
This eye does not yet have GA; there is extensive hypopigmentation that is developing in a U-pattern, as well as clumps of hyperpigmentary changes present. There is relative preservation of foveal architecture, with less pigmentary changes in the central macula. There are features of age-related choroidal atrophy with an area of scleral show between the fovea and optic disc. There is thinning of the inferior neuroretinal rim.
When eyes with subfoveal GA were excluded, mean LogMAR BCVA was worse in eyes with GA and RPD (LogMAR 0.32, SD 0.23) than those with GA but no RPD (LogMAR 0.25, SD 0.21). This difference was, however, not statistically significant (p = 0.25). Only 6.9% (9 of 130) of eyes had no/minimal morphological changes in keeping with ARM outside the area of GA, whilst 25% (33 of 130) of GA eyes had Rotterdam stage 3 outside the GA.
Discussion
Several studies have reported GA prevalence and incidence in different world populations [9, 12, 15, 16, 32,33,34]. However, robust UK prevalence data were limited. Previous figures were based on data from registrations of visual impairment [35], and reduced vision in persons over 75 years [36], supplemented with a review by Owen et al. [37], estimating GA prevalence at 2.6 and 6.7% in UK population aged >65 and >80 years respectively. This manuscript provides an updated, detailed report acquired from standardised grading of digital CFP, representing the largest UK population GA study in persons aged ≥65 years. The findings indicate prevalence increases with age, from 1.29% in the 65–69 years group, to a maximum of 15.15% in the over 90-year group, an increase that was not gender dependent. The frequent occurrence of bilateral GA in this population, and significant ARM in contralateral eyes (in persons with unilateral GA) has major implications on prognosis, posing significant potential for future bilateral visual loss.
It is clear GA is heterogeneous, but some features appear more frequently. Most GA eyes have a single area of atrophy, similar to findings from the Complications of Age-Related Macular Degeneration Prevention Trial (CAPT) (78%) [38]. The mean distance from the most proximal lesion edge to the fovea of 430 μm (SD 400) in CAPT was similar to 494 µm measured in our study. The lower rate of multifocal GA in the CAPT (22%), compared to the BEAP study (36%) is not surprising, given the lower mean age at enrolment (70.6 years CAPT study, vs. 73.4 years BEAP). Another explanation is the CAPT population, with multiple (≥10), bilateral and large (≥125 μm) drusen at enrolment may not represent community AMD populations, and included primarily early GA lesions. In the BDES, the occurrence of solitary GA at baseline was 45%. This difference may reflect the addition of a third grading category, where Klein et al. divided GA into three configurations, including single round GA, multifocal and ‘merged’ (one or more large irregular) lesions [16]. In the present report, a single large area of GA was recorded as solitary as it was felt drawing assumptions on the origin of GA, as to whether they enlarged concentrically from small round GA, or from union of multifocal areas was not plausible.
Multifocal GA is a predictor for greater progression [16, 28] as well as likelihood of foveal involvement [16]. In the BDES, multifocal GA had the greatest increase in area (12.0 mm2), whilst solitary GA had the least (2.2 mm2) [16]. This finding was repeated in the BMES [14]. Consequently, the occurrence of such configurations within populations is important for healthcare planning. Similar to the BDES, eyes with multifocal GA in this report, did not have larger mean areas when compared to solitary GA, perhaps indicating there may be sub-phenotypes of multifocal GA. Once united, multifocal lesions would be categorised as a single lesion with a large area.
Our findings support the concept GA lesions are predominantly small and parafoveal [38], although a third of eyes in this community had foveal involvement. This is an important finding given GA only causes significant VA reduction when lesions encroach the fovea. The rate of subfoveal GA in this study is higher, but not dissimilar, to that from the CAPT study [38]. Subfoveal GA occurrence was significantly higher in BMES (57%) and BDES (50%) at baseline, compared to the present study [16]. With FAF imaging, Fleckenstein et al. reported foveal sparing in 58% of eyes with a particular GA phenotype, referred to as the ‘diffuse-trickling phenotype’ [22, 39]. The CAPT study reported a 70% incidence of subfoveal GA secondary to drusenoid pigment epithelial detachments (PED) regression [38]. The presence of drusenoid PED was associated with higher risk of GA and vision reduction [38]. Similarly, other investigators report drusenoid PEDs pose particular risk of high progression rates, particularly, to foveal involving GA [40, 41]. Our results concur the presence of large drusen or RPD appear to have the strongest association with GA (OR 6.15).
In the BDES, mean GA area was 4.6 mm2 (SD 6.00) and varied with GA configuration, being similar for isolated GA (2.72 mm2 [SD 4.54]) and multifocal GA (2.02 mm2 [SD 1.91]) but significantly larger for merged GA (8.21 mm2 [SD 7.14]). The findings from the BMES are similar (5 mm2) for GA eyes at baseline [14], and replicated in the BEAP Study. The mean area of 0.57 mm2 (SD 0.75) in CAPT reflected early incident lesions [38].
The association of RPD with GA in population based studies has only been infrequently explored [17, 33, 42,43,44]. Whilst RPD has low community prevalence, including 0.7% in the BDES [42], an association with advanced AMD has been confirmed by various groups [23, 26, 28, 42, 45, 46]. Cohen et al. [47] demonstrated a high RPD prevalence of 24% in eyes with AMD with red free and blue-filter photograph analysis. In the BDES, RPD prevalence increased with age, from 0.4% in the 43–54 years’ group to 6.6% in the 75–86 years’ group [42]. Furthermore, RPD reportedly conferred an increased risk of progression to GA, in addition to drusen and pigmentary changes (Hazard ratio [HR], 4.93, p = 0.042) [48]. The Bridlington population results confirm an increased prevalence of RPD in eyes with GA, and that persons with GA and RPD are, on average, older than those without RPD. The presence of RPD is associated with GA (OR 1.87) within this Bridlington population.
Xu et al. [25] reported that RPD was almost universal in eyes with multilobular GA, and progression was highly correlated to areas with RPD [25]. In the present study, multifocal GA occurred more commonly among subjects with identifiable RPD and U-shaped GA, similar to findings from previous reports [25, 26]. Many of these lesions were likely secondary to regression of multiple drusenoid PEDs. This is not surprising, given conventional drusen are more prevalent than RPD, and drusen regression and drusenoid PEDs are established causes of GA.
RPD are more frequently found in the superior macular zone [42, 49,50,51] with a relative sparring of the fovea previously reported in eyes with AMD [51], and eyes with early/intermediate AMD [52]. In contrast, drusen have a predilection for the fovea. These finding are supported by histological reports demonstrating paucity of subretinal drusenoid deposits at the fovea, but abundance in the perifoveal region [53]. This study shows that GA configuration appears to differ between eyes with and without RPD. RPD was associated with U-shaped GA configurations, often with widespread confluent perilesional pigmentary changes reflecting the well-known macular topographical distribution of RPD.
Multifocal GA is a non-specific term and could represent the pathological process of two large regressed drusen, to several areas of GA occurring in a U-pattern associated with RPD, or a combination of mechanisms. It is suggested eyes with no RPD could still develop U-shaped GA configurations with foveal preservation. An important and infrequently explored feature remains associated perilesional areas. Subjectively in our study, many of the U-shaped GA eyes in subjects with PRD appeared to have more widespread perilesional RPE changes, including the perifoveal region.
It is hypothesised that despite the greater tendency (although not statistically significant in this study) for RPD associated GA to be foveal sparing, VA may be reduced secondary to significant pigment epitheliopathy that often involves the central macula before the development of definite centre involving GA in RPD subjects. This phenomenon requires further exploration.
The main limitation of this study is the utilisation of CFP only. Areas of GA, when small, or in pale fundi, can be difficult to identify and accurate border delineation problematic [54]. It may be difficult in parafoveal GA to identify foveal sparring. Similarly, early occult CNV without haemorrhage could be missed. Ideally, multimodal imaging, particularly FAF and SD-OCT would have confirmed the findings, affirmed fovea involvement, and provided information on integrity of retinal layers. Multimodal imaging would allow further detailed assessment of GA and perilesional areas, with possibly more sophisticated characterisation of GA phenotype, and sensitive RPD detection. There is clear need for future studies to make use of developments in imaging technologies.
The population included in this study is purely Caucasian. As such, the data presented does not provide any information on racial differences in GA, or fully represent GA prevalence in the mixed UK population. Only a minority of GA eyes in the population have large areas of atrophy over 17.5 mm2. The exclusion of participants registered as visually impaired (VI) and severely visually impaired (SVI) may well affect the prevalence and overall phenotype of GA, particularly bilateral centre involving GA described in this study. A number of persons with advanced bilateral AMD may have been excluded and as such our reported prevalence could be an underestimation. However, our earlier report suggests such exclusions may be minimal [21]. As there are several GA phenotypes at different stages of evolution, prospective, incidence studies are required to tease out aetiology. The cross-sectional design of our study prevents any inference of causality.
In conclusion, GA is predominantly solitary and eccentric, often with preservation of VA until foveal involvement. There is a clear association between GA phenotype and drusen precursor lesions. RPD appear associated with GA that is U-shaped or forms a U-shape with confluent areas of perilesional hypopigmentation that spreads around the fovea. Subjects with RPD had a trend towards a higher prevalence of multifocal GA, a larger mean GA area and a suggestion towards foveal preservation, although these differences were not statistically significant.
This study is the first to describe in detail the features of GA within a UK population. The information will be useful in the design of future clinical trials that evaluate the development or progression of GA as well as modelling the impact of GA on sight loss in the UK.
Summary
What was known before
-
Although GA prevalence from several populations has been reported, there is a paucity of detailed studies from the UK, as well as a lack of detailed population based reports of GA characteristics.
-
Foveal-sparing of GA is a recognised but poorly understood phenomenon.
-
RPD are associated with GA, but limited data exists as to whether RPD presence influences the GA characteristics in population based studies.
What this study adds
-
GA has a prevalence of 2.90% in either eye of individuals aged ≥65 year in the Bridlington population.
-
The majority of GA eyes have a single area of atrophy (64%), with a significant proportion having foveal involvement of GA (31.5%).
-
There is a possible association between GA phenotype and drusen precursor lesions.
-
There is a trend for GA in subjects with RPD to be more likely multifocal with an association of RPD with U-shaped GA and perilesional changes.
-
There is a trend for foveal preservation in eyes with RPD and GA. However, the mean VA may remain the same secondary to a diffuse, central retinal pigment epitheliopathy that appears common among in eyes with RPD and U-shaped GA.
References
Congdon N, O’Colmain B, Klaver CC, Klein R, Munoz B, Friedman DS, et al. Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol. 2004;122:477–85.
Klaver CC, Wolfs RC, Vingerling JR, Hofman A, de Jong PT. Age-specific prevalence and causes of blindness and visual impairment in an older population: the Rotterdam Study. Arch Ophthalmol. 1998;116:653–8.
Sunness JS, Gonzalez-Baron J, Applegate CA, Bressler NM, Tian Y, Hawkins B, et al. Enlargement of atrophy and visual acuity loss in the geographic atrophy form of age-related macular degeneration. Ophthalmology. 1999;106:1768–79.
Gass JD. Drusen and disciform macular detachment and degeneration. Arch Ophthalmol. 1973;90:206–17.
Schmitz-Valckenberg S, Fleckenstein M, Helb HM, Charbel Issa P, Scholl HP, Holz FG. In vivo imaging of foveal sparing in geographic atrophy secondary to age-related macular degeneration. Investig Ophthalmol Vis Sci. 2009;50:3915–21.
Sunness JS. The natural history of geographic atrophy, the advanced atrophic form of age-related macular degeneration. Mol Vis. 1999;5:25.
Sunness JS, Rubin GS, Applegate CA, Bressler NM, Marsh MJ, Hawkins BS, et al. Visual function abnormalities and prognosis in eyes with age-related geographic atrophy of the macula and good visual acuity. Ophthalmology. 1997;104:1677–91.
Sunness JS, Rubin GS, Zuckerbrod A, Applegate CA. Foveal-sparing scotomas in advanced dry age-related macular degeneration. J Vis Impair Blind. 2008;102:600–10.
Sunness JS, Margalit E, Srikumaran D, Applegate CA, Tian Y, Perry D, et al. The long-term natural history of geographic atrophy from age-related macular degeneration: enlargement of atrophy and implications for interventional clinical trials. Ophthalmology. 2007;114:271–7.
Calabrese A, Bernard JB, Hoffart L, Faure G, Barouch F, Conrath J, et al. Wet versus dry age-related macular degeneration in patients with central field loss: different effects on maximum reading speed. Investig Ophthalmol Vis Sci. 2011;52:2417–24.
Mauschitz MM, Fonseca S, Chang P, Gobel AP, Fleckenstein M, Jaffe GJ, et al. Topography of geographic atrophy in age-related macular degeneration. Investig Ophthalmol Vis Sci. 2012;53:4932–9.
Jonasson F, Arnarsson A, Peto T, Sasaki H, Sasaki K, Bird AC. 5-year incidence of age-related maculopathy in the Reykjavik Eye Study. Ophthalmology. 2005;112:132–8.
Jonasson F, Arnarsson A, Sasaki H, Peto T, Sasaki K, Bird AC. The prevalence of age-related maculopathy in iceland: Reykjavik eye study. Arch Ophthalmol. 2003;121:379–85.
Joachim N, Mitchell P, Rochtchina E, Tan AG, Wang JJ. Incidence and progression of reticular drusen in age-related macular degeneration: findings from an older Australian cohort. Ophthalmology. 2014;121:917–25.
Klein R, Klein BE, Linton KL. Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology. 1992;99:933–43.
Klein R, Meuer SM, Knudtson MD, Klein BE. The epidemiology of progression of pure geographic atrophy: the Beaver Dam Eye Study. Am J Ophthalmol. 2008;146:692–9.
Mitchell P, Wang JJ, Foran S, Smith W. Five-year incidence of age-related maculopathy lesions: the Blue Mountains Eye Study. Ophthalmology. 2002;109:1092–7.
Sunness JS, Gonzalez-Baron J, Bressler NM, Hawkins B, Applegate CA. The development of choroidal neovascularization in eyes with the geographic atrophy form of age-related macular degeneration. Ophthalmology. 1999;106:910–9.
Yehoshua Z, Rosenfeld PJ, Gregori G, Feuer WJ, Falcao M, Lujan BJ, et al. Progression of geographic atrophy in age-related macular degeneration imaged with spectral domain optical coherence tomography. Ophthalmology. 2011;118:679–86.
Klein ML, Ferris FL 3rd, Armstrong J, Hwang TS, Chew EY, Bressler SB, et al. Retinal precursors and the development of geographic atrophy in age-related macular degeneration. Ophthalmology. 2008;115:1026–31.
Wilde C, Poostchi A, Mehta RL, MacNab HK, Hillman JG, Vernon SA, et al. Prevalence of age-related macular degeneration in an elderly UK Caucasian population-The Bridlington Eye Assessment Project: a cross-sectional study. Eye. 2017;31:1042–50.
Fleckenstein M, Schmitz-Valckenberg S, Lindner M, Bezatis A, Becker E, Fimmers R, et al. The “diffuse-trickling” fundus autofluorescence phenotype in geographic atrophy. Investig Ophthalmol Vis Sci. 2014;55:2911–20.
Arnold JJ, Sarks SH, Killingsworth MC, Sarks JP. Reticular pseudodrusen. A risk factor in age-related maculopathy. Retina. 1995;15:183–91.
Marsiglia M, Boddu S, Bearelly S, Xu L, Breaux BE Jr., Freund KB, et al. Association between geographic atrophy progression and reticular pseudodrusen in eyes with dry age-related macular degeneration. Investig Ophthalmol Vis Sci. 2013;54:7362–9.
Xu L, Blonska AM, Pumariega NM, Bearelly S, Sohrab MA, Hageman GS, et al. Reticular macular disease is associated with multilobular geographic atrophy in age-related macular degeneration. Retina. 2013;33:1850–62.
Pumariega NM, Smith RT, Sohrab MA, Letien V, Souied EH. A prospective study of reticular macular disease. Ophthalmology. 2011;118:1619–25.
Sunness JS, Bressler NM, Tian Y, Alexander J, Applegate CA. Measuring geographic atrophy in advanced age-related macular degeneration. Investig Ophthalmol Vis Sci. 1999;40:1761–9.
Schmitz-Valckenberg S, Sahel JA, Danis R, Fleckenstein M, Jaffe GJ, Wolf S, et al. Natural history of Geographic atrophy progression secondary to age-related macular degeneration (Geographic Atrophy Progression Study). Ophthalmology. 2016;123:361–8.
Sarks SH. Drusen patterns predisposing to geographic atrophy of the retinal pigment epithelium. Aust J Ophthalmol. 1982;10:91–7.
Sarks JP, Sarks SH, Killingsworth MC. Evolution of geographic atrophy of the retinal pigment epithelium. Eye. 1988;2:552–77.
Grunwald JE, Pistilli M, Ying GS, Maguire MG, Daniel E, Martin DF, et al. Growth of geographic atrophy in the comparison of age-related macular degeneration treatments trials. Ophthalmology. 2015;122:809–16.
Bressler NM, Bressler SB, West SK, Fine SL, Taylor HR. The grading and prevalence of macular degeneration in Chesapeake Bay watermen. Arch Ophthalmol. 1989;107:847–52.
Joachim N, Mitchell P, Kifley A, Rochtchina E, Hong T, Wang JJ. Incidence and progression of geographic atrophy: observations from a population-based cohort. Ophthalmology. 2013;120:2042–50.
Klaver CC, Assink JJ, van Leeuwen R, Wolfs RC, Vingerling JR, Stijnen T, et al. Incidence and progression rates of age-related maculopathy: the Rotterdam Study. Investig Ophthalmol Vis Sci. 2001;42:2237–41.
Bunce C, Xing W, Wormald R. Causes of blind and partial sight certifications in England and Wales: April 2007–March 2008. Eye. 2010;24:1692–9.
Evans JR, Fletcher AE, Wormald RP. Age-related macular degeneration causing visual impairment in people 75 years or older in Britain: an add-on study to the Medical Research Council Trial of Assessment and Management of Older People in the Community. Ophthalmology. 2004;111:513–7.
Owen CG, Jarrar Z, Wormald R, Cook DG, Fletcher AE, Rudnicka AR. The estimated prevalence and incidence of late stage age related macular degeneration in the UK. Br J Ophthalmol. 2012;96:752–6.
Brader HS, Ying GS, Martin ER, Maguire MG. Complications of Age-Related Macular Degeneration Prevention Trial Research Group. Characteristics of incident geographic atrophy in the complications of age-related macular degeneration prevention trial. Ophthalmology. 2013;120:1871–9.
Fleckenstein M, Schmitz-Valckenberg S, Martens C, Kosanetzky S, Brinkmann CK, Hageman GS, et al. Fundus autofluorescence and spectral-domain optical coherence tomography characteristics in a rapidly progressing form of geographic atrophy. Investig Ophthalmol Vis Sci. 2011;52:3761–6.
Casswell AG, Kohen D, Bird AC. Retinal pigment epithelial detachments in the elderly: classification and outcome. Br J Ophthalmol. 1985;69:397–403.
Cukras C, Agron E, Klein ML, Ferris FL 3rd, Chew EY, Gensler G, et al. Natural history of drusenoid pigment epithelial detachment in age-related macular degeneration: age-related eye disease study report no. 28. Ophthalmology. 2010;117:489–99.
Klein R, Meuer SM, Knudtson MD, Iyengar SK, Klein BE. The epidemiology of retinal reticular drusen. Am J Ophthalmol. 2008;145:317–26.
Buitendijk GH, Hooghart AJ, Brussee C, de Jong PT, Hofman A, Vingerling JR, et al. Epidemiology of reticular pseudodrusen in age-related macular degeneration: the Rotterdam study. Investig Ophthalmol Vis Sci. 2016;57:5593–601.
Finger RP, Chong E, McGuinness MB, Robman LD, Aung KZ, Giles G, et al. Reticular pseudodrusen and their association with age-related macular degeneration: the Melbourne Collaborative Cohort Study. Ophthalmology. 2016;123:599–608.
Wilde C, Patel M, Lakshmanan A, Morales MA, Dhar-Munshi S, Amoaku WM. Prevalence of reticular pseudodrusen in eyes with newly presenting neovascular age-related macular degeneration. Eur J Ophthalmol. 2016;26:128–34.
Zweifel SA, Imamura Y, Spaide TC, Fujiwara T, Spaide RF. Prevalence and significance of subretinal drusenoid deposits (reticular pseudodrusen) in age-related macular degeneration. Ophthalmology. 2010;117:1775–81.
Cohen SY, Dubois L, Tadayoni R, Delahaye-Mazza C, Debibie C, Quentel G. Prevalence of reticular pseudodrusen in age-related macular degeneration with newly diagnosed choroidal neovascularisation. Br J Ophthalmol. 2007;91:354–9.
Finger RP, Wu Z, Luu CD, Kearney F, Ayton LN, Lucci LM, et al. Reticular pseudodrusen: a risk factor for geographic atrophy in fellow eyes of individuals with unilateral choroidal neovascularization. Ophthalmology. 2014;121:1252–6.
Querques G, Canoui-Poitrine F, Coscas F, Massamba N, Querques L, Mimoun G, et al. Analysis of progression of reticular pseudodrusen by spectral domain-optical coherence tomography. Investig Ophthalmol Vis Sci. 2012;53:1264–70.
Knudtson MD, Klein R, Klein BE, Lee KE, Meuer SM, Tomany SC. Location of lesions associated with age-related maculopathy over a 10-year period: the Beaver Dam Eye Study. Investig Ophthalmol Vis Sci. 2004;45:2135–42.
Sarks J, Arnold J, Ho IV, Sarks S, Killingsworth M. Evolution of reticular pseudodrusen. Br J Ophthalmol. 2011;95:979–85.
Steinberg JS, Fleckenstein M, Holz FG, Schmitz-Valckenberg S. Foveal sparing of reticular drusen in eyes with early and intermediate age-related macular degeneration. Investig Ophthalmol Vis Sci. 2015;56:4267–74.
Curcio CA, Messinger JD, Sloan KR, McGwin G, Medeiros NE, Spaide RF. Subretinal drusenoid deposits in non-neovascular age-related macular degeneration: morphology, prevalence, topography, and biogenesis model. Retina. 2013;33:265–76.
Brader HS, Ying GS, Martin ER, Maguire MG. Complications of age-related macular degeneration prevention trial CRG. New grading criteria allow for earlier detection of geographic atrophy in clinical trials. Investig Ophthalmol Vis Sci. 2011;52:9218–25.
Acknowledgements
This research was funded in part by a Research Grant from the Macular Society UK, Andover, Hants and an unrestricted grant from Guide Dogs for the Blind, Reading, Berkshire, UK. The BEAP was funded by an unrestricted grant from Pfizer. We would also like to thank the following organisations for financial support of the Project: Pharmacia, Yorkshire Wolds and Coast Primary Care Trust, The Lords Feoffees of Bridlington, Bridlington Hospital League of Friends, The Hull and East Riding Charitable Trust, The National Eye Research Centre (Yorkshire), The Rotary Club of Bridlington, The Alexander Pigott Wernher Memorial Trust, Bridlington Lions Club, The Inner Wheel Club of Bridlington, Soroptimist International of Bridlington, and The Patricia and Donald Shepherd Charitable Trust.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wilde, C., Poostchi, A., Hillman, J.G. et al. Characteristics of Geographic atrophy in an elderly UK population—The Bridlington Eye Assessment Project (BEAP): a cross-sectional study (2002–2006). Eye 35, 1697–1704 (2021). https://doi.org/10.1038/s41433-020-01169-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01169-3
This article is cited by
-
Dry age-related macular degeneration in the Japanese population
Japanese Journal of Ophthalmology (2022)