Abstract
Background/objectives
Retinopathy of prematurity (ROP) is a potentially blinding disorder affecting premature infants. Our Eye Unit supports two neonatal intensive care units (NICUs), one provides neonatal surgical and medical facilities and the other is exclusively medical. Our objectives were to (1) to identify the annual rate of ROP treatments during the period 2009–2015 and (2) to estimate the incidence of ROP treatment in babies born very prematurely (<27 weeks).
Subjects/methods
Records for all infants treated for ROP by our unit during the period 2009–2015 were reviewed. We calculated numbers treated in each year. Records of babies born under 27 weeks of gestation and cared for in the non-surgical NICU were also reviewed. Their requirement for laser treatments for ROP was calculated by the week of gestation at birth.
Results
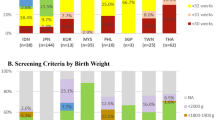
In the two NICUs combined, 95 infants were treated for ROP between 2009 and 2015. The numbers treated increased from 9/158 (5.7%) of babies screened in 2009 to 22/159 (13.8%) in 2015 (ptrend = 0.004). The rate of laser treatment for ROP increased as gestation at birth decreased: from 12/100 (12%) of babies born at 26 weeks to 17/29 (59%) of babies born at 23 weeks (ptrend = 0.001).
Conclusion
The number of laser treatments for ROP carried out by this unit has increased steadily between 2009 and 2015 and this may in part be due to the increased need for ROP treatment in extremely preterm babies, whose survival has increased in the same period. These data may aid planning for ROP services.
Similar content being viewed by others
Introduction
Retinopathy of prematurity (ROP) is a potentially blinding disorder affecting premature infants. Risk factors include a low gestational age and a low birth weight [1]. ROP is a major cause of preventable blindness in children worldwide [2]. The proportion of blind children affected by ROP has been reported as 37.4% in Former Soviet Economies and 23.9% in Latin American countries, in contrast with 10% in established market economies such as the UK and nil or extremely rare in sub-Saharan Africa [1]. The reasons for these differences are thought to include variation in levels of training in neonatal care and the ability to monitor oxygen saturations in babies having supplemental oxygen and the availability of ophthalmic support for screening and treatment.
Guidelines exist for screening to identify sight-threatening stages of ROP and to instigate timely treatment. Screening and treatment for ROP in the UK follows the guidelines set jointly by The Royal College of Ophthalmologists and the Royal College of Paediatrics and Child Health [3]. These use the nomenclature and descriptions (location in retinal zones 1–3; severity in stages 1–5 and plus or pre-plus to describe increases in retinal vessel calibre and tortuosity) of the International Committee for the Classification of ROP [4]. The current criteria for treatment are based on the Early Treatment of Retinopathy of Prematurity Study (ETROP) [5]. The features of ROP requiring treatment are collectively known as ‘Type 1 ROP’ which includes any stage ROP in zone 1 with plus; zone 1 stage 3 with or without plus; zone 2 stage 2 or 3 ROP with plus. Treatment may also be given for ‘Type 2 ROP’ if there is clinical concern, otherwise this can be kept under review until progression to type 1 ROP or regression takes place.
Screening in the UK is currently recommended for all babies born at <32 weeks of gestation or weighing <1501 g, starting at 4–5 weeks after birth or 30 weeks gestation (whichever is the later) and should continue until the retina is fully vascularised, or treatment is required. A recent national prospective surveillance study in the UK reported the incidence of ROP requiring treatment to be 4% in infants with birth weight <1500 g [6], which is greater than previous estimates of 1.5–2% [7, 8]. This study reported the majority of primary treatments for ROP were by diode laser photoablation of the avascular retina in 90.5% of babies and intravitreal injection of an anti-VEGF (currently not licensed) in 8% [6].
In our Eye Hospital unit, we treat babies with ROP cared for in either of two local level 3 neonatal intensive care units (NICUs) and some babies from other NICUs as requested. One of our NICUs offers regional surgical and medical facilities for neonates, while the other is exclusively medical and cares for a higher proportion of the extreme premature infants.
We had noticed an increase in the numbers of laser treatments being performed over the last few years and aimed to review this to inform future capacity planning. Additionally, as international studies have reported increased incidence of treatment-requiring ROP in very prematurely born babies as compared with babies born at higher gestations [9,10,11,12], we aimed to determine whether this was the case for our UK-born neonates.
The aims of this study were therefore twofold: firstly, describe yearly ROP treatments during the 7-year study period (2009 to 2015) and secondly to estimate the rates of ROP requiring treatment in infants born very preterm (<27 weeks), by weekly category of gestational age.
Patients and methods
First aim: laser treatments carried out per year by our unit
For the first aim, we retrospectively reviewed the clinical data of all the infants that were treated for ROP by the Vitreoretinal (VR) team at Bristol Eye Hospital between 1 January 2009 and 31 December 2015. Babies screened for ROP in Bristol include Bristol-booked infants and babies transferred to Bristol for tertiary care. Of note, the referral pathways did not change over the time period studied. The Western Network and Peninsula Network (lead centre Plymouth) combined in January 2013 to form the South West Neonatal Network, but this did not change the referral pathways for the tertiary units in the Network, therefore Bristol did not receive referrals from a wider area at any time during the study.
For all babies, we used the recommended criteria for screening (birth weight <1500 g and/or <32 weeks gestation) and the first examination was at 4–5 weeks after birth or 30 weeks gestation, whichever was the later. Examinations were carried out weekly. Treatment decisions were based on the 2008 RCOphth ROP Guidelines [3]. Initial treatment for all subjects consisted of transpupillary indirect ophthalmoscope diode laser therapy of laser burns to the entire avascular retina. Review was undertaken within 5–7 days, then weekly after treatment and the decision for further treatment (with either an intravitreal anti-VEGF agent, further laser or vitrectomy) was taken 2–3 weeks later if regression was not evident.
Infants that had been treated for ROP during the study period were retrospectively identified from a laser book held at the Eye Hospital and cross-referenced against lists held by the individual neonatal units identifying the individuals that were treated. Clinical data were taken from the neonatal electronic patient record database Badger Net.
Second aim: rates of ROP needing treatment by gestational age at birth
For the second aim, we reviewed the notes and database records of all babies under 27 weeks cared for in the exclusively medical NICU. Care of babies under 27 weeks in the Western neonatal network is centralised to NICUs in our area, the majority in the exclusively medical NICU. In order to estimate the survival rates and the need for laser treatment in extremely premature infants, we used as denominator all infants who were born or transferred within 48 h of birth to the exclusively medical NICU. For those who were transferred out of our area before their ROP screening was completed, we checked the national or regional neonatal database for details of any laser treatments carried out elsewhere.
Therefore, the groups of babies used to answer each question are not the same, although there is an overlap between them. Statistical significance was assessed with extended Mantel–Haenszel (MH) χ2 for linear trend.
Results
Study aim 1: laser treatments carried out each year between 2009 and 2015
During the 7-year study period, a total of 95 infants were treated for ROP, by the local vitreoretinal team (Table 1). Laser treatments were carried out under sedation and muscle relaxant, with intubation to support their ventilation. Each NICU had a dedicated room for the purpose and provided full nursing and neonatology support.
Over the time period studied (2009–2015), 8.2% of the infants who were examined required treatment for ROP. There was a year-on-year increase in the absolute number treated, with significantly more treated in 2015 compared to 2009 (Table 2). In the majority of cases (82 of 95, 86%), treatment consisted of one course of laser treatment alone. Additional treatment following the first course of laser was required in the remainder (13 of 95, 14%). This consisted of two courses of laser in 5 of 95 (5.3%), laser followed by an intravitreal injection of anti-vascular endothelial growth factor (VEGF) in 7 of 95 (7.4%) and laser followed by vitrectomy in 1 of 95 (1.1%), in this case, the infant was referred to a different centre for the vitrectomy due to aggressive ROP failing to regress following the initial laser treatment.
Of these 95 babies, approximately two-thirds were not later resident in Bristol, but were transferred to other units near their homes.
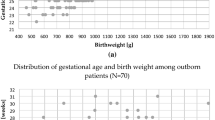
Study aim 2: incidence of ROP treatment by gestational age
Over the time period studied (2009–2015), 333 infants <27 weeks were cared for at the exclusively medical NICU. Of these 269 (81%) survived to complete ROP screening (Table 3). Figure 1 shows the number of babies <27 weeks gestation cared for at the exclusively medical NICU, and the number surviving to complete ROP screening increased from 2009 to 2015. Their survival improved from 69% in 2009 to 90% in 2015.
Survival to complete ROP screening improved with increasing gestation; 69% of 23 weeks gestation and 88% of 26 weeks gestation infants survived (Table 3). ROP treatment was required for 69 of 269 (26%) of extremely premature babies that survived to complete ROP screening. Of these, 56 (81%) were treated in Bristol (and are included in the first study aim) and 13 (19%) were treated at their base unit. The incidence of ROP treatment increased in proportion with the degree of prematurity at birth: extended MH χ2 for linear trend = 28.57; df = 1; p < 0.001. As shown in Fig. 2, 17/29 (59%) of those born at 23 weeks gestation required treatment compared to 12/100 (12%) of those born at 26-weeks gestation (Fig. 2).
Discussion
We aimed to answer two questions: firstly, was our unit carrying out increasing numbers of laser treatments for ROP over the last few years and secondly, in a cohort of extremely premature infants, did the rates of ROP needing treatment vary by week of gestational age at birth. We found that the absolute numbers of laser treatments carried out had increased, with no increase in the overall numbers of babies examined each year, suggesting that the babies in our local units were increasingly higher-risk (for ROP) as the study period progressed. We also observed that in a cohort of extremely premature (<27 weeks at birth) infants, not only were they increasingly more likely to survive as the study period progressed, but also the rate of ROP requiring treatment varied inversely with their gestational age at birth. Thus, while 12% of babies born at 26 weeks and survived needed laser for ROP, this was nearly fivefold higher for babies born at 23 weeks and survived (Table 3). These data suggest that the increase in ROP treatments we have carried out during the study period is in part be due to the increased survival of the more extreme premature infants. A recent population-based study showed the survival to discharge of extreme preterms in England between 2008 and 2014 was 36% for 23 weeks gestation, 59% for 24 weeks, 74% for 25 weeks and 83% for 26 weeks [13]. These survival rates are lower than those we observed in this study especially for the lower gestations (69% for 23 weeks gestation and 78% for 24 weeks). Thus, a small improvement in survival of the more extremely premature babies especially those at 23 and 24 weeks gestation will have a greater impact on the numbers requiring ROP treatment and therefore the ophthalmology service. Since 2008, in the UK as a whole, all care for <27 weeks gestation infants has been centralised to tertiary neonatal units such as the two in our city. This centralisation of services also increases the demands on the reduced numbers of Eye units carrying out ROP treatments and is a likely additional reason for the increase in ROP treatments we have observed.
Our study is not a population-based study and therefore cannot be used to estimate incidence of ROP treatment of those eligible for screening (<1500 g and/or <32 weeks gestation). The babies examined in the two NICUs include Bristol-booked infants and those born <27 weeks from the wider regional neonatal network, but excludes prematurely born local babies cared for in nearby level 2 centres. Previous studies have reported that the incidence of ROP treatment is increasing [14] and the recent national surveillance study found that more babies were treated for ROP in 2014 than were reported in a previous national study [15]. In our study, all babies were treated by diode laser as a primary treatment and 13.7% (13/95) required further treatment. This is similar to the national picture [6]. The use of other forms of treatment such as anti-VEGF intravitreal injections remains off licence in the UK, and this is an area where further research is required, particularly in identifying the safety profile of these medications systemically in premature infants. In our study, an anti-VEGF intravitreal injection was used as a second-line agent in 7 of the 13 cases where initial treatment had failed to result in resolution of the ROP. In the recent national audit, 8% of babies received anti-VEGF as firstline treatment [6]. Other reports have suggested that anti-VEGF intravitreal injections, may be of value in cases where there is poor visibility of the retina, which would make laser treatment difficult, or in cases where laser treatment has failed to result in regression of ROP [16].
A limitation of our study is that we have considered just one geographic area and the results may not be generalisable to other areas. The recording of ROP laser treatments in the laser book and/or the neonatal database may have been inaccurate and we could not cross-check data sources for babies treated outside our unit. We did not record the stage of ROP triggering the decision to treat, so the threshold for treatment may have varied over the study period and there is also well-recognised variability between ophthalmologists, for example regarding presence or absence of Plus disease [17]. However, the same team was involved in screening and treatment throughout the period, and the national guidelines did not change. A strength of this study is that we have defined a cohort of extreme preterms and obtained ROP-treatment outcome for all of them. This study, therefore, can estimate the incidence of ROP treatment in this defined population and has identified a greatly increased risk of needing ROP treatment for babies born at 23 or 24 weeks, compared to babies born when more mature. There are no reports of ROP treatment rate by gestation from other UK centres, but similar observations to ours have been made in other countries [9,10,11,12].
In conclusion, the recent increase in the incidence of ROP requiring treatment, which we have seen locally over our 7-year study period, appears to be at least in part due to the increased survival of premature infants. With on-going advances in neonatal intensive care facilities, particularly in developed countries, leading to the greater survival of extremely premature infants, it is likely that the incidence of ROP and ROP requiring treatment will continue to rise in future. With increasing centralisation of specialised services, the data we present may help in capacity planning and service design for Eye Units involved with care of babies with ROP. The data will also help neonatologists and ophthalmologists when counselling the parents of babies born extremely preterm, about the likelihood of ROP developing which requires treatment.
Summary
What was known before
ROP is a potentially blinding disorder affecting premature infants. Guidelines exist for screening to identify sight-threatening stages of ROP and to instigate timely treatment. Risk factors for ROP include low birth weight, low gestation at birth, high or variable oxygen.
What this study adds
ROP treatment has increased over the recent years. Improved survival in the extreme preterms over the recent years. Categorisation of incidence of ROP requiring treatment by gestational age.
References
Gilbert C, Muhit M. Twenty years of childhood blindness: what have we learnt? Community Eye Health. 2008;21:46–7.
Blencowe H, Lawn JE, Vazquez T, et al. Preterm-associated visual impairment and estimates of retinopathy of prematurity at regional and global levels for 2010. Pediatr Res. 2013;74(Suppl 1):35–49.
Guidelines for the screening and treatment of retinopathy of prematurity. 2008 guidelines. https://www.rcophth.ac.uk/wp-content/uploads/2014/12/2008-SCI-021-Guidelines-Retinopathy-of-Prematurity.pdf
International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Early Treatment for Retinopathy of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121:1684–94.
Adams GGW, Bunce C, Xing W, et al. Treatment trends for retinopathy of prematurity in the UK: active surveillance study of infants at risk. BMJ Open. 2017;7:e013366.
Painter SL, Wilkinson AR, Desai P, et al. Incidence and treatment of retinopathy of prematurity in England between 1990 and 2011: database study. Br J Ophthalmol. 2015;99:807–11.
Wong HS, Santhakumaran S, Statnikov Y, et al. Retinopathy of prematurity in English neonatal units: a national population-based analysis using NHS operational data. Arch Dis Child Fetal Neonatal Ed. 2014;99:F196–202.
Goyal A, Giridhar A, Gopalakrishnan M. Real-world scenario of retinopathy of prematurity in Kerala. Kerala J Ophthalmol. 2017;29:30–34.
Hwang JH, Lee EH, Ai-Rhan Kim E. Retinopathy of prematurity among very-low-birth-weight infants in Korea: incidence, treatment, and risk factors. J Korean Med Sci. 2015;30(Suppl 1):S88–94.
Isaza G, Arora S. Incidence and severity of retinopathy of prematurity in extremely premature infants. Can J Ophthalmol. 2012;47:296–300.
Liu Q, Yin ZQ, Ke N, Chen XK, Chen L, Fang J, et al. Incidence of Retinopathy of Prematurity in Southwestern China and Analysis of Risk Factors. Med Sci Monit. 2014;20:1442–51.
Santhakumaran S, Statnikov Y, Gray D, Battersby C, Ashby D, Modi N. Survival of very preterm infants admitted to neonatal care in England 2008-14: time trends and regional variation. Arch Dis Child Fetal Neonatal Ed. 2017;0:F1–8.
Austeng D, Kallen KB, Ewald UW, et al. Incidence of retinopathy of prematurity in infants born before 27 weeks’ gestation in Sweden. Arch Ophthalmol. 2009;127:1315–9.
Haines L, Fielder AR, Baker H, et al. UK population based study of severe retinopathy of prematurity: screening, treatment, and outcome. Arch Dis Child Fetal Neonatal Ed. 2005;90:F240–4.
Mintz-Hittner HA, Kennedy KA, Chuang AZ, et al. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med. 2011;364:603–15.
Fleck BW, Williams C, Juszczak E, Cocker K, Stenson BJ, Darlow BA, et al. An international comparison of retinopathy of prematurity grading performance within the Benefits of Oxygen Saturation Targeting II trials. Eye 2017; 1–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Financial support
CW is supported by an NIHR Senior Research Fellowship.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tavassoli, S., Wach, R., Haynes, R. et al. Estimate of incidence of ROP requiring treatment in extreme preterms and impact on service—7 year review in tertiary unit. Eye 33, 845–849 (2019). https://doi.org/10.1038/s41433-018-0330-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-018-0330-x
This article is cited by
-
Association of inflammatory and angiogenic biomarkers in maternal plasma with retinopathy of prematurity in preterm infants
Eye (2023)
-
Long use of continuous positive airway pressure protects against the development of treatment-requiring retinopathy of prematurity
Scientific Reports (2022)
-
Comment on: Estimate of incidence of ROP requiring treatment in extreme preterms and impact on service—7 year review in tertiary unit
Eye (2019)