Abstract
Purpose
To evaluate the clinical features and treatment outcomes of patients complaining of tearing after receiving chemotherapy.
Methods
The clinical records of patients who complained of tearing between August 2014 and February 2016, and underwent or were undergoing chemotherapy were retrospectively reviewed. Clinical measurements were as follows: LipiView® interferometer (lipid layer thickness and meibography), lacrimal drainage examinations (syringing), and outcomes at 6 months after treatment.
Results
This study included 34 eyes of 17 patients with a mean age of 62.4 ± 14.82 years. The mean follow-up period was 9.6 months. On syringing, 10 eyes (29.4%) showed total regurgitation, 19 eyes (55.9%) showed partial regurgitation, and 5 eyes (14.7%) showed no regurgitation. On LipiView®, mean lipid layer thickness was 34.5 nm (range, 20–89 nm). Mean meiboscore was 2.15 ± 0.86 in upper eyelid and 2.53 ± 0.79 in lower eyelid. Patients were treated with silicon tube intubation (STI) (10 eyes, 29.4%), dacryocystorhinostomy (DCR) (4 eyes, 17.6%), conjunctivodacryocystorhinostomy (CDCR) (8 eyes, 11.8%), DCR combined with CDCR (1 eyes, 8.8%), and conservative care (11 eyes, 32.4%). Mean time interval from onset of tearing to first clinic visit was 1.4 months in the conservative care group, 2.9 months in the STI and DCR groups, and 6.0 months in the CDCR group.
Conclusion
Because of the high incidence of accompanying meibomian gland loss in cases of lacrimal drainage system (LDS) obstruction, reflex tearing by mebibomian gland dysfunction should also be considered for proper management of tearing. Early recognition and management of LDS stenosis could result in patients undergoing surgery with a lower burden.
Similar content being viewed by others
Introduction
The use of chemotherapeutic agents has been associated with many ophthalmic complications that manifest as ocular surface, ocular adnexal, and lacrimal problems [1]. Tearing has been reported as an adverse effect of many chemotherapeutic drugs [2,3,4,5,6,7,8,9,10]. Epiphora resulting from stenosis or obstruction of the lacrimal drainage system (LDS) is a main cause of excessive tearing. Well-documented chemotherapeutic drugs that induce epiphora are S-1, docetaxel, paclitaxel, and 5-FU [4, 6, 7, 11]. Hyperlacrimation can also occur due to irritation caused by ocular surface lesions such as ocular irritation, conjunctivitis, and keratitis. Systemic chemotherapy can cause qualitative and quantitative changes in the tear film leading to damaged corneal and conjunctival epithelium [12].
The LDS, which is covered by a highly proliferative epithelium, is susceptible to the toxic effects of chemotherapeutic drugs. Such drugs may adversely affect the LDS through drug secretion in tears by producing local inflammation or through other less well-understood mechanisms [13]. Epiphora caused by stenosis of the LDS is an important consideration in patients undergoing chemotherapy who complain of tearing. A recent case report suggested that oral administration of anticancer TS-1® may cause meibomian gland dysfunction (MGD) [14]. MGD can be an important cause of reflex tearing. So, the consideration for reflex tearing is also becoming as an important cause of tearing in patients with chemotherapy.
Although there have been some studies on the pathophysiology of tearing in patients with chemotherapy, there have been few reports about the clinical features and treatment outcomes of these patients. The purpose of this study is to evaluate the clinical features and short-term treatment outcomes of patients complaining of tearing after receiving chemotherapy.
Patients and methods
Patients
The clinical records of patients who visited the Oculoplastic Outpatient Clinic, Department of Ophthalmology, Korea University Hospital between August 2014 and February 2016 and underwent or were undergoing chemotherapy in the Department of Hemato-oncology, Korea University Hospital and complained of tearing were retrospectively reviewed. The study was approved by the Institutional Review Board of Korea University Hospital. Patients with the following conditions were excluded from this study: 1. Young age (<18 years), 2. Short follow-up period (<6 months), 3. Ophthalmic disease (including LDS stenosis, severe dry eye or keratitis) before chemotherapy, and 4. Other systemic disease aside from cancer (including rheumatologic disease).
Clinical measurements
The following clinical measurements were used: (1) Slit-lamp biomicroscopy (tear break-up time (TBUT), fluorescein dye disappearance test (FDDT), punctum evaluation), (2) LipiView® interferometer (TearScience Inc., Morrisville, NC, USA) (lipid layer thickness and meibography), (3) lacrimal drainage examinations (probing, syringing and dacryoscintigraphy (DSG)), and (4) outcomes at 6 months after treatment (outcomes (subjective symptoms) were divided into three categories of no improvement, partial resolution, and complete resolution).
Ophthalmologic evaluation
Patients underwent slit-lamp biomicroscopic examinations to evaluate the puncta and measure TBUT. An FDDT was carried out to identify physiologic tear drainage function. FDDT was defined as grade 0 (no fluorescence in the conjunctival sac), grade 1 (thin fluorescein marginal tear strips only), grade 2 (between grades 1 and 3), and grade 3 (wide and bright fluorescein strip). Lacrimal irrigation (syringing) and probing were carried out through the lower punctum. The findings were divided into passage without regurgitation, passage with partial regurgitation, and no passage with complete regurgitation. Probing (Bowman Probe size 1) was performed. If the probe passed freely and then stopped suddenly against the lacrimal bone beneath the lacrimal sac wall, it was considered to indicate a patent canaliculus and lacrimal sac. If the probe encountered resistance and then stopped softly, it was considered to indicate soft tissue obstruction with canaliculi or at the common internal punctum. Patients also underwent DSG to confirm function of the LDS.
Meiboscore
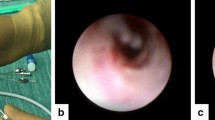
Meiboscores were measured using the non-contact LipiView® meibography system (Fig. 1). Partial or complete loss of the MG was scored using the following grades (meiboscore) for each eyelid: 0, no loss of MG; 1, area loss less than one-third of the total MG area; 2, area loss between one-third and two-thirds of the total MG area; 3, area loss was more than two-thirds of the total MG area [15].
Non-contact meibography LipiView® system image. The left column indicates meibography of right eye, which shows normal meibomian gland in upper and lower eyelids (meiboscore 0). The right column indicates interferometer of LipiView®. Specular reflections on tear film with interferometry color units (ICU) scale bar on right in anterior segment photograph (top). Graph showing changes in average, maximum, and minimum lipid layer thickness over 20 s (bottom)
Lipid layer thickness (LLT)
LLT was measured using LipiView® (Fig. 1), which applies white light interferometry, and the tear film is measured using interferometry color assessment via specular reflection. Interferometry color units (ICU) were used as the unit of measurement. ICU is an index of thickness and is estimated on the basis of observed mean interference colors. LipiView® determines the average, maximum, and minimum LLT over 20 s.
Statistical analysis
Data were analyzed using the Statistical Package for Social Sciences version 21.0 (SPSS Inc., Chicago, IL, USA). Kruskal-Wallis one-way analysis was used to compare means between multiple groups. Wilcoxon signed rank test was used to compare means between paired groups. P values ≤ 0.05 were considered statistically significant.
Results
This study included 34 eyes of 17 patients (9 males and 8 females) with a mean age of 62.4 ± 14.82 years (range, 33–80 years). The mean follow-up period was 9.6 months (range, 6-24 months). Mean chemotherapy duration was 13.8 months (range, 3–36 months). The locations of primary cancers were stomach (n = 10, 58.8%), lung (n = 4, 23.5%), breast (n = 2, 11.8%), and colon (n = 1, 5.9%). The types of chemotherapeutic agents included TS-1 (n = 10, 58.8%), Doxetaxel (n = 4, 23.5%), Paclitaxel (n = 2, 11.8%), and 5-FU (n = 1, 5.9%). The mean time to onset of tearing after chemotherapy was 9.4 months (range, 1–36 months). Nine patients (52.9%) had tearing within 3 months after chemotherapy, and 11 patients (64.7%) had tearing within 6 months after chemotherapy (Table 1).
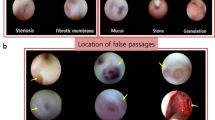
On slit lamp examination, mean TBUT was 5.4 s (range, 2–10 s). Mean FDDT was 1.91 ± 0.87 (range, 0–3) and 10 eyes (29.4%) had grade 1 normal findings. Puncta of 34 eyes were normal (24 eyes, 70.6%), stenotic (9 eyes, 26.5%), or obstructed (1 eye, 2.9%). On syringing, 10 eyes (29.4%) showed total regurgitation, 19 eyes (55.9%) showed partial regurgitation, and 5 eyes (14.7%) showed no regurgitation. On probing, 4 eyes (11.8%) had a soft stop and 30 eyes (88.2%) had a hard stop. However, in 8 of 30 eyes with a hard stop, resistance was felt when the probe passed through the canaliculus. On dacryoscintigraphy, 20 eyes (58.8%) showed pre-sac delay or obstruction, 8 eyes (23.5%) showed post-sac delay or obstruction, and 6 eyes (17.6%) were normal (Table 2).
On LipiView®, mean lipid layer thickness was 34.5 nm (range: 20–89 nm), lower than the normal value (>75 nm). In the upper eyelids, the meiboscore distribution was as follows: score 0, 0 eyes (0%); score 1, 10 eyes (29.4%); score 2, 9 eyes (26.5%); and score 3, 15 eyes (44.1%). In lower eyelids, meiboscore distribution was as follows: score 0, 0 eyes (0%); score 1, 6 eyes (17.6%); score 2, 4 eyes (11.8%); and score 3, 24 eyes (70.6%). Mean meiboscore in the upper and lower eyelids was 2.15 ± 0.86 and 2.53 ± 0.79 respectively, and this was a significant difference (P < 0.001) (Table 3).
Patients were treated with silicon tube intubation (STI) (10 eyes, 29.4%), dacryocystorhinostomy (DCR) (4 eyes, 17.6%), conjunctivodacryocystorhinostomy (CDCR) (8 eyes, 11.8%), DCR combined with CDCR (1 eyes, 8.8%), and conservative care (11 eyes, 32.4%). Two of 10 eyes failed STI and were then treated in a conservative manner. Four eyes of 2 patients who were classified as CDCR were initially treated with DCR, but symptoms did not improve, so CDCR was performed at 3 months and 15 months after DCR. In 21 eyes that underwent surgical procedures (STI, DCR, and CDCR), symptoms completely (11 eyes, 52.4%) or partially (10 eyes, 47.6%) resolved at 6 months after treatment. There were no surgical or anesthesia-related complications (Table 1).
Mean time from chemotherapy initiation to the onset of tearing was 11.5 months in the conservative care group, 13.3 months in the STI and DCR groups, and 3.3 months in the CDCR group. There was no significant differences among the three groups (P = 0.098). Mean time interval from onset of tearing to first clinic visit was 1.4 months in the conservative care group, 2.9 months in the STI and DCR groups, and 6 months in the CDCR group. There was no significant differences among the three groups (P = 0.096) (Table 4).
Discussion
Many studies have reported that chemotherapeutic drug caused stenosis of the LDS [2,3,4,5,6,7,8,9,10,11]. In this study, most patients had total (10 eyes, 29.4%) or partial (19 eyes, 55.9%) regurgitation on syringing. Most patients had a pre-sac delay (20 eyes, 58.8%) or post-sac delay (8 eyes, 23.5%) on dacryoscintigraphy. Mean FDDT was 1.91 ± 0.87, higher than the normal value. These findings are similar to previous reports, supporting that epiphora caused by stenosis of the LDS is the main cause of tearing in patients with chemotherapy.
All included patients had MG loss in upper and lower eyelids. Arita et al. [15] reported that changes in MGs increase with age. Age may have influenced the outcome of our study because 6 of 17 patients were older than 70 years old. However, patients under the age of 50 had definite MG loss, and regardless of age, most patients (70.6% in upper eyelid and 82.4% in lower eyelid) had severe MG loss more than score 2. Although this study is limited without a control group, the above results suggest that anticancer drugs are closely related to destruction of the MG. Eom et al. [16] found that loss of MG in the lower eyelid was greater than that in the upper eyelid in 10 patients on anticancer therapy because the tears containing anticancer drugs were in the lower fornix due to gravity, and the MG in lower eyelid was more affected by the cancer drug. Similarly, in this study, it was confirmed that the loss of MG in the lower eyelid was significantly larger than that in the upper eyelid. However, previous studies reported that the lower eyelid had a greater tendency for MG loss physiologically because it experiences less movement and ejects meibum in the opposite direction of gravity [17, 18]. Therefore, further study will be needed to understand precisely the effects of loss of MG due to anticancer drugs.
The results of several tests, including FDDT, probing, syringing and DSG, suggested epiphora is mainly caused by LDS obstruction. However, MG loss was observed in all patients with LDS obstruction, and 10 eyes (29.4%) had normal findings of grade 1 on FDDT, a relatively high proportion. LLT and TBUT, which indicate function of the MG, were definitely reduced. Five (14.7%) of 34 eyes were normal on lacrimal drainage examination. These results indicate that loss of the structure and function of the MG causes instability of the tear film and reflex tearing may occur. Both epiphora and hyperlacrimation should be considered to properly manage patients with tearing after chemotherapy.
Eleven (7 patients) of 34 eyes (17 patients) were treated with conservative therapy. Conservative treatment included administration of topical antibiotics and steroid to diminish inflammation and resultant scarring of the LDS and warm compression based on treatment of the MGD [19, 20]. In 5 of 11 eyes, there was no evidence of LDS stenosis (normal punctum, no regurgitation on lacrimal syringing, and hard stop on probing), so surgical treatment was not considered. The other 6 of these 11 eyes had LDS stenosis, but the patients refused surgical treatment (STI, DCR, and CDCR). In 4 of 5 eyes without LDS stenosis and 2 of 6 eyes with LDS stenosis, chemotherapy was finished before the first clinic visit. All 5 eyes without LDS stenosis and 2 of 6 eyes with LDS stenosis had partial symptom resolution 6 months after conservative treatment, but the other 4 eyes with LDS stenosis had no improvement of symptoms.
There have been a few reports of surgical treatment outcomes in patients with epiphora after chemotherapy. John et al. [21]. reported that in 19 patients who were treated with systemic 5-FU with complaints of tearing, 15 patients underwent surgery (STI: 5 patients, CDCR: 3 patients, STI and CDCR on each side: 1 patient, DCR: 1 patient, bilateral punctual 3-snip procedure: 4 patients, and STI failure: 1 patient) and all treated patients exhibited immediately improved symptoms. However, follow-up was not performed. In our study, 21 eyes of 13 patients who underwent surgical procedures (STI, DCR and CDCR) had their symptoms resolve completely (47.8%) or partially (52.2%) 6 months after treatment. Interestingly, all 9 eyes undergoing CDCR had complete resolution of tearing symptoms, whereas all 8 eyes undergoing STI showed partial resolution. Although there are many long-term complications, including tube extrusion, displacement and granulation [22], this study showed high success rates of CDCR for up to 6 months postoperative. In 9 eyes with STI treatment, there was no complete resolution due to stenotic change of the LDS. However, partial symptom resolution was achieved in all 9 eyes and complete LDS obstruction could be prevented. Therefore, STI is considered to have sufficient clinical significance.
Although there was no statistically significant difference, the mean time interval from onset of tearing to first clinic visit was longer in the CDCR group than in the conservative group and STI or DCR group. This indicates that CDCR can be avoided if ophthalmologic examination is promptly performed after the occurrence of tearing. CDCR requires the placement of a glass blown Jones tube to drain tears from the conjunctival cul de sac into the nose. CDCR can be associated with many complications, such as migration, extrusion, granulation and clogging [22]. Jones tubes also require a significant amount of care by patients and surgeons. Preservation of the natural lacrimal outflow system with a silicone tube is superior to the use of Jones tubes. After continued long-term administration of chemotherapeutic drugs, irreversible stenosis of the punctal and canalicular system may occur [3, 23]. Physicians should be aware of the importance of a timely ophthalmologic consultation for tearing in patients with chemotherapy.
Our study has some limitations. First, this was a retrospective non-comparative study. Therefore, comparison with the control group is needed to support the results of this study. Second, since only patients referred to the oculoplastic department of a tertiary medical institution were included in the study, there is a possibility for selection bias that may include patients with more severe ophthalmic conditions. Finally, because this study was conducted only on patients who had been treated in our department of hematology and oncology, only a small sample size was included. All members of the CDCR group were treated with TS-1, but we could not adequately analyze the clinical importance of this. Further research is needed to analyze the differences in clinical features according to the types and cumulative dose of anticancer therapies.
This is the first large single study to evaluate ophthalmic examination (including meibomian gland and LDS) and treatment of patients. The analysis of clinical features according to types and regimens of chemotherapeutic drugs with a larger sample size is a necessary follow-up clinical study.
Conclusion
Because of the high incidence of accompanying MG loss in cases of LDS obstruction, reflex tearing by MGD should also be considered for proper management of tearing. Failure to treat early LDS stenosis caused by chemotherapeutic drugs may lead to severe and irreversible punctal-canaliculus stenosis, which may necessitate CDCR. Early recognition and management of LDS stenosis could result in patients undergoing surgery with a lower burden to both patients and surgeons. Early visits to an ophthalmic clinic and early intervention is are important for better treatment outcomes, higher quality of life for patients and reduced socioeconomic costs.
Summary
What was known before
Chemotherapeutic drugs can be caused stenosis of the lacrimal drainage system (LDS).
Epiphora resulting from stenosis or obstruction of the LDS is a main cause of excessive tearing after chemotherapy.
What this study adds
Anticancer drugs are closely related to destruction of the MG.
Both epiphora and hyperlacrimation should be considered to properly manage patients with tearing after chemotherapy.
References
Imperia PS, Lazarus HM, Lass JH. Ocular complications of systemic cancer chemotherapy. Surv Ophthalmol. 1989;34:209–30.
Schmid KE, Kornek GV, Scheithauer W, Binder S. Update on ocular complications of systemic cancer chemotherapy. Surv Ophthalmol. 2006;51:19–40.
Haidak DJ, Hurwitz BS, Yeung KY. Tear-duct fibrosis (dacryostenosis) due to 5-fluorouracil. Ann Intern Med. 1978;88:657.
Esmaeli B, Golio D, Lubecki L, Ajani J. Canalicular and nasolacrimal duct blockage: an ocular side effect associated with the antineoplastic drug S-1. Am J Ophthalmol. 2005;140:325–7.
Eiseman AS, Flanagan JC, Brooks AB, Mitchell EP, Pemberton CH. Ocular surface, ocular adnexal, and lacrimal complications associated with the use of systemic 5-fluorouracil. Ophthal Plast Reconstr Surg. 2003;19:216–24.
Prasad S, Kamath GG, Phillips RP. Lacrimal canalicular stenosis associated with systemic 5-fluorouacil therapy. Acta Ophthalmol Scand. 2000;78:110–3.
Esmaeli B, Valero V, Ahmadi MA, Booser D. Canalicular stenosis secondary to docetaxel (taxotere): a newly recognized side effect. Ophthalmology. 2001;108:994–5.
Esmaeli B, Amin S, Valero V, Adinin R, Arbuckle R, Banay R, et al. Prospective study of incidence and severity of epiphora and canalicular stenosis in patients with metastatic breast cancer receiving docetaxel. J Clin Oncol. 2006;24:3619–22.
Esmaeli B, Burnstine MA, Ahmadi MA, Prieto VG. Docetaxel-induced histologic changes in the lacrimal sac and the nasal mucosa. Ophthal Plast Reconstr Surg. 2003;19:305–8.
Esmaeli B, Hidaji L, Adinin RB, Faustina M, Coats C, Arbuckle R, et al. Blockage of the lacrimal drainage apparatus as a side effect of docetaxel therapy. Cancer. 2003;98:504–7.
McCartney E, Valluri S, Rushing D, Burgett R. Upper and lower system nasolacrimal duct stenosis secondary to paclitaxel. Ophthal Plast Reconstr Surg. 2007;23:170–1.
Omoti AE, Omoti CE. Ocular toxicity of systemic anticancer chemotherapy. Pharm Pract (Granada). 2006;4:55–59.
Mansur C, Pfeiffer ML, Esmaeli B. Evaluation and management of chemotherapy-induced epiphora, punctal and canalicular stenosis, and nasolacrimal duct obstruction. Ophthal Plast Reconstr Surg. 2017;33:9–12.
Mizoguchi S, Okada Y, Kokado M, Saika S. Abnormalities in the meibomian glands in patients with oral administration of anticancer combination drug-capsule TS-1((R)): a case report. BMC Cancer. 2015;15:796.
Arita R, Itoh K, Inoue K, Amano S. Noncontact infrared meibography to document age-related changes of the meibomian glands in a normal population. Ophthalmology. 2008;115:911–5.
Eom Y, Baek S, Kim HM, Song JS. Meibomian gland dysfunction in patients with chemotherapy-induced lacrimal drainage obstruction. Cornea. 2017;36:572–7.
Srinivasan S, Menzies K, Sorbara L, Jones L. Infrared imaging of meibomian gland structure using a novel keratograph. Optom Vis Sci. 2012;89:788–94.
Eom Y, Choi KE, Kang SY, Lee HK, Kim HM, Song JS. Comparison of meibomian gland loss and expressed meibum grade between the upper and lower eyelids in patients with obstructive meibomian gland dysfunction. Cornea. 2014;33:448–52.
Brink HM, Beex LV. Punctal and canalicular stenosis associated with systemic fluorouracil therapy. Report of five cases and review of the literature. Doc Ophthalmol. 1995;90:1–6.
Olson MC, Korb DR, Greiner JV. Increase in tear film lipid layer thickness following treatment with warm compresses in patients with meibomian gland dysfunction. Eye Contact Lens. 2003;29:96–99.
Fezza JP, Wesley RE, Klippenstein KA. The treatment of punctal and canalicular stenosis in patients on systemic 5-FU. Ophthalmic Surg Lasers. 1999;30:105–8.
Sekhar GC, Dortzbach RK, Gonnering RS, Lemke BN. Problems associated with conjunctivodacryocystorhinostomy. Am J Ophthalmol. 1991;112:502–6.
Caravella LP Jr, Burns JA, Zangmeister M. Punctal-canalicular stenosis related to systemic fluorouracil therapy. Arch Ophthalmol. 1981;99:284–6.
Author contributions
Conception and study design (JP, JK, SB), Study orchestration (JP, JK, SB), Data collection and management (JP, JK, SB), Data analysis (JP, JK, SB), Data interpretation (JP, JK, S), Preparation, review, and approval of the manuscript (JP, JK, SB). D The Institutional Review Board of the Korea University Guro Hospital approved this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The Institutional Review Board of the Korea University Guro Hospital approve.
Rights and permissions
About this article
Cite this article
Park, J., Kim, J. & Baek, S. Clinical features and treatment outcomes of patients with tearing after chemotherapy. Eye 33, 746–753 (2019). https://doi.org/10.1038/s41433-018-0305-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-018-0305-y
This article is cited by
-
Antineoplastics
Reactions Weekly (2019)