Abstract
Purpose:
Childhood blepharoptosis may cause cosmetic and functional problems in children, but there is a paucity of studies about its epidemiology. This study aimed to investigate the prevalence of childhood blepharoptosis and associated risk factors in a representative Korean population.
Methods:
This cross-sectional nation-wide study analysed the data set acquired from the Korea National Health and Nutrition Examination Survey 2008–2012. A total of 8218 children aged 3–18 years were included. The prevalence of childhood blepharoptosis, defined as a margin reflex distance (MRD) of < 2 mm in either eye, was estimated, and the risk factors were identified using multivariate logistic regression analysis.
Results:
The mean age of participants was 11.3 ± 0.1 years, and 52.8 ± 0.6% were boys. The overall prevalence of childhood blepharoptosis in Korea was 8.0% (95% CI, 6.9–9.1%). Boys exhibited a higher prevalence of blepharoptosis than girls at most of ages. Levator function increased with age in the normal general population. The proportion of subjects exhibiting MRD1 ≥ 4.0 mm also increased significantly with age (p < 0.001). Male gender, higher body mass index, and urban residency were significantly associated with childhood blepharoptosis.
Conclusions:
The prevalence of childhood blepharoptosis is higher in urban obese boys. The increase of levator function with age should be considered in evaluations of childhood ptosis.
Similar content being viewed by others
Introduction
Blepharoptosis is abnormal low-lying of the upper eyelid over the eye [1]. It exhibits varying degrees of severity, and is one of the commonly encountered eyelid disorders in adult and paediatric ophthalmology clinics [2]. It generally causes mere cosmetic problems in adults, and veiling of the visual field can be corrected via surgery. In children however, blepharoptosis can cause functional impairment, as well as a cosmetic deficit [3]. Strabismus, amblyopia, and permanent reduction of visual acuity can be associated with childhood blepharoptosis [3,4,5]. Moreover, childhood blepharoptosis is clinically more challenging to manage than adult blepharoptosis because ophthalmic examinations are sometimes inaccurate due to poor cooperation and surgical correction usually requires general anaesthesia in children.
Although many previous studies have investigated childhood blepharoptosis, most of them have focused on surgical techniques and treatment results [6, 7]. Few studies have investigated the epidemiology of childhood blepharoptosis, and its prevalence and associated risk factors are not clearly established in the literature [8]. Although the correlation between systemic diseases and paediatric ptosis has been raised, the association is yet to be elucidated [3].
In the current study, we investigated the prevalence of childhood blepharoptosis and associated risk factors using nation-wide, population-based, cross-sectional data derived from South Korean children, on behalf of the Epidemiologic Survey Committee of the Korean Ophthalmological Society. A secondary aim of the study was to evaluate changes in margin reflex distance (MRD) and levator function (LF) with age. To the authors’ knowledge, this is the first population-based study on the prevalence of blepharoptosis in Asian children.
Materials and methods
Study population
The present study utilised the data set acquired from the Korea National Health and Nutrition Examination Survey (KNHANES), which is conducted annually by the Korea Centre for Disease Control and Prevention (KCDC) to examine the health and nutritional status of the Korean population [9]. The KNHANES is a nation-wide cross-sectional survey issued to ~4000 households annually using a stratified complex sampling method [9]. Details of the design and methodology of the KNHANES have been described previously [10]. Ophthalmologic examinations were only performed from 2008 to 2012, and thus this study analysed the data set acquired during that period, on behalf of the Epidemiologic Survey Committee of the Korean Ophthalmological Society. The current study was conducted in accordance with the tenets of the Declaration of Helsinki. Written informed consent was obtained from the legal guardians of all participants included in the survey. The protocol of the KNHANES was approved by the Institutional Review Board of the KCDC (IRB No: 2008–04EXP-01-C, 2009–01CON-03-2C, 2010-02CON-21-C, 2011-02CON-06-C, 2012-01EXP-01-2C).
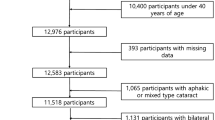
A participation flowchart pertaining to the present study is shown in Supplemental Fig. 1. Legal guardians of eligible subjects were asked to participate in health interviews and health examinations, including ophthalmological assessment. Only subjects aged ≥ 3 years underwent eyelid examination. To restrict the investigation to childhood blepharoptosis, subjects aged ≥ 19 years were excluded from the study. Thus, participants who underwent ophthalmological examination, including eyelid assessment who were aged 3–18 years were included in the study.
Assessment of blepharoptosis and levator function
MRD1 was measured as the distance from the corneal light reflex to the upper eyelid margin while relaxed, looking straight ahead, and focusing on a distant target [10]. The examiners were instructed to endeavour to exclude the effects of skin hooding or brow ptosis. If there is a skin hooding obscuring eyelid margin, MRD1 was measured lifting drooped skin to show upper eyelid margin. An examiner shone a penlight into the eyes of participants, and the distance between the upper eyelid margin and the corneal reflex was measured. MRD1 was classified into five categories: ≥ 4.0, 3.0–3.9, 2.0–2.9, 1.0–1.9, and <1.0 mm [2] Functionally significant blepharoptosis was defined as an MRD1 of <2.0 mm in either eye [1, 2, 10, 11]. Bilateral blepharoptosis was defined when MRD1 was <2.0 mm in both eyes, and unilateral ptosis was defined as MRD1 of one eye <2.0 mm and MRD1 of the other eye ≥ 2.0 mm. The LF of the upper eyelid was measured as the upper eyelid excursion from downgaze to upgaze, eliminating frontalis muscle function [2]. LF was divided into four categories: ≥ 12, 8–11, 5–7, and ≤ 4 mm [2].
Demographic, socioeconomic, behavioural, and systemic variables
Demographic, socioeconomic, and behavioural variables were evaluated using standardised self-reported questionnaires administered during the health interview component of the survey. Variables investigated included age, sex, place of residence type, and monthly household income (classified into quartiles). Height, waist circumference, and weight were measured via standard procedures, and body mass index (BMI) was calculated via the standard formula, weight in kilograms divided by height in metres squared. Visual acuity was measured at 4 m using an international standard vision chart. Refractive error was assessed using an autorefractor.
The presence of systemic diseases or comorbidities was examined via self-reporting using questionnaires. Only the comorbidities, which were investigated for children and adolescents were included in this study. The prevalences of the following diseases were investigated: atopic dermatitis, asthma, pneumonia, attention-deficit hyperactivity disorder (ADHD), urinary tract infection, congenital heart disease, epilepsy, and diabetes mellitus.
Statistical analyses
The prevalence of blepharoptosis was estimated via survey sampling weights calculated using response rate and extraction rate. The distributions of MRD1 and LF were based on the value of the eye with the worst MRD1. Data for continuous variables, including MRD1 and LF were expressed as means ± standard error. Odds ratios (ORs) were based on means with 95% confidence intervals. Data for categorical variables were expressed as percentages ± standard error. The p for linear trend about the relationship between age and MRD1 or LF was estimated.
Multivariate logistic regression analysis to construct a prediction model for childhood blepharoptosis was performed in two steps. In the first step, age-adjusted univariate logistic regression analyses of the variables investigated were conducted, and those yielding significance values of p < 0.1 were selected as candidate risk factors. In the second step, multivariate logistic regression analysis was performed using these candidate risk factors, but excluding variables with a variance inflation factor (VIF) > 5. Age and sex were entered fixedly, and a stepwise selection method was performed. A final model pertaining to the prediction of childhood blepharoptosis was constructed based on putative risk factors with p-values of < 0.05 in the multivariate logistic regression analysis. Statistical analyses were performed using R version 3.4.1 software (The R Foundation for Statistical Computing, Vienna, Austria) to account for survey weights and the complex sampling design.
Results
From 2008 to 2012, a total of 51,085 participants were invited to respond to the survey. Of these, 39,291 (76.9%) participated in the health interviews and physical examinations. The subjects included 8218 children aged 3–18 years. The mean age of these children was 11.3 ± 0.1 years, and 52.8% were boys.
Prevalence of childhood blepharoptosis
The overall prevalence of functionally significant childhood blepharoptosis in subjects aged 3–18 years in Korea was 8.0% (95% CI, 6.9–9.1%). The prevalence of bilateral blepharoptosis was 6.8% (95 CI, 6.3–7.3%). With regard to unilateral ptosis, the prevalence was 0.62% (95% CI, 0.51–0.73%) for the right eyelid and 0.58% (95% CI, 0.48–0.68%) for the left eyelid.
The prevalences of functionally significant blepharoptosis by age are shown in Fig. 1. It was lowest at aged 4 years (5.5%; 95% CI, 3.1%–7.9%) and highest in children aged 10 years (10.1%, 95% CI: 6.8%-13.5%). At all ages except 4 and 5 years, boys exhibited a higher prevalence of blepharoptosis than girls. The clinical characteristics of respondents with and without blepharoptosis are summarised in Table 1. The proportion of boys was significantly higher in children with blepharoptosis than in those without blepharoptosis (69.9% vs. 51.3%, p < 0.001). Children with blepharoptosis tended to be taller than those without blepharoptosis (148.9 cm vs. 146.1 cm, p = 0.022), and weigh more (BMI, 20.1 vs. 19.3, p < 0.001). They were also more likely to reside in a city, but that trend was not statistically significant. The presence of blepharoptosis was not significantly associated with any of the other medical conditions investigated, including atopic dermatitis, asthma, ADHD, congenital heart disease, epilepsy, and diabetes mellitus.
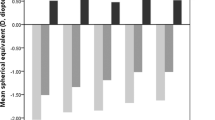
Associations between age and MRD1 and levator function
The distribution of MRD1 of the participants is presented in Fig. 2. Overall, the proportion of subjects exhibiting MRD1 ≥ 4.0 mm increased significantly with age (p < 0.001). However, the proportion of subjects exhibiting MRD1 < 2.0 mm was not significantly correlated with age. The likelihood of MRD1 ≥ 4.0 was also significantly associated with increased age in the non-ptotic group (p < 0.001). In the blepharoptosis group most subjects exhibited an MRD1 of 1.0–1.9 mm, and the overall proportion of MRD1 < 1.0 mm was 16.1 ± 1.9%. LF distribution by age is shown in Fig. 3. In the non-ptosis group, the proportion of participants with excellent LF ( ≥ 12 mm) increased significantly with age (p < 0.001), while in the blepharoptosis group LF did not exhibit any specific pattern. The proportion of participants with excellent LF ( ≥ 12 mm) was significantly lower in the ptotic population than in the non-ptotic population (31.2% vs. 69.2%, p < 0.001). Also, the proportion of participants with poor LF (≤ 7 mm) was significantly higher in the ptotic population than in the non-ptotic population (18.0% vs. 1.6%, p < 0.001).
Risk factors for childhood blepharoptosis
Supplemental Table 1 shows the results of univariate regression analyses adjusted for age. In these analyses, the factors associated with the presence of blepharoptosis with a p-value of < 0.1 included sex, urban residency, height, waist circumference, and BMI. Variables with the largest VIF of > 5, waist circumference and height, were excluded stepwise.
Table 2 shows the multivariate regression model. The final model included younger age, male sex, higher BMI, and urban residency as risk factors for the presence of blepharoptosis. Childhood blepharoptosis was significantly more prevalent in boys (OR = 2.21, 95% CI: 1.79–2.73). The adjusted OR for childhood blepharoptosis with 1-year age increase was 0.97 (95% CI: 0.94–0.99), with urban residency it was 1.66 (95% CI: 1.01–2.75), and with a 1 kg/m2 BMI increase it was 1.07 (95% CI: 1.03–1.10).
Discussion
In this large, nation-wide, population-based study, the prevalence of functionally significant blepharoptosis in childhood was 8.0% in South Korea. In the non-ptosis group, the proportions of subjects with high MRD1 and excellent LF increased with age. Multivariate regression analysis revealed male gender, higher body mass, and urban residency were significant risk factors for childhood blepharoptosis.
This is the first report to investigate the prevalence of blepharoptosis in Asian children, and it was 8.0%. This is a somewhat higher prevalence than that in previous epidemiologic reports. A cross-sectional Iranian study of 4106 children aged 7 years reported a prevalence of 1.41% [5]. An American epidemiologic study conducted in Olmsted reported that the incidence of childhood blepharoptosis was 7.9/100,000 [8]. In a community-based study conducted in Israel the reported incidence was 19.9/100,000 [3]. These disparities are probably explained by methodological differences and racial differences. In previous studies, the study populations were recruited based on medical referral systems or medical records, while in the current study a nation-wide representative sample of Koreans was used. The KNHANES used stratified, multistage, clustered sampling based on national census data to randomly select a population-based sample from across the nation [10]. Thus, the results of the present study are likely to be representative of the real prevalence of childhood blepharoptosis, and they suggest the importance of screening tests. With regard to racial differences, the vertical palpebral fissure is normally 1.5–2.0 mm smaller in Asians than in Caucasians [12, 13]. We defined blepharoptosis as an MRD1 of < 2 mm, and cases of mild blepharoptosis may explain the high prevalence of blepharoptosis in the current study.
Associations between age and MRD1 and LF were analysed in the non-ptosis group and the blepharoptosis group. In the non-ptosis group, the proportion of subjects with the highest MRD1 ( ≥ 4 mm) increased with age. This is comparable to the results of a previous study. In a European study, age-related changes in surface measurements of orbital regions in normal Caucasian children aged 2 to 16 years were investigated [14]. They reported that the rate of orbital growth was usually modest, and the palpebral fissure reached an adult level at the age of 16 years. The proportion of subjects with excellent LF ( ≥ 12 mm) increased with age in the blepharoptosis group, similar to the pattern of MRD1. Few previous studies have investigated associations between age and LF in children. Park et al. [15]. analysed LF anthropometrically in 498 normal Korean subjects aged 6 to 80 years, and reported that it peaked during the twenties. This is consistent with the results in the present study, suggesting the gradual maturation of LF in the paediatric period. Those results imply that levator muscle function is not fully developed in early childhood, and suggest that the normal range of LF should be adjusted by age in the clinical setting. In subjects with blepharoptosis, neither MRD1 nor LF exhibited a specific association with age, suggesting that the majority of the blepharoptosis group in the present study may have had congenital blepharoptosis. Further studies are needed, to generate an LF growth curve derived from ptotic eyes.
In the current study, male gender was the strongest risk factor for childhood blepharoptosis. Boys accounted for 70% of the childhood blepharoptosis group, and male gender was an independent risk factor in multivariate logistic regression analysis with an OR of 2.21. There has been controversy over whether male gender is associated with childhood blepharoptosis. Berry-Brincat and Willshaw [16] reported a higher frequency of male subjects (61.8%) in their 10-year retrospective case series. Male preponderance has also been reported in cohort studies conducted in the UK and Taiwan [6, 17]. Recent large case series from Korea also reported male dominance in congenital ptosis (1154 of 1336 patients, 63.6%). However, in the population-based cohort study reported by Griepentrog et al. [8] there was no significant gender difference in patients with childhood blepharoptosis, though there was a subtle trend (male: female = 56:44). The results of the present study suggest that male gender is strongly associated with paediatric blepharoptosis. The causal relationship between gender and paediatric blepharoptosis remains unclear. We speculate that a genetic association may exist. Only a few studies have investigated candidate genes however, such as PTOS1 and ZFH4, and no causative gene for congenital blepharoptosis has been identified [18, 19]. No large-scale gene study in Asian patients with paediatric blepharoptosis has been conducted.
The blepharoptosis group in the current study exhibited a significantly higher mean BMI. This is the first study suggesting an association between childhood blepharoptosis and weight. Paik et al. [11] previously reported that there was a strong association between blepharoptosis severity and obesity parameters in Korean adults. They hypothesised that total body fat increases may cause fatty changes of the eyelid and levator muscle, and hypertrophied orbital fat in obese subjects may have a mechanical “push-down effect” on the upper eyelid. We surmise that these hypotheses may be applicable in paediatric blepharoptosis. Although the pathogenesis of adult and childhood blepharoptosis differs, fatty changes in the levator muscle have frequently been observed in several histological studies of congenital blepharoptosis [20,21,22].
In the present study, urban residency was an independent risk factor for paediatric blepharoptosis. As this investigation was a coss-sectional study, the causal relationship is not clear. One possible explanation may relate to the fact that health during pregnancy can be affected by residential area. In several studies, conditions involving adverse environmental factors such as air pollution, exposure to smoking, and noise pollution have been significantly associated with maternal and foetal health [23,24,25,26]. Thus, urban residency may be a novel risk factor for congenital blepharoptosis.
The current study had several limitations. First, blepharoptosis subtypes were not specified. Second, there may have been measurement error among examiners, though they were repeatedly educated by oculoplasty specialists and were familiar with the examinations. The KNHANES validated the agreement rates only for the evaluation of fundus and optic disc on fundus photographs, and did not provide the validation data for inter- or intra-observer variation. Third, the exact difference of MRD1 between both eyes cannot be calculated because it was assessed as a categorical value, so we defined functionally significant ptosis when MRD1 of either eye < 2.00 mm. Fourth, because MRD1 and LF could not be recorded as continuous values, linear regression could not be performed to assess correlations. Fifth, the history of blepharoptosis repair surgery could be omitted due to the self-reporting system used to ascertain medical history. Despite these limitations, the KNHANES is a nation-wide population-based survey of the Korean population, and this study provides an important foundation for investigating the prevalence of paediatric blepharoptosis and associated factors in a large sample.
In conclusion, the prevalence of functionally significant paediatric blepharoptosis in a large Korean population-based sample aged between 3 and 18 years was 8.0%. The presence of paediatric blepharoptosis was positively associated with male gender, high BMI, and urban residency. A prospective, large population-based clinical study will be needed to determine causal relationships pertaining to these findings.
Summary
What was known before
-
There is a paucity of studies about the epidemiology of childhood blepharoptosis in the general population.
What this study adds
-
The overall prevalence of childhood blepharoptosis in Korea is 8.0%. The prevalence of childhood blepharoptosis is higher in urban obese boys. Levator function increases with age in children.
References
Rha EY, Han K, Park Y, Yoo G. Socioeconomic disparities in the prevalence of blepharoptosis in the South Korean Adult Population Based on a Nationwide Cross-Sectional Study. PLoS ONE. 2016;11:e0145069.
Kim MH, Cho J, Zhao D, Woo KI, Kim YD, Kim S, et al. Prevalence and associated factors of blepharoptosis in Korean adult population: The Korea National Health and Nutrition Examination Survey 2008-2011. Eye (Lond). 2017;31:940–6.
Nemet AY, Segal O, Mimouni M, Vinker S. Associated morbidity of pediatric ptosis—a large, community based case-control study. Graefes Arch Clin Exp Ophthalmol. 2014;252:1509–14.
Jockin YM. Blepharoptosis in childhood. Int Ophthalmol Clin. 2014;54:55–71.
Hashemi H, Nabovati P, Dadbin N, Heidari Z, Yekta A, Jafarzadehpur E, et al. The Prevalence of Ptosis and Its Association with Amblyopia and Strabismus in 7-Year-Old Schoolchildren in Iran. Strabismus. 2015;23:126–31.
Ho YF, Wu SY, Tsai YJ. Factors associated with surgical outcomes in congenital ptosis: A 10-year study of 319 cases. Am J Ophthalmol. 2017;175:173–82.
Hou D, Li G, Fang L, Li B. Frontalis muscle flap suspension for the correction of congenital blepharoptosis in early age children. PLoS ONE. 2013;8:e53185.
Griepentrog GJ, Diehl NN, Mohney BG. Incidence and demographics of childhood ptosis. Ophthalmology. 2011;118:1180–3.
Cho BJ, Heo JW, Kim TW, Ahn J, Chung H. Prevalence and risk factors of age-related macular degeneration in Korea: the Korea National Health and Nutrition Examination Survey 2010-2011. Invest Ophthalmol Vis Sci. 2014;55:1101–8.
Yoon KC, Choi W, Lee HS, Kim SD, Kim SH, Kim CY, et al. An overview of ophthalmologic survey methodology in the 2008-2015 Korean National Health and Nutrition Examination Surveys. Korean J Ophthalmol. 2015;29:359–67.
Paik JS, Jung SK, Han KD, Kim SD, Park YM, Yang SW. Obesity as a POtential Risk Factor for Blepharoptosis: The Korea National Health and Nutrition Examination Survey 2008-2010. PLoS ONE. 2015;10:e0131427.
Saonanon P. Update on Asian eyelid anatomy and clinical relevance. Curr Opin Ophthalmol. 2014;25:436–42.
Rhee SC, Woo KS, Kwon B. Biometric study of eyelid shape and dimensions of different races with references to beauty. Aesthetic Plast Surg. 2012;36:1236–45.
Hreczko T, Farkas LG, Katic M. Clinical significance of age-related changes of the palpebral fissures between age 2 and 18 years in healthy Caucasians. Acta Chir Plast. 1990;32:194–204.
Park DH, Jung JM, Song CH. Anthropometric analysis of levator muscle function. Plast Reconstr Surg. 2008;121:1181–7.
Berry-Brincat A, Willshaw H. Paediatric blepharoptosis: a 10-year review. Eye (Lond). 2009;23:1554–9.
Lee V, Konrad H, Bunce C, Nelson C, Collin JR. Aetiology and surgical treatment of childhood blepharoptosis. Br J Ophthalmol. 2002;86:1282–6.
Stein A, Kelly JP, Weiss AH. Congenital eyelid ptosis: onset and prevalence of amblyopia, associations with systemic disorders, and treatment outcomes. J Pediatr. 2014;165:820–22.
McMullan TF, Collins AR, Tyers AG, Robinson DO. A novel X-linked dominant condition: X-linked congenital isolated ptosis. Am J Hum Genet. 2000;66:1455–60.
Surve A, Sharma MC, Pushker N, Bajaj MS, Meel R, Kashyap S. A study of changes in levator muscle in congenital ptosis. Int Ophthalmol. 2019;39:1231–8.
Baldwin HC, Manners RM. Congenital blepharoptosis: a literature review of the histology of levator palpebrae superioris muscle. Ophthalmic Plast Reconstr Surg. 2002;18:301–7.
Leite CP, Schellini SA, Pellizzon CH, Marques ME, Padovani CR. [Congenital ptosis associated with fatty infiltration of levator eyelid muscle]. Arq Bras Oftalmol. 2006;69:827–9.
Svechkina A, Dubnov J, Portnov BA. Environmental risk factors associated with low birth weight: The case study of the Haifa Bay Area in Israel. Environ Res. 2018;165:337–48.
Lamichhane DK, Ryu J, Leem JH, Ha M, Hong YC, Park H, et al. Air pollution exposure during pregnancy and ultrasound and birth measures of fetal growth: A prospective cohort study in Korea. Sci Total Environ. 2018;619-620:834–41.
Gong X, Lin Y, Zhan FB. Industrial air pollution and low birth weight: a case-control study in Texas, USA. Environ Sci Pollut Res Int. 2018;25:30375–89.
Auger N, Duplaix M, Bilodeau-Bertrand M, Lo E, Smargiassi A. Environmental noise pollution and risk of preeclampsia. Environ Pollut. 2018;239:599–606.
Acknowledgements
We thank the Epidemiologic Survey Committee of the Korean Ophthalmological Society for their dedication to the design and implementation of the Korea National Health and Nutrition Examination Survey, data acquisition and verification, and for allowing public access to the data. This research was supported by the Bio & Medical Technology Development Programme of the National Research Foundation (NRF) and funded by the Korean government (MSIT) (No. NRF-2017M3A9E8033207).
Funding
This research was supported by the Bio & Medical Technology Development Programme of the National Research Foundation (NRF) and funded by the Korean government (MSIT) (No. NRF-2017M3A9E8033207).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Cho, BJ., Choi, Y.J., Shin, M.C. et al. Prevalence and risk factors of childhood blepharoptosis in Koreans: the Korea National Health and Nutrition Examination Survey. Eye 34, 1585–1591 (2020). https://doi.org/10.1038/s41433-019-0697-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-019-0697-3
This article is cited by
-
Blepharoptosis and cognitive performance: a population-based study of 1.4 million adolescents
European Journal of Pediatrics (2023)
-
Correlation between body composition and blepharoptosis in adults
Eye (2021)