Abstract
Background/objectives
To investigate the correlation between obstructive sleep apnea (OSA) severity and the structural and functional progression in patients with glaucoma.
Subjects/methods
This retrospective comparative cohort study included subjects from the polysomnography database in Chang Gung Memorial Hospital between June 1, 2009, and June 1, 2017, by identifying patients who had received diagnoses of primary open-angle glaucoma (POAG), normal-tension glaucoma (NTG), or glaucoma suspect. Patients with follow-up time of <3 years and/or <3 consecutive reliable optical coherence tomography (OCT) or visual field (VF) tests were excluded. Progression of overall peripapillary retinal nerve fiber layer (RNFL) thickness on OCT scans and VF mean deviation (MD) or VF index (VFI) were determined through linear regression trend analysis.
Results
Thirty-two patients were included. There was a trend to higher percentage of progression on RNFL thickness and VF in higher OSAS severity. After stratifying patients to no OSA/mild OSA (group 1) and moderate/severe OSA (group 2), group 2 exhibited a significantly higher percentage of RNFL thickness progression than did group 1 (64.7% vs 26.7%, P = 0.042). Multivariate Cox regression analysis showed that severe OSA had an 8.448-fold higher risk of RNFL thickness progression after age, sex, diabetes mellitus, hypertension, hyperlipidemia, and body mass index adjustment (95% confidence interval, 1.464–48.752, P = 0.017).
Conclusions
Severe OSA is significantly correlated with a higher risk of structural deterioration in patients with glaucoma.
Similar content being viewed by others
Introduction
Obstructive sleep apnea (OSA) is characterized by recurrent complete or partial upper airway occlusion during sleep that causes a decrease in airflow as well as oxygen desaturation [1, 2]. OSA has been associated with several ophthalmic conditions, such as floppy eyelid syndrome [3, 4], central serous choroidoretinopathy [5,6,7,8], retinal vein occlusions [9], papilledema [10, 11], nonarteritic anterior ischemic optic neuropathy [11,12,13,14,15,16,17], and is currently widely accepted as a risk factor for glaucoma [1, 2, 18]. The association between glaucoma and OSA has been reported in various studies, most of which were case–control or cross-sectional studies on the prevalence of these conditions or correlation of OSA severity with structural and functional changes related to glaucomatous damage [19,20,21,22,23,24,25,26,27,28,29,30]. Only two longitudinal studies have demonstrated the relationship between OSA and the risk of glaucoma, and both were database studies [31, 32]. To date, no longitudinal studies have focused on the correlation between OSA severity and the risk of glaucoma progression over time. Our study investigated the association between OSA severity and the structural and functional progression in patients with glaucoma.
Materials and methods
This retrospective comparative cohort study was conducted in a tertiary referral center, Chang Gung Memorial Hospital, Taoyuan, Taiwan. This study was approved by the institutional review board of Chang Gung Memorial Hospital in Taoyuan, Taiwan, and adhered to the tenets of the Declaration of Helsinki (IRB: 201601390B0).
The study cohort was selected from the polysomnography (PSG) database in Chang Gung Memorial Hospital between June 1, 2009, and June 1, 2017, by identifying patients who had received diagnoses of primary open-angle glaucoma (POAG), normal-tension glaucoma (NTG), or glaucoma suspect. The patients were first included by identifying a presumed International Classification of Diseases, Tenth Revision, coding indicating POAG, NTG, or glaucoma suspect (H40001–H40029, H40051–H40059, H4010X0–H4010X4, H401110–H401194, H401210–H401294, H4089, and H409). The medical records of the identified patients were then reviewed thoroughly to determine the diagnosis. Patients were excluded from the cohort if they exhibited closed anterior chamber angles, secondary causes of glaucoma, coexisting retinal disorders, or optic neuropathy in addition to glaucoma. The patients who did not exhibit glaucomatous disk appearance, retinal nerve fiber layer (RNFL) defects, visual field (VF) defects, and did not receive treatments for glaucoma were categorized as glaucoma suspect. The patients who received glaucoma treatments and exhibited either glaucomatous disk appearance, RNFL defects, or VF defects were classified as POAG or NTG. The patients were categorized as POAG if at least one measurement of intraocular pressure (IOP) exceeded 21 mmHg. If all measurements of IOP were within 21 mmHg, the patients were categorized as NTG.
Demographic data including the patients’ age at diagnosis, sex, body mass index (BMI), comorbidities, PSG results, OSA treatment and follow-up condition, and results of ophthalmic examinations, such as visual acuity, IOP, mean deviation (MD), and visual field index (VFI) in VF tests and thickness of circumferential peripapillary RNFL on OCT scans, were collected for analyses. All patients had undergone PSG at the sleep center of the hospital in a temperature-controlled and sound-attenuated room. During the examination, electroencephalography (EEG) was recorded to determine the period of sleep. The nasal and oral airflow and oxygen saturation of the patients were measured using thermistors and through pulse oximetry, respectively. Obstructive apnea was defined as a decrease in airflow by >80% compared with the normal value, lasting for at least 10 s. Obstructive hypopnea was defined as a decrease in airflow by >50% of the normal value with oxygen desaturation of >3%, lasting for at least 10 s [33, 34]. The apnea–hypopnea index (AHI) was defined as the total number of apneas or hypopneas per hour of the sleep period recorded through EEG. The classification of OSA severity according to the patients’ AHI scores was as follows: no OSA (AHI < 5), mild OSA (5 ≤ AHI < 15), moderate OSA (15 ≤ AHI < 30), and severe OSA (AHI ≥ 30) [33].
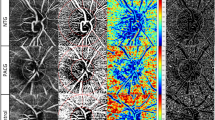
VFs were acquired using the Swedish Interactive Threshold Algorithm standard 30-2 or 24-2 strategies by using a Humphrey Field Analyzer II (Carl Zeiss Meditec, Dublin, CA, USA). The values of circumferential peripapillary RNFL thickness were evaluated using a Spectralis spectral-domain OCT device (Heidelberg Engineering, Heidelberg, Germany). We used MD or VFI of VF and circumferential peripapillary RNFL thickness on OCT scans to track the glaucoma status. The progression of the aforementioned parameters over time was determined using linear regression trend analysis, and a significant (P < 0.05) negative slope was defined as progression. To determine the time of progression, the series of each parameter from the first examination to each subsequent examination were evaluated. The time between the first examination and the earliest examination that showed a progression was defined as the time of progression detection. A progression of VF was defined as a progression of either MD or VFI. To ensure adequate numbers of data points for linear regression analysis, the patients who had a follow-up time of <3 years and those who had <3 consecutive reliable VF or OCT tests, were excluded from the study.
All statistical analyses were performed using SPSS version 17.0 (SPSS, Inc., Chicago, IL, USA). Qualitative data were expressed as numbers and percentages, whereas continuous variables were presented as mean and standard deviation. One-way analysis of variance (ANOVA) was used to compare differences in the numerical variables among groups. Categorical variables were analyzed using the Chi-squared test or Fisher exact test. A multivariate Cox proportional hazards regression model was used to determine the hazard ratios of progression in patients with comorbidities or OSA with different severity, whereas an event was defined as progression and survival as no progression. The curves of cumulative survival were also estimated using Cox regression analysis. P < 0.05 was considered statistically significant.
Results
Between June 1, 2009, and June 1, 2017, 14,152 patients who had undergone PSG had registered in the PSG database. Among these patients, 81 patients with POAG, NTG, and glaucoma suspect were identified. The patients were excluded if they had a follow-up time of <3 years or <3 consecutive reliable VF or OCT tests. Finally, 32 patients remained for analysis. The demographics of these patients are summarized in Table 1. The average age of the patients at diagnosis was 50.8 ± 13.2 years. Twenty-eight (87.5%) patients were men. The average BMI was 25.4 ± 2.3. According to the cutoff points for the Asian population [35], 24 (75.0%) of the patients were pre-obese (23.0 ≤ BMI < 27.5) and 5 (15.6%) were obese (BMI ≥ 27.5). Overall, 11 (34.4%), 14 (43.8%), and 7 (21.9%) patients were categorized as NTG, POAG, and glaucoma suspect, respectively. All the patients received adequate treatments for glaucoma and exhibited normal IOP during follow-up.
The demographic data of the patients grouped according to the AHI are summarized in Table 2. According to the AHI scores, 5 (15.6%), 10 (31.3%), 10 (31.3%), and 7 (21.9%) patients exhibited no, mild, moderate, and severe OSA, respectively. The four groups did not differ significantly in their age at diagnosis, sex, BMI, and prevalence of comorbidities, such as diabetes mellitus, hypertension, and hyperlipidemia.
Progressive thinning of the peripapillary RNFL detected on OCT scans was noted in 1 patient with no OSA (20.0%) and in 3 (30.0%), 5 (50.0%), and 6 (85.7%) patients with mild, moderate, and severe OSA, respectively. Relatively high severity of OSA was correlated with a high percentage of progression of RNFL thinning, although the correlation was not statistically significant (P = 0.096). We further divided the patients into two groups, no or mild OSA (AHI < 15, group 1) and moderate or severe OSA (AHI ≥ 15, group 2). The patients in group 2 had a significantly higher percentage of progression of RNFL thinning than did those in group 1 (64.7% vs 26.7%, P = 0.042) (Table 3).
Progression of MD or VFI in VF was observed in 1 (10.0%) patient with moderate OSA and 2 (28.6%) patients with severe OSA. Relatively high severity of OSA was correlated, although not significantly, with a high percentage of progression in VF (P = 0.219). The patients in group 2 exhibited a higher percentage of progression in VF compared with the patients in group 1 (17.6% vs 0.0%); however, the correlation was not significant (P = 0.229) (Table 4).
We also investigated whether treatment for OSA could ameliorate the progression of glaucoma. Of 27 patients with OSA, 7 patients received treatment with continuous positive airway pressure (CPAP), and 2 patients received surgery. Progression of RNFL thickness on OCT measurement was noted in 66.7% of patients with treatment, as compared with 44.4% of patients without treatment; however, there was no statistically significant difference (P = 0.420). Similarly, there was also no statistically significant difference in progression of MD and VFI on VF test between OSA patients with treatment and those without treatment (Supplementary Table 1).
A multivariate Cox proportional hazards regression model was used to determine the hazard ratios of the progression of RNFL thinning in patients with comorbidities or with OSA with different severity. After adjustment for age, sex, diabetes mellitus, hypertension, hyperlipidemia, and BMI, the results showed that severe OSA had 8.448-fold higher risk of progression of RNFL thinning than no or mild OSA did (95% CI 1.464–48.752, P = 0.017) (Table 5). By contrast, hypertension was correlated with a relatively low risk of progression of RNFL thinning (HR 0.231, 95% CI 0.063–0.852, P = 0.028) (Table 5). Other factors such as age, sex, diabetes mellitus, hyperlipidemia, BMI (preobesity or obesity), mild OSA, or moderate OSA did not significantly affect the progression of RNFL thinning on OCT scans (Table 5). The Cox regression adjusted survival curves are displayed in Supplementary Fig. 1.
Discussion
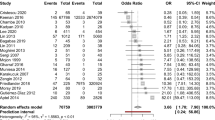
In this study, we investigated the relationship between OSA severity and structural and functional progression in glaucoma patients. The relationship between glaucoma and OSA was first reported in 1999 [19], which revealed a higher prevalence of POAG and NTG in patients with OSA than in the general population. Subsequently, several prevalence studies have also demonstrated an association between glaucoma and OSA [20,21,22,23,24, 26, 29]. A meta-analysis by Shi et al. [36] analyzed six case–control studies and nine cross-sectional studies and revealed a significantly higher prevalence of glaucoma in patients with OSA than in controls in the case–control (pooled OR = 1.96) and cross-sectional studies (pooled OR = 1.41) [36].
Tsang et al. [25] first evaluated changes in the optic disc and VF in patients with OSA. In their case–control study involving Chinese patients with moderate or severe OSA and matched non-OSA patients, the reported incidence of suspicious disc changes in the patients OSA was 4 times higher than that in the controls (26.39% vs 6.78%, P = 0.001), and the VF MD and PSD were both statistically subnormal in patients with OSA compared with controls (P < 0.01) [25]. Sergi et al. [26] further reported that the AHI was significantly correlated with VF MD in patients with NTG [26]. Lin et al. [27] first investigated the changes in RNFL thickness in patients with OSA using OCT. Their study included 247 participants consecutively admitted for PSG, and their RNFL thickness was measured through Stratus time-domain OCT. The RNFL was significantly thinner in the superior and temporal quadrants in the “moderate or severe OSA” group than in the “no or mild OSA” group. The prevalence of NTG was also significantly higher in patients with moderate or severe OSA than in those with no or mild OSA [27]. Several similar studies regarding RNFL thickness and OSA severity were later conducted, and a meta-analysis by Yu et al. [37] showed that both moderate and severe OSA were associated with a significant decrease in average, superior, inferior, and nasal RNFL thickness on OCT [37]. Other meta-analysis studies have also provided similar results [38,39,40,41].
More recently, Liguori et al. [30] demonstrated that patients with severe OSA exhibited a significantly more delayed latency and significantly lower amplitude of P100 waves on their visual evoked potential than the controls; however, electroretinography results did not differ significantly between the patients with OSA and controls [30]. Yu et al. [42] first evaluated OCT angiography changes in OSA patients. They noted that the peripapillary vessel density was significantly lower in patients with moderate and severe OSA than in those with no or mild OSA, but the density did not differ significantly between patients with moderate OSA and severe OSA. By contrast, the parafoveal vessel density was significantly lower in patients with severe OSA than in those with no or mild OSA, but the density did not differ between patients with moderate OSA and those with no or mild OSA [42].
However, most of the aforementioned studies were either case–control or cross-sectional studies. To date, only two large-scale longitudinal studies had been conducted on OSA and glaucoma, both of which were retrospective cohort studies using Taiwan National Health Insurance Research Database; both studies demonstrated the relationship between OSA and the risk of glaucoma [31, 32]. Lin et al. [31] reported that patients with OSA had 1.67 times higher risk of glaucoma than did patients without OSA within a 5-year period. Chen et al. [32] reported that patients with OSA who did not receive treatment had 2.15 times higher risk of glaucoma than those who received treatment, and treatment with surgery and other modalities, except CPAP, can significantly reduce the risk of glaucoma [32]. However, the database studies could only identify the time of receiving a glaucoma diagnosis but could not investigate the structural and functional progression of glaucoma over time. Only two brief reports, consisting of 3 patients, investigated OSA and glaucoma progression [43, 44]. Those reports suggested that treatment for OSA may mitigate progression on either RNFL thickness or VF. However, the patients in those reports underwent only few examinations, and linear regression trend analysis was not applied to determine whether progression occurred. In our study, we did not find treatment for OSA prevented the progression of glaucoma. The explanation for this finding was our relatively small case number. Besides, patients’ compliance to treatment with CPAP was unknown. Further studies with large case number as well as control of more comorbidities to see the effect of treatment are needed.
Because longitudinal studies on OSA and glaucoma progression over time are scant, we investigated the structural and functional progression in glaucoma patients with different levels of severity of OSA. Our data showed that patients with moderate or severe OSA exhibited a significantly higher prevalence of structural progression of RNFL thinning compared with patients with no OSA or mild OSA. Furthermore, we also demonstrated that severe OSA had 8.448-fold higher risk of structural progression of RNFL thinning after adjustment for age, sex, diabetes mellitus, hypertension, hyperlipidemia, and BMI. Although our study had few patients with functional progression of VF to provide any significant findings, our results also showed that relatively high severity of OSA was correlated with a relatively high prevalence of progression of VF. To the best of our knowledge, this is the first study to demonstrate a significant correlation between severity of OSA and structural deterioration in glaucoma over time. Based on the findings, we recommend to screen patients with glaucoma for severe OSA after they exhibit either rapid progression of RNFL thinning or deterioration of VF despite adequately controlled IOP.
Our study has several limitations. One major limitation is the small sample size, particularly with regard to groups with different severity of OSA. Although the study was conducted in the largest tertiary referral center in Taiwan, in which the PSG database included as many as 14,152 patients during the study period, only a few patients met the selection criteria of our study. That may be partially because we did not routinely refer patients with glaucoma to undergo PSG. Moreover, many patients with subjectively stable glaucoma may not prefer to attend follow-up in a busy medical center. Therefore, many patients were lost to follow-up after a short period; thus, they could not meet the criteria for trend analysis. We are conducting an additional study to investigate the neuroprotective effects of OSA treatment on patients with glaucoma.
In conclusion, our study demonstrated that patients with glaucoma and severe OSA exhibit a significantly higher risk of structural deterioration over time than those with no OSA. Clinicians should consider possible undiagnosed severe OSA when patients exhibit progression of glaucoma despite adequate treatments.
Summary
What was known before
-
OSA was associated with higher incidence of glaucoma, more thinning of peripapillary RNFL, and more severe VF defect.
-
OSA severity correlates with thinning of peripapillary RNFL on OCT, and decrease of peripapillary and parafoveal vessel density on OCTA.
-
OSA patients had higher risk of developing glaucoma in 5 years.
What this study adds
-
There was a trend to more glaucoma progression over time in higher OSA severity.
-
Severe OSA was significantly associated with a higher risk of glaucoma structural deterioration.
-
Underlying OSA should be considered when treated glaucoma still progressed.
References
Perez-Rico C, Gutierrez-Diaz E, Mencia-Gutierrez E, Diaz-de-Atauri MJ, Blanco R. Obstructive sleep apnea-hypopnea syndrome (OSAHS) and glaucomatous optic neuropathy. Graefes Arch Clin Exp Ophthalmol. 2014;252:1345–57.
Chaitanya A, Pai VH, Mohapatra AK, Ve RS. Glaucoma and its association with obstructive sleep apnea: a narrative review. Oman J Ophthalmol. 2016;9:125–34.
Ezra DG, Beaconsfield M, Collin R. Floppy eyelid syndrome: stretching the limits. Surv Ophthalmol. 2010;55:35–46.
Muniesa M, Sanchez-de-la-Torre M, Huerva V, Lumbierres M, Barbe F. Floppy eyelid syndrome as an indicator of the presence of glaucoma in patients with obstructive sleep apnea. J Glaucoma. 2014;23:e81–5.
Kloos P, Laube I, Thoelen A. Obstructive sleep apnea in patients with central serous chorioretinopathy. Graefes Arch Clin Exp Ophthalmol. 2008;246:1225–8.
Jain AK, Kaines A, Schwartz S. Bilateral central serous chorioretinopathy resolving rapidly with treatment for obstructive sleep apnea. Graefes Arch Clin Exp Ophthalmol. 2010;248:1037–9.
Brodie FL, Charlson ES, Aleman TS, et al. Obstructive sleep apnea and central serous chorioretinopathy. Retina. 2015;35:238–43.
Chatziralli I, Kabanarou SA, Parikakis E, Chatzirallis A, Xirou T, Mitropoulos P. Risk factors for central serous chorioretinopathy: multivariate approach in a case-control study. Curr Eye Res. 2017;42:1069–73.
Leroux les Jardins G, Glacet-Bernard A, Lasry S, Housset B, Coscas G, Soubrane G. Retinal vein occlusion and obstructive sleep apnea syndrome. J Fr Ophtalmol. 2009;32:420–4.
Purvin VA, Kawasaki A, Yee RD. Papilledema and obstructive sleep apnea syndrome. Arch Ophthalmol. 2000;118:1626–30.
Stein JD, Kim DS, Mundy KM, et al. The association between glaucomatous and other causes of optic neuropathy and sleep apnea. Am J Ophthalmol. 2011;152:989.
Mojon DS, Hedges TR 3rd, Ehrenberg B, et al. Association between sleep apnea syndrome and nonarteritic anterior ischemic optic neuropathy. Arch Ophthalmol. 2002;120:601–5.
Palombi K, Renard E, Levy P, et al. Non‐arteritic anterior ischaemic optic neuropathy is nearly systematically associated with obstructive sleep apnoea. Br J Ophthalmol. 2006;90:879–82.
Li J, McGwin G Jr., Vaphiades MS, Owsley C. Non-arteritic anterior ischaemic optic neuropathy and presumed sleep apnoea syndrome screened by the Sleep Apnea scale of the Sleep Disorders Questionnaire (SA-SDQ). Br J Ophthalmol. 2007;91:1524–7.
Arda H, Birer S, Aksu M, et al. Obstructive sleep apnoea prevalence in non-arteritic anterior ischaemic optic neuropathy. Br J Ophthalmol. 2013;97:206–9.
Bilgin G, Koban Y, Arnold AC. Nonarteritic anterior ischemic optic neuropathy and obstructive sleep apnea. J Neuroophthalmol. 2013;33:232–4.
Sun MH, Liao YJ, Lin CC, Chiang RP, Wei JC. Association between obstructive sleep apnea and optic neuropathy: a Taiwanese population-based cohort study. Eye. 2018;32:1353–8.
Mallick J, Devi L, Malik P, Mallick J. Update on normal tension glaucoma. J Ophthalmic Vis Res. 2016;11:204–8.
Mojon DS, Hess CW, Goldblum D, et al. High prevalence of glaucoma in patients with sleep apnea syndrome. Ophthalmology. 1999;106:1009–12.
Mojon DS, Hess CW, Goldblum D, Bohnke M, Korner F, Mathis J. Primary open-angle glaucoma is associated with sleep apnea syndrome. Ophthalmologica. 2000;214:115–8.
Onen SH, Mouriaux F, Berramdane L, Dascotte JC, Kulik JF, Rouland JF. High prevalence of sleep-disordered breathing in patients with primary open-angle glaucoma. Acta Ophthalmol Scand. 2000;78:638–41.
Marcus DM, Costarides AP, Gokhale P, et al. Sleep disorders: a risk factor for normal-tension glaucoma? J Glaucoma. 2001;10:177–83.
Mojon DS, Hess CW, Goldblum D, et al. Normal-tension glaucoma is associated with sleep apnea syndrome. Ophthalmologica. 2002;216:180–4.
Girkin CA, McGwin G, McNeal SF, Owsley C. Is there an association between pre‐existing sleep apnoea and the development of glaucoma? Br J Ophthalmol. 2006;90:679–81.
Tsang CS, Chong SL, Ho CK, Li MF. Moderate to severe obstructive sleep apnoea patients is associated with a higher incidence of visual field defect. Eye. 2006;20:38–42.
Sergi M, Salerno DE, Rizzi M, et al. Prevalence of normal tension glaucoma in obstructive sleep apnea syndrome patients. J Glaucoma. 2007;16:42–6.
Lin PW, Friedman M, Lin HC, Chang HW, Wilson M, Lin MC. Normal tension glaucoma in patients with obstructive sleep apnea/hypopnea syndrome. J Glaucoma. 2011;20:553–8.
Lin PW, Friedman M, Lin HC, Chang HW, Pulver TM, Chin CH. Decreased retinal nerve fiber layer thickness in patients with obstructive sleep apnea/hypopnea syndrome. Graefes Arch Clin Exp Ophthalmol. 2011;249:585–93.
Bilgin G. Normal-tension glaucoma and obstructive sleep apnea syndrome: a prospective study. BMC Ophthalmol. 2014;14:27.
Liguori C, Palmieri MG, Pierantozzi M, et al. Optic nerve dysfunction in obstructive sleep apnea: an electrophysiological study. Sleep. 2016;39:19–23.
Lin CC, Hu CC, Ho JD, Chiu HW, Lin HC. Obstructive sleep apnea and increased risk of glaucoma: a population-based matched-cohort study. Ophthalmology. 2013;120:1559–64.
Chen HY, Chang YC, Lin CC, Sung FC, Chen WC. Obstructive sleep apnea patients having surgery are less associated with glaucoma. J Ophthalmol. 2014;2014:838912.
Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22:667–89.
Kushida CA, Littner MR, Morgenthaler T, et al. Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep. 2005;28:499–521.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Shi Y, Liu P, Guan J, Lu Y, Su K. Association between glaucoma and obstructive sleep apnea syndrome: a meta-analysis and systematic review. PLoS ONE. 2015;10:e0115625.
Yu JG, Mei ZM, Ye T, et al. Changes in retinal nerve fiber layer thickness in obstructive sleep apnea/hypopnea syndrome: a meta-analysis. Ophthalmic Res. 2016;56:57–67.
Sun CL, Zhou LX, Dang Y, Huo YP, Shi L, Chang YJ. Decreased retinal nerve fiber layer thickness in patients with obstructive sleep apnea syndrome: a meta-analysis. Medicine. 2016;95:e4499.
Wang JS, Xie HT, Jia Y, Zhang MC. Retinal nerve fiber layer thickness changes in obstructive sleep apnea syndrome: a systematic review and Meta-analysis. Int J Ophthalmol. 2016;9:1651–6.
Zhao XJ, Yang CC, Zhang JC, Zheng H, Liu PP, Li Q. Obstructive sleep apnea and retinal nerve fiber layer thickness: a meta-analysis. J Glaucoma. 2016;25:e413–8.
Wang W, He M, Huang W. Changes of retinal nerve fiber layer thickness in obstructive sleep apnea syndrome: a systematic review and meta-analysis. Curr Eye Res. 2017;42:796–802.
Yu J, Xiao K, Huang J, Sun X, Jiang C. Reduced retinal vessel density in obstructive sleep apnea syndrome patients: an optical coherence tomography angiography study. Invest Ophthalmol Vis Sci. 2017;58:3506–12.
Kremmer S, Niederdraing N, Ayertey HD, Steuhl KP, Selbach JM. Obstructive sleep apnea syndrome, normal tension glaucoma, and nCPAP therapy—a short note. Sleep. 2003;26:161–2.
Sebastian RT, Johns S, Gibson RA. Treating obstructive sleep apnoea syndrome: does it improve visual field changes? Eye. 2006;20:118–20.
Acknowledgements
This study was supported by Chang Gung Memorial Hospital Research Grants [grant numbers CORPG1F0071 and CORPG3F0841]. The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41433_2019_430_MOESM1_ESM.docx
ST1 Percentage of progression in RNFL thinning on OCT scans, MD and VFI on VF tests among the patients with regular treatment and the patients without treatment for OSA
Rights and permissions
About this article
Cite this article
Fan, YY., Su, WW., Liu, CH. et al. Correlation between structural progression in glaucoma and obstructive sleep apnea. Eye 33, 1459–1465 (2019). https://doi.org/10.1038/s41433-019-0430-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-019-0430-2
This article is cited by
-
Increased risk of open-angle glaucoma in non-smoking women with obstructive pattern of spirometric tests
Scientific Reports (2022)
-
7,8-Dihydroxyflavone protects retinal ganglion cells against chronic intermittent hypoxia-induced oxidative stress damage via activation of the BDNF/TrkB signaling pathway
Sleep and Breathing (2022)
-
Progression patterns of normal-tension glaucoma groups classified by hierarchical cluster analysis
Eye (2021)
-
The Associations of Obstructive Sleep Apnea and Eye Disorders: Potential Insights into Pathogenesis and Treatment
Current Sleep Medicine Reports (2021)