Abstract
Objective
To evaluate the demography, aetiology and clinical course of acute onset binocular diplopia (AOBD) in patients presented as emergency and managed at the neuroophthalmology clinic of a tertiary eye care centre in Saudi Arabia.
Patients and methods
A retrospective review of the medical records of 100 consecutive patients who attended the emergency department of Dhahran Eye Specialist Hospital with isolated, AOBD. The exclusion criteria were: (a) monocular diplopia, (b) binocular diplopia accompanied with neurological deficits other than ocular muscles dysfunction and (c) thyroid eye disease. All patients were followed until resolution of the diplopia or onward referral to another specialty for further management.
Results
Male:female ratio was 2:1. Median age of the cohort was 56 years (range 18–90 years). Associated nerve palsy included: abducens nerve (n = 57 patients), oculomotor (n = 32 patients) and trochlear nerve (n = 3 patients). Microvascular ischaemia and ocular myasthenia gravis were two most common pathogenic mechanisms. AOBD resolved spontaneously in 98% of patients.
Conclusion
AOBD, though an alarming and distressing condition, carries reassuringly good prognosis in majority of patients. High risk factors for vascular disease in Middle-Eastern population are reflected in microvascular aetiology as the major cause.
Similar content being viewed by others
Introduction
Binocular diplopia is the simultaneous perception of two images of a single object and is characterized by the disappearance of the double image on closing either eye [1]. In addition to diplopia, patients may also complain of visual confusion and be found to have a disturbed vestibulo–ocular reflex, and collectively, these symptoms may be referred to as acute onset binocular diplopia (AOBD) [2]. AOBD is a manifestation of a number of neurologic and neuromuscular disorders.
Many previous published reports on diplopia were limited to specific patient cohorts such as patients presenting to a squint clinic [3], a general ophthalmic outpatient clinic [4], the orthoptic clinic [5] or patients presenting with diplopia due to a specific cause [6].
Only a few studies have examined the causes of diplopia in patients presenting to an ophthalmology emergency department with limited reporting of final outcomes [2, 7, 8].
The author, hereby, describes the demography, aetiology (with an emphasis on vascular risk factors) and outcomes of AOBD in a Middle-Eastern population.
Methods
The medical records of 100 consecutive patients with AOBD who presented to the emergency department of Dhahran Eye Specialist Hospital in Saudi Arabia were reviewed retrospectively. An approval was obtained from the local research and ethics committee. The emergency department of this hospital accepts patients referred by ophthalmologists, neurologists and general practitioners, as well as self-referred patients. All the patients underwent full blood count, erythrocyte sedimentation rate, blood sugar, haemoglobin A1c, lipid profile, renal and liver function tests. The patients less than 50 years of age were investigated for connective tissue disorders as well. A contrast magnetic resonance imaging (MRI) of brain and orbit was performed to elucidate aetiology other than microvascular ischaemia in the following subgroups of patients: age less than 50 years, partial pupil sparing and/or incomplete oculomotor nerve palsy, lack of improvement in motility disturbance after 8 weeks and those with history of malignancy or immunosuppression. Patients with third nerve palsy involving pupil were referred acutely to neurosurgery.
The information about their demographics, vascular risk factors, clinical features, imaging findings and clinical progress collated. Patients with monocular diplopia or binocular diplopia accompanied by other neurological deficits or thyroid eye disease were excluded from this study. All cases were followed in the neuroophthalmology clinic every 4 weeks until resolution of the diplopia in primary gaze. Thereafter, they were followed up every 6 weeks until the manifest deviation had resolved in all cardinal gaze positions, ptosis had resolved completely or their referral to another specialty for further management of their diplopia.
Results
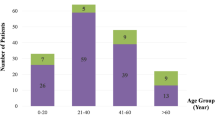
Male:female ratio was 2:1. Mean age (±SD) of cohort was 53.55 (±16.3) years (median 56 years, range 18–90 years), Fig. 1a.
a Bar diagram shows age and gender distribution of patients. X axis for age groups and Y axis for numbers. b, c Magnetic resonance imaging in a patient with right abducens nerve palsy. Axial T2 sequence shows sphenoid sinusitis (a) that resolved after antibiotic treatment (b), accompanied by resolution of abducens nerve palsy
Ocular motor cranial nerve palsy (OMCNP)
Two patients presented with AOBD due to traumatic cranial nerve paresis following road traffic accidents had oculomotor nerve palsy (n = 1) and bilateral abducens nerve palsy (n = 1).
Among non-traumatic causes, acute OMCNP accounted for in 90 patients (Table 1). Abducens nerve palsy was commonest (n = 56 patients), followed by oculomotor nerve palsy (n = 31 patients) and trochlear nerve palsy (n = 3 patients). Ocular myasthenia gravis mimicking as OMCNP was diagnosed in eight patients.
Of 90 patients of non-traumatic OMCNP, microvascular ischaemic risk factors were present in 76 patients (Table 2). Non-ischaemic causes (n = 7) included multiple sclerosis (MS), sphenoid sinusitis, Tolosa–Hunt syndrome, chronic lymphocytic leukaemia, idiopathic intracranial hypertension (IIH), cerebral venous sinus thrombosis (CVST) and pontine infarction. In a patient with sphenoid sinusitis, abducens nerve palsy resolved after antibiotic treatment (Fig. 1b, c). No underlying cause or risk factors could be identified in seven patients though AOBD resolved spontaneously in all of them. In OMCNP group, right eye was involved in 52/90 patients. The median age of microvascular ischaemic OMCNP was 57 years (range 28–90). Half of the patients with ischaemic OMCNP reported mild-to-moderate periocular pain or headache. Most patients with ischaemic oculomotor nerve palsy progressed to complete ophthalmoplegia within a week of the onset of diplopia. In partial third nerve palsy, all muscles supplied by third nerve were affected albeit to variable degree. Abducens nerve palsy presented with variable degree of impairment of abduction. The magnitude of motility limitation at the time of presentation did not have any prognostic value. Vertical diplopia with mild ptosis was the commonest presentation of ocular myasthenia gravis in this study. OMCNP resolved completely in 12–30 weeks in 98% of patients. Ischaemic OMCNP resolved earlier in patients who were younger than 50 years of age.
Five OMCNP patients had developed facial nerve palsy in past. Four patients with ischaemic OMCNP re-presented with a recurrence of AOBD due to same or different ocular motor cranial nerves paresis in the same or contralateral eye (Table 3). A patient, who had initially presented with oculomotor nerve palsy, developed palsy of abducens and trochlear nerve at 12 months and 25 months afterward. None of the patients suffered from stroke or other neurological disease during follow up.
Vascular risk factors
Among 76 OMCNP patients with ischaemic risk factors, 27 of them (35.5%) had diabetes, hypertension and hyperlipidaemia. The combination of diabetes and hypertension was seen in 20 patients (26.3%), while diabetes and hyperlipidaemia were noted in eight patients (10.5%). Diabetes as the only risk factor was found in16 patients (21%), while hypertension or hyperlipidaemia alone was seen in three (3.9%) and two of them (2.6%), respectively. Median duration of diabetes was 15 years (range 2–40 years). The glycaemic control in most of the patients with ischaemic OMCNP was poor (59/71). Microvascular ischaemic OMCNP was observed mostly in patients aged 50 years or older (64/76). In eight patients, the finding of OMCNP triggered the identification of microvascular risk factors. Among 71 diabetic patients with OMCNP, non-proliferative diabetic retinopathy was detected in 20 (28%), while five (7%) showed proliferative diabetic retinopathy. There was no diabetic retinopathy in 28 (39.4%) patients, while 18 (25.3%) patients had received pan retinal photocoagulation in past. Ischaemic heart disease was noted in nine patients. Association of the individual OMCNP with various diseases is shown in Table 4.
Neuroimaging
A total 47 patients with non-traumatic OMCNP underwent Neuroimaging. Computerized tomography (CT) with contrast and MRI with contrast, of brain and orbit, were obtained in 23 and 21 patients, respectively. In three patients, contrast was not used for neuroimaging due to renal co-morbidity. Three patients underwent additional MR angiography and one patient had a CT angiogram.
All patients with OMCNP in below 50 years age subgroup (n = 22) underwent neuroimaging. In all patients with known microvascular risk factors (n = 12), neuroimaging was normal. Among ten patients who do not have microvascular risk factor, specific aetiology was identified in six but in 4, no definitive underlying cause was found.
Twenty-five patients in above 50 years age subgroup underwent neuroimaging. In 21 who had microvascular risk factors, neuroimaging was normal. In three patients, no aetiology was identified. In one patient paresis of abducens nerve was attributed to recurrence of chronic lymphocytic leukaemia that resolved with the treatment of underlying disease.
Discussion
AOBD is a distressing and incapacitating symptom, which may be the only presentation of a range of disorders [2, 9]. Similar to previous studies, OMCNP was the most frequent aetiology of AOBD in this cohort of patients. However, this retrospective observational study reports high proportion of AOBD patients due to microvascular ischaemic OMNCP in a predominantly Middle-Eastern population presenting to a tertiary eye centre. Interestingly, ocular myasthenia gravis was the second commonest cause of in this cohort.
Perhaps, the high proportion of ischaemic OMCNP in this study is related to the high prevalence (30%) of diabetes mellitus in Saudi Arabia, which is the single most important risk factor for OMCNP [10]. It is worth highlight that poor glycaemic control is a striking feature in high number of patients with ischaemic OMCNP in this cohort.
None of the patient in this study was diagnosed with giant cell arteritis [11]. Unlike higher incidence of vertical diplopia or orbital pulley disorders reported by Kawai et al., these findings were not noticed in this cohort [12]. Similar to the previous reports involving Caucasian and Chinese ethnicities, OMCNP was more common among males in Arabic population [13].
Among patients with OMCNP, the abducens nerve tends to be affected most commonly [2, 14]. The reason for this observation remains poorly understood. The area and number of myelinated nerve fibres perfused by one endoneurial microvessel are nerve specific; perhaps the relatively lower vascular density of abducens nerve predispose it to microvascular ischaemic damage [15]. However, previous studies have shown no consistency regarding the frequency of ischaemic OMCNP, Table 2 [2, 9, 16,17,18,19]. Similar to the observations of Al Saleh et al. [17] and Choi et al. [20] this cohort of patients showed higher prevalence of oculomotor nerve palsy as compared with that of trochlear nerve palsy. Similar predilection for ocular motor cranial nerves has been described in post-stroke OMCNP [21].
Complete recovery in the majority of patients might suggest demyelination due to nerve ischaemia as the underlying pathogenic mechanism [11]. Early resolution of ischaemic cranial nerve palsy in patients younger than 50 years of age could possibly be related to the milder microvascular changes that resulted in early recovery from ischaemic damage. Furthermore, there is lower recurrence of ocular motor nerve palsy in my cohort of patients as compared with that reported by Sanders et al. [22]. It is quite possible that lower recurrence of ocular motor nerve palsy as well as no occurrence of stroke is due to an inherent bias in this study as a result of shorter duration of follow up.
Only seven patients were categorized as having AOBD due to ‘undetermined aetiology’, that is much lower than that reported in the literature [7, 16, 23]. Ocular motor nerve palsy was sentinel event leading to the identification of microvascular risk factors in eight patients.
Routine neuroimaging in patients presenting with acute onset isolated ocular motor cranial palsy continues to be a topic of debate in the literature, especially in the presence of risk factors [11, 14]. In this study, not all the patients aged 50 years and above did undergo neuroimaging. Murchison et al., as in this study, mentioned much lower yield (abnormal findings 1/25 patients) of neuroimaging in this age group [24]. In contrast, the causative lesion was found in 6/10 patients among patients aged less than 50 years of age without any microvascular risk factor.
A very recent study by Choi et al. reported severe headache as a pointer towards causes other than microvascular ischaemia in isolated OMNP [20]. I did not observe any correlation between severity of headache and aetiology in my patient cohort.
Although there was no correlation between OMCNP and diabetic retinopathy, yet the presence of multiple microvascular risk factors (especially the combination of diabetes and hypertension) increased the risk of OMCNP. In this study hyperlipidaemia alone was observed as a possible risk factor for OMCNP.
Although this is a retrospective study from a single institution that limits its interpretation, it is the first to describe, in a large cohort, the details of aetiology and outcomes in patients presenting with AOBD in Middle-Eastern population.
The author concludes that AOBD, though an alarming and distressing condition, carries reassuringly good prognosis in majority of patients. There is a need for multicentre prospective study of AOBD to understand the natural history and treatment outcomes to evolve an evidence based practice.
Summary
What was known before
-
Aetiology of binocular diplopia.
What this study adds
-
Demography, aetiology and outcomes of AOBD.
References
Danchaivijitr C, Kennard C. Diplopia and eye movement disorders. J Neurol Neurosurg Psychiatry. 2004;75:24–31.
Comer R, Dawson E, Plant G, Acheson J, Lee J. Causes and outcomes for patients presenting with diplopia to an eye casualty department. Eye. 2007;21:413–8.
Trimble R. Diplopia as a presenting sign of neoplasia. Trans Ophthal Soc UK. 1980;100:498–500.
Nolan J. Diplopia. Br J Ophthalmol. 1968;52:166–71.
Yapp JMS. Diplopia as a presenting symptom. Br Ortho J. 1973;30:52–65.
Rush JA, Younge BR. Paralysis of cranial nerves III, IV and VI. Causes and prognosis in 1000 cases. Arch Ophthalmol. 1981;99:76–9.
MORRIS RJ. Double vision as a presenting symptom in an ophthalmic casualty department. Eye. 1991;5:124–9.
Trimble R, Kelly V. Diplopia as a presenting symptom: a prospective study. Berne: Transactions of the IV international orthoptic congress; 1979:91–4.
O’Colmain U, Gilmour C, MacEwen CJ. Acute–onset diplopia. Acta Ophthalmol. 2014;92:382–6.
Alberto G-R, Patrik S. Prevalence of diabetic retinopathy in a population of diabetics from the Middle East with microvascular ocular motor palsies. J Neuro-Ophthalmol. 2016;36:131–3.
Galtrey CM, Schon F, Nitkunan A. Microvascular Non-arteritic ocular motor nerve palsies—what we know and how should we treat? Neuro-Ophthalmol. 2015;39:1–11.
Kawai M, Goseki T, Ishikawa H, Hoshina M, Shoji N. Causes, background, and characteristics of binocular diplopia in the elderly. Jpn J Ophthalmol. 2018;62:659–66.
Kahtani ESA, Khandekar R, Al-Rubeaan K, Youssef AM, Ibrahim HM, Al-Sharqawi AH. Assessment of the prevalence and risk factors of ophthalmoplegia among diabetic patients in a large national diabetes registry cohort. BMC Ophthalmol. 2016;16:118–26.
Tamhankar MA, Biousse V, Ying G, Prasad S, Subramanian PS, Lee MS, et al. Isolated third, fourth and sixth cranial nerve palsies from presumed microvascular versus other causes: a prospective study. Ophthalmology. 2013;120:264–9.
Maeda K, Yasuda H. Histological background of susceptibility of oculomotor nerve to ischemia. J Neurolog Disord Stroke. 2014;3:1092–95.
Merino P, Fuentes D, Liano PGd, Ordónez MA. Binocular diplopia in a tertiary hospital: aetiology, diagnosis and treatment. Arch Socespoftalmol. 2017;92:565–70.
Al Saleh M, Bosley T. Microvascular cranial nerve palsies in an Arabic population. J Neuroophthalmol. 1999;19:252–56.
Chou KL, Galetta SL, Liu GT, Volpe NJ, Bennett JL, Asbury AK, Balcer LJ. Acute ocular motor mononeuropathies: prospective study of the roles of neuroimaging and clinical assessment. J Neurol Sci. 2004;219:35–9.
Murchison AP, Gilbert ME, Savino PJ. Neuroimaging and acute ocular motor mononeuropathies: a prospective study. Arch Ophthalmol. 2011;129:301–5.
Choi Kwang-Dong, Choi SeoYoung, Kim Ji-Soo, Choi Jae-Hwan, Yang Tae-Ho, Oh Sun-Young, et al. Acquired Ocular motor nerve palsy in neurology clinics: a prospective multicenter study. J Clin Neurol. 2019;15:221–7.
Rowe F, group V. Prevalence of ocular motor cranial nerve palsy and associations following stroke. Eye. 2011;25:881–7.
Sanders SK, Kawasaki A, Long-term VAP. prognosis in patients with vasculopathic sixth nerve palsy. Am J Ophthalmol. 2002;134:81–4.
Park UC, Kim SJ, Hwang JM, Yu YS. Clinical features and natural history of acquired third, fourth, and sixth cranial nerve palsy. Eye. 2008;22:691–6.
Pineles SL, Velez FG. Isolated ocular motor nerve palsies. J Binocul Vis Ocul Motil. 2018;68:70–7.
Acknowledgements
The author thanks Mr Anthony J Vivian and Mr Ajay Kumar Sharma for detailed reading, editing and helpful comments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kumar, S. Acute onset binocular diplopia: a retrospective observational study of 100 consecutive cases managed at a tertiary eye centre in Saudi Arabia. Eye 34, 1608–1613 (2020). https://doi.org/10.1038/s41433-019-0705-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-019-0705-7
This article is cited by
-
Diplopia: characteristics and etiologic distribution in a referral-based university hospital
Journal of Neurology (2023)