Abstract
Background
To investigate factors that may affect graft dislocation after uneventful Descemet stripping endothelial keratoplasty (DSAEK), with a special focus on different donor cornea storage conditions.
Methods
All DSAEK surgeries performed during 6 years in our hospital were retrospectively investigated. Patients with previous intraocular surgeries other than cataract extraction were excluded. Donor data (age, gender, death-to-preservation time, cornea storage conditions, graft storage time, and estimated thickness of the graft) and patient information (age, gender, and indication for surgery) were noted.
Results
A total of 26 dislocations (6.6%) out of 394 DSAEK surgeries were found. The dislocation rate was considerably reduced between 2011 and 2016, due to more experienced surgeons. There was a significantly higher dislocation rate with the use of donor corneas stored in cold storage solution (12.7%) compared with organ culture solution (2.5%) (P < 0.001). During the study period, donor corneas stored in cold storage solution and organ culture solution were applied in 158 (40%) and 236 (60%) cases, respectively. There were no differences in recipient age and gender between patients who received corneas from the two storage systems, indicating a random distribution of grafts. In a multivariate analysis, only operation year (reduced rate over the years) and cold storage solution were statistically significantly associated with graft dislocation.
Conclusion
This study suggests that the type of storage solution may have a decisive role in graft dislocation in DSAEK surgery.
Similar content being viewed by others
Introduction
Endothelial keratoplasty (EK) has replaced penetrating keratoplasty (PK) for many corneal diseases such as Fuchs endothelial dystrophy, bullous keratopathy, and failed PK [1,2,3,4]. Descemet stripping endothelial keratoplasty (DSAEK) is one of the most performed EKs, where the Descemet membrane in most cases is removed and the donor tissue is prepared with an automated microkeratome. Compared with PK, EK is less invasive, induces minimal astigmatism, and results in improved and faster visual outcomes and reduced rejection rates [5, 6].
The most frequent complication after DSAEK surgery is dislocation of the graft, which is more frequent in the hands of inexperienced surgeons [7]. Much attention has been given to optimizing the surgical technique to prevent this occurrence. In a previous study [8], we showed that by letting the anterior chamber to be fully filled with air at the end of surgery for at least 1.5 h, the dislocation rate was low, and it was irrelevant whether patients were left in a supine position or not. Other strategies have been proposed, such as scraping the peripheral donor bed, venting incisions, sweeping motions on the host surface, and suturing side port incisions [9,10,11,12].
In the present study, we wanted to explore if factors other than surgical techniques could influence the dislocation rate after DSAEK. Factors such as age and gender of both the donor and the recipient, recipient diagnosis, as well as other qualities of the donor cornea, like death-to-preservation (DTP) time, estimated thickness of the graft, and different storage conditions for the donor cornea were considered prior to transplantation. These parameters have mainly been investigated in association with endothelial cell (EC) loss over time rather than in relation to dislocation rate [13, 14].
Only a few studies have compared results after corneal transplantation using donor corneas stored in different culture solutions. The procedure involved in these studies has been PK, and the clinical outcome has shown relatively similar outcomes [15,16,17,18]. However, a recent study showed a higher dislocation rate of the graft in Descemet membrane endothelial keratoplasty (DMEK) using corneas stored under cold (4 °C) short-term conditions compared with long-term organ culture conditions [19].
Access to donor corneas for transplantation has varied over the years in our hospital. In the absence of corneas from our eye bank (using organ culture storage solution), we have applied corneas from the San Diego Eye Bank in the U.S. (using short-term cold storage solution). As we have considered the two storage systems comparable, the donor corneas from the different storage solutions have been used irrespective of the recipient’s eye disease. In the past few years, increasingly number of corneas has been obtained from our local eye bank, and the need for U.S. corneas has therefore decreased.
The aim of this study was to investigate, which factor mentioned above can affect graft dislocation after DSAEK, with a special focus on the two different donor cornea storage conditions.
Methods
Study group
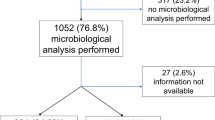
DSAEK surgery has been a well-established surgical procedure at Oslo University Hospital (OUH) since 2011. In the present study, we investigated the rate of graft dislocation from January 2011 to November 2016. In this period, we performed a total of 456 DSAEK surgeries. Fifty-seven of these cases were excluded from the study due to complicated preoperative anatomical conditions, which may increase the risk of graft dislocation, such as previous filtering surgery or presence of an anterior chamber intraocular lens [20,21,22]. In addition, four eyes with dislocation were excluded due to problems during preparation or implantation of the graft, as these problems were considered as explaining the reason for the dislocation. Of these four, three grafts were curled up on the Busin injector, and it was uncertain whether the grafts were lying with the endothelium side down in the anterior chamber, and in one patient, the graft was accidentally thinner because of lack of pressure on the artificial chamber during preparation. One patient rubbed the eye heavily postoperatively, which could have caused the dislocation, and was also excluded. Of the five patients in whom the dislocation had a reasonable explanation, two donor corneas were stored in cold storage solution and three in organ culture solution. Graft dislocation was defined as a dislocation requiring re-bubbling. Hence, a total of 394 eyes were included. From a corneal transplant registry in our department, we extracted several parameters related to the corneal graft and the patients’ pre- and postoperative findings. The registry is approved by the hospital’s Data Protection Officer and the Regional Committee for Medical and Health Research Ethics. All patients who undergo keratoplasties are registered after written consent.
Donor cornea storage conditions
Donor corneas from San Diego Eye Bank were preserved in Optisol-GS (Bausch & Lomb Inc., Irvine, CA) at 4 °C (cold storage solution), and donor corneas from our eye bank were stored in organ culture storage solution at 32 °C, containing Minimum Essential M Medium (Invitrogen, Carlsbad, CA) supplemented with Hepes, amphotericin-B, and fetal calf serum. The graft storage time (mean ± standard deviation) was 9.4 ± 1.3 days (range 6–13) in the corneas stored in a cold storage solution, and 19.2 ± 6.7 days (range 4–34 days) in the corneas stored in an organ culture storage solution.
Surgical procedure
The DSAEK procedure was performed as previously described [8] with modifications, and is briefly described here:
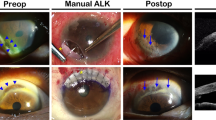
Donor preparation
The donor cornea was positioned on an artificial chamber and prepared by the surgeon in the operating theatre, using the automated lamellar keratoplasty system (ALTK; Moria SA, Antony, France). Central corneal thickness (CCT) was measured on the donor lenticule with ultrasound pachymetry (Sonogage, Cleveland, OH). If CCT exceeded 500 µm, a 350 µm head was applied, while a 300 µm head was used if CCT was below 500 µm. The epithelium was removed before the microkeratome dissection. The donor lamella was placed on a Barron punch (Barron Precision Instruments, Grand Blanc, MI) with the endothelium side up, and an 8.5 mm cut was made. The donor lenticule was covered with a storage solution while the host cornea was prepared. Graft thickness was calculated as the total CCT of the donor cornea minus the applied microkeratome of 350 or 300 µm and the stipulated epithelium thickness of 70 µm. As the size of the cap removed may vary despite the same size of the microkeratome knife, the thickness of the donor lenticule should be considered as an estimate of the graft thickness and will be referred accordingly.
Patient preparation
All surgeries were performed under retrobulbar anaesthesia and by two surgeons (LD and MS: 79% and 21% of the cases, respectively). Between 2011 and 2014, all surgeries were performed by one single surgeon (LD). From 2014, both surgeons were involved. The endothelium was removed with a Price Hook and a 90° spatula (both from Moria). Then, a 2-mm temporal and a 4-mm nasal incision were made, and an anterior chamber maintainer was placed at the 12 o’clock incision. The DSAEK Busin forceps (Moria) was advanced through the temporal incision across the anterior chamber, and the transplant was grasped from the Busin glide at the nasal wound. 10–0 Nylon sutures were used to close all three incisions. No peripheral iridectomy was performed. The intraocular pressure (IOP) was measured at the end of surgery with rebound tonometry (ICare, Revenio Group Corporation, Helsinki, Finland). The anterior chamber was left almost fully filled with air, and the IOP was aimed at ~20–30 mmHg. The patients were placed in an upright position after surgery, as we followed the procedure previously described [8]. One-and-a-half or 2 h after surgery, a slit-lamp examination was performed to measure IOP and note the position of the graft. If IOP was high, air was released from one of the incisions to acceptable values. Before the patient was released, the pupil was dilated (cyclopentolate and metaoxedrine), and it was ensured that the air bubble was above the lower edge of the pupillary margin to prevent pupillary blockage.
Postoperative follow-up
The patients were re-examined on Day 1, Day 7, and after 1 month. Later, patients were followed either by their local ophthalmologist or at our hospital.
Statistical analyses
Statistical analysis was conducted with IBM SPSS version 25.0 (IBM Corp., Armonk, NY, USA). Independent sample t-test and Pearson chi-square test were used to compare different quantitative (age, DTP, estimated graft thickness, storage time) and categorical variables (gender, diagnosis, storage solution), respectively, between patients who had graft dislocation or not. The risk of graft dislocation was also analysed, applying logistic regression to control for relevant variables. The results were presented as an Odds Ratio (OR) ± 95% confidence interval (CI). In all analyses, a significance level of 5% and two-sided significance testing were applied.
Results
Patient data
The reason for surgery was Fuchs endothelial dystrophy in 315 cases (79.9%). Other causes were bullous keratopathy (n = 30; 7.6%), re-grafts (previous DSAEK, n = 23; 5.8%, failed PK, n = 15; 3.8%, and failed DMEK, n = 7; 1.8%) or not specified (n = 4; 1.0%).
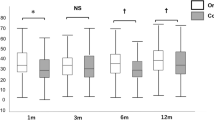
Dislocation rate
Of the 394 patients included in the study, 26 (6.6%) patients developed graft dislocation requiring re-bubbling. The dislocation rate was considerably reduced between 2011 and 2016 due to more experienced surgeons (Fig. 1). There was a significantly higher dislocation rate in corneas stored in cold storage solution (12.7%) compared with corneas stored in organ culture storage solution (2.5%) (P < 0.001). Of the 26 patients with dislocated grafts, 25 were successfully re-bubbled. Sixteen (62%) of the 26 patients with graft dislocation were re-bubbled within the 1st week. The remaining patients, except one, were re-bubbled within 2 weeks. The last patient was operated with a new DSAEK transplant 34 days postoperatively. Although anatomically attached, six patients had re-DSAEK due to failed grafts. These surgeries were performed between 1 and 13 months after the primary DSAEK procedure. Of the six patients that were re-transplanted, four belonged to the cold storage medium group and two cases to the culture medium group.
There was no statistically significant difference between the rate of graft dislocation and recipient diagnosis, donor age and gender, donor cornea DTP time, or estimated graft thickness (Table 1). In a multivariate analysis, controlling for storage solution, DTP time, different surgeons, and operation year, only cold storage solution [P = 0.006, OR 3.855 (1.469–10.114)] and years of surgery [P = 0.001, OR 0.606 (0.446–0.823)] were statistically significantly associated with graft dislocation.
Donor storage time was not included in the multivariate analysis, as this factor is basically different between the two storage methods. Since there was a significantly higher dislocation rate in the cold storage group, the storage time within this group was analysed to explore if there was an association between the length of the storage time and the risk of graft dislocation. However, we found no statistically significant differences in storage time for eyes with dislocated grafts (mean ± standard deviation); 9.5 ± 1.4 days (range 7–12), compared with eyes with no dislocation; 9.4 ± 1.3 days (range 6–13) in the cold storage group (P = 0.759). There was also no association between storage time and dislocation in the grafts stored in culture medium (P = 0.954).
Since the dislocation rate was especially high in 2011, we also performed analyses excluding patients from that year. We still found a statistically significant difference in dislocation rate between the two groups (P = 0.031).
Corneal grafts
In the study period, a total of 158 (40%) donor corneas originated from San Diego Eye Bank, stored in cold storage solution, and 236 (60%) donor corneas came from our eye bank stored in organ culture storage solution. However, the percentages from the two eye banks varied from year to year (Fig. 2).
Discussion
Graft dislocation is the most frequent complication after DSAEK and usually occurs within the first days after surgery, although occurrence at a later time has been reported [23]. Dislocation is an unfortunate incidence, possibly affecting the clinical outcome as studies have shown an increased risk of EC loss [24] and graft failure [25]. Dislocation can lead to more surgical interventions, additional outpatient consultations, and extended convalescence for the patient. Hence, much effort is paid to preventing this complication with different surgical strategies as previously described [9,10,11,12].
The mechanisms of graft adhesion in DSAEK are poorly understood. The graft is initially pushed to the host cornea by filling up the anterior chamber with air, and surface tension may facilitate the initial attachment. A “fibrillar interaction” between the host and donor stroma has been suggested [12]. Once the endothelial pump starts to function, the adhesion is further facilitated. Sometimes, if the decompensation of the host cornea is pronounced, the patient can experience improved vision as soon as the day after surgery, indicating that the EC pump probably begins working quickly. However, a study has shown graft adhesion in the presence of primary graft failure, indicating mechanisms other than the endothelial pump function being important for the adhesion of the graft [25].
The present study indicates that there is a difference in dislocation rate after DSAEK between the two different storage conditions used. There are mainly two well-documented storage systems for corneas worldwide. In the U.S., cold storage at 2–8 °C is most prevalent, a method introduced in 1974 [26]. Although the Food and Drug Administration has approved cold storage for a maximum of 14 days, most surgeons prefer a significantly shorter storage time, and storage up to 8 days has shown to preserved EC density as compared with shorter storage time [27]. The method using organ culture storage solution was introduced in Europe in 1978 and allows 4–5 weeks of storage [28,29,30].
Corneas stored in organ culture solution over 2 weeks are likely to be less immunogenic because of a decrease in antigen presenting cells, compared with cold storage [31]. This could theoretically lower the rejection rate of corneas stored in organ culture storage solution, but could obviously not explain the observations in the present study. One may speculate, however, that other unknown alterations to the media over time may influence the donor corneas and affect graft adhesion. Another speculation could be that the ECs function better in organ culture storage solution and start to work more rapidly than in corneas stored in cold storage solution, all of which may facilitate graft adhesion.
When it comes to EK, few studies are published comparing the clinical outcome in patients receiving donor corneas stored in these two storage systems. One study showed a higher dislocation rate using donor corneas stored in cold storage solution compared with organ culture storage solution in DMEK surgery [19]. The authors speculated that the slightly longer storage time for the corneas in cold storage solution (mean 9.4 days) than what is usual in the U.S. might explain this difference. This prolonged storage time was also the case in the present study, with an exact similar mean storage time of 9.4 days. However, this anticipation was not confirmed in our study, as we found no relationship between storage time and graft dislocation in patients who received grafts preserved in cold storage solution. Studies comparing these media, both prepared in the same local eye bank, would give us further answers to this question.
Another hypothesis regarding the difference in graft dislocation between the two storage conditions could be that donor corneas stored in cold storage solution in this study are shipped and not retrieved from our local eye bank. Other studies have shown that shipment corneas for transplantation have a negative outcome on corneal graft survival [32] and speculate that shaking, pressure change, and rapid acceleration and deceleration may play a role in this respect. However, other smaller studies comparing local and shipped corneas have not shown these differences [33, 34]. Even so, one may speculate that the combination of both prolonged storage time and transport itself could at least partly explain the difference seen in the dislocation rate between the two groups.
Two surgeons performed the surgeries in this study. Surgeon LD performed 310 surgeries from 2011 to 2016 and MS performed 84 surgeries from 2014 to 2016. Although MS was the least-experienced surgeon, she already knew the DSAEK technique when she started in 2014 and had no more dislocations than the more experienced surgeon. We found no association between different surgeons and rate of dislocation in the statistical analysis.
The mean dislocation rate in previous studies is reported to be around 14% (range 0–82%) [35]. The influence on dislocation rate using different storage media is, of course, more important when the overall dislocation rate is higher, as during a learning curve period. Still, our results suggest that even though the dislocation rate was low in both storage groups in the last few years, a significant difference was found in favour of organ culture storage solution.
In the present study, we found no relationship between dislocation rate and donor age- or gender, DTP, estimated graft thickness, or recipient age or gender. Only a few studies have investigated different preoperative conditions regarding donor and recipient cornea and rate of dislocation after DSAEK. One study reported no correlation between preoperative conditions (recipient diagnosis, corneal thickness, visual acuity, history of glaucoma) and dislocation rate [36]. In contrast to our findings, the same group experienced a significantly higher dislocation rate in older patients.
A limitation to the present study is its retrospective design. However, whether patients received donor corneas stored in cold or organ culture storage solution was random. Patients were scheduled for surgery regularly every week, independent of available grafts, as we ordered donor corneas from the U.S. in cases of shortages in donor corneas from our eye bank. This is also confirmed by the similar gender and age distribution in patients receiving donor corneas from the two storage media. Another limitation is that over the years, the surgeons have been more experienced and skilled, resulting in a lower dislocation rate. Since we have achieved an increasing number of donor corneas from our local eye bank over the years, this could have an impact on the results.
In conclusion, this study implies that, in the DSAEK surgery, donor corneas stored in organ culture storage solution may be preferable in avoiding graft dislocation. However, large prospective, randomized studies, where corneas stored under these two storage conditions originating from the same local eye bank, are required to give further answers. It would also be of interest to investigate the biomechanical and immunological properties of the different storage solutions to explain possible differences in graft adhesion.
Summary
What was known before
-
Dislocation rate in DSAEK varies from study to study.
What this study adds
-
We show that the dislocation rate in DSAEK using corneas stored in cold storage medium is higher than in corneas stored in organ culture medium.
References
Melles GR, Eggink FA, Lander F, Pels E, Rietveld FJ, Beekhuis WH, et al. A surgical technique for posterior lamellar keratoplasty. Cornea. 1998;17:618–26.
Terry MA, Chen ES, Shamie N, Hoar KL, Friend DJ. Endothelial cell loss after Descemet’s stripping endothelial keratoplasty in a large prospective series. Ophthalmology. 2008;115:488–96.e483.
Terry MA, Ousley PJ. Deep lamellar endothelial keratoplasty in the first United States patients: early clinical results. Cornea. 2001;20:239–43.
Price FW Jr., Price MO. Endothelial keratoplasty to restore clarity to a failed penetrating graft. Cornea. 2006;25:895–9.
Koenig SB, Covert DJ, Dupps WJ Jr., Meisler DM. Visual acuity, refractive error, and endothelial cell density six months after Descemet stripping and automated endothelial keratoplasty (DSAEK). Cornea. 2007;26:670–4.
Price MO, Gorovoy M, Benetz BA, Price FW Jr., Menegay HJ, Debanne SM, et al. Descemet’s stripping automated endothelial keratoplasty outcomes compared with penetrating keratoplasty from the Cornea Donor Study. Ophthalmology. 2010;117:438–44.
Suh LH, Yoo SH, Deobhakta A, Donaldson KE, Alfonso EC, Culbertson WW, et al. Complications of Descemet’s stripping with automated endothelial keratoplasty: survey of 118 eyes at One Institute. Ophthalmology. 2008;115:1517–24.
Saethre M, Drolsum L. The role of postoperative positioning after DSAEK in preventing graft dislocation. Acta Ophthalmol. 2014;92:77–81.
Price FW Jr., Price MO. Descemet’s stripping with endothelial keratoplasty in 200 eyes: early challenges and techniques to enhance donor adherence. J Cataract Refract Surg. 2006;32:411–8.
Vaddavalli PK, Diakonis VF, Canto AP, Kankariya VP, Pappuru RR, Ruggeri M, et al. Factors affecting DSAEK graft lenticle adhesion: an in vitro experimental study. Cornea. 2014;33:551–4.
Hovlykke M, Ivarsen A, Hjortdal J. Venting incisions in DSAEK: implications for astigmatism, aberrations, visual acuity, and graft detachment. Graefes Arch Clin Exp Ophthalmol. 2015;253:1419–24.
Terry MA, Shamie N, Chen ES, Hoar KL, Friend DJ. Endothelial keratoplasty a simplified technique to minimize graft dislocation, iatrogenic graft failure, and pupillary block. Ophthalmology. 2008;115:1179–86.
Hesham N, Schultze RL. Impact of donor characteristics on 2-year Descemet stripping automated endothelial keratoplasty outcomes in patients with Fuchs endothelial dystrophy. Cornea. 2015;34:6–10.
Price MO, Fairchild KM, Price DA, Price FW Jr. Descemet’s stripping endothelial keratoplasty five-year graft survival and endothelial cell loss. Ophthalmology. 2011;118:725–9.
Rijneveld WJ, Remeijer L, van Rij G, Beekhuis H, Pels E. Prospective clinical evaluation of McCarey-Kaufman and organ culture cornea preservation media: 14-year follow-up. Cornea. 2008;27:996–1000.
Frueh BE, Bohnke M. Prospective, randomized clinical evaluation of Optisol vs organ culture corneal storage media. Arch Ophthalmol. 2000;118:757–60.
Andersen J, Ehlers N. Corneal transplantation using 4-week banked donor material. Long-term results. Acta Ophthalmol. 1987;65:293–9.
Frueh BE, Bohnke M. Corneal grafting of donor tissue preserved for longer than 4 weeks in organ-culture medium. Cornea. 1995;14:463–6.
Laaser K, Bachmann BO, Horn FK, Schlotzer-Schrehardt U, Cursiefen C, Kruse FE. Donor tissue culture conditions and outcome after descemet membrane endothelial keratoplasty. Am J Ophthalmol. 2011;151:1007–1018.e1002.
Goshe JM, Terry MA, Li JY, Straiko MD, Davis-Boozer D. Graft dislocation and hypotony after Descemet’s stripping automated endothelial keratoplasty in patients with previous glaucoma surgery. Ophthalmology. 2012;119:1130–3.
Gupta PK, Bordelon A, Vroman DT, Afshari NA, Kim T. Early outcomes of descemet stripping automated endothelial keratoplasty in pseudophakic eyes with anterior chamber intraocular lenses. Am J Ophthalmol. 2011;151:24–28.e21.
Nahum Y, Leon P, Mimouni M, Busin M. Factors associated with graft detachment after primary descemet stripping automated endothelial keratoplasty. Cornea. 2017;36:265–8.
Busin M, Bhatt PR. Late detachment of donor graft after Descemet stripping automated endothelial keratoplasty. J Cataract Refract Surg. 2008;34:159–60.
Price MO, Price FW Jr. Endothelial cell loss after descemet stripping with endothelial keratoplasty influencing factors and 2-year trend. Ophthalmology. 2008;115:857–65.
Chaurasia S, Vaddavalli PK, Ramappa M, Garg P, Sangwan VS. Clinical profile of graft detachment and outcomes of rebubbling after Descemet stripping endothelial keratoplasty. Br J Ophthalmol. 2011;95:1509–12.
McCarey BE, Kaufman HE. Improved corneal storage. Investig Ophthalmol. 1974;13:165–73.
Terry MA, Shamie N, Straiko MD, Friend DJ, Davis-Boozer D. Endothelial keratoplasty: the relationship between donor tissue storage time and donor endothelial survival. Ophthalmology. 2011;118:36–40.
Andersen J, Ehlers N. Corneal transplantation using long-term cultured donor material. Acta Ophthalmol. 1986;64:93–6.
Pels E, Schuchard Y. Organ-culture preservation of human corneas. Doc Ophthalmol. 1983;56:147–53.
Sperling S. Early morphological changes in organ cultured human corneal endothelium. Acta Ophthalmol. 1978;56:785–92.
Al-Fakih A, Faltus V, Jirsova K. A decrease in the density of HLA-DR-positive cells occurs faster in corneas stored in organ culture than under hypothermic conditions. Ophthalmic Res. 2012;47:39–46.
Keane MC, Lowe MT, Coster DJ, Pollock GA, Williams KA. The influence of Australian eye banking practices on corneal graft survival. Med J Aust. 2013;199:275–9.
Varssano D, Russ V, Linhart Y, Lazar M. Air transportation of corneal tissue: experience with local compared to transatlantic donor corneas. Cornea. 2005;24:674–7.
Shimazaki J, Shinozaki N, Shimmura S, Holland EJ, Tsubota K. Efficacy and safety of international donor sharing: a single-center, case-controlled study on corneal transplantation. Transplantation. 2004;78:216–20.
Lee WB, Jacobs DS, Musch DC, Kaufman SC, Reinhart WJ, Shtein RM. Descemet’s stripping endothelial keratoplasty: safety and outcomes: a report by the American Academy of Ophthalmology. Ophthalmology. 2009;116:1818–30.
Hood CT, Woodward MA, Bullard ML, Shtein RM. Influence of preoperative donor tissue characteristics on graft dislocation rate after Descemet stripping automated endothelial keratoplasty. Cornea. 2013;32:1527–30.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sæthre, M., Krekling, E.D. & Drolsum, L. Lower risk of graft dislocation applying organ cultured corneas compared with cold short-term cultured corneas during DSAEK surgery. Eye 34, 711–716 (2020). https://doi.org/10.1038/s41433-019-0579-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-019-0579-8