Abstract
Purpose
To describe the principle characteristics of combined hamartoma of the retina and retinal pigment epithelium (‘combined harmatoma’) on MultiColorTM imaging and evaluate its role as a diagnostic and management tool.
Methods
Retrospective, observational case series comprising three patients with unilateral, juxtapapillary combined harmatoma. Complete ophthalmic examination was performed. MultiColorTM, including green reflectance (GR) and near infra-red reflectance (NIRR), optical coherence tomography (OCT) and autofluorescence (AF) imaging were obtained (Heidelberg Spectralis).
Results
On MultiColorTM, ‘red shifting’, indicated partial pigmentation. GR clearly defined epiretinal gliosis, retinal dragging and striations. On NIRR, all lesions were hypo-reflectant with hyper-reflectance at their edges. OCT showed full-thickness retinal thickening and disorganisation, intra-retinal fluid in two cases, sectoral RPE atrophy with photoreceptor loss in one case, RPE thickening and foveal pigment migration in one case; epiretinal membrane associated with ‘mini peaks’ of the inner retina in all cases and vitreous traction causing retinoschisis in one case. All lesions were hypo-autofluorescent.
Conclusions
MultiColorTM enables combined harmatomas to be further characterised and may represent a valuable diagnostic and management tool: MultiColorTM and NIR define tumour boundaries and macular involvement, which may be useful for assessing visual impact; GR highlights inner retinal distortion, which may aid surgical management decisions.
Similar content being viewed by others
Introduction
Combined hamartoma of the retina and retinal pigment epithelium (‘combined hamartoma’) is a benign ocular tumour. Accurate diagnosis is critical, as enucleations for presumed melanomas have been reported [1, 2]. MultiColorTM imaging is a novel technique that scans the retina at three depths simultaneously, producing a high-resolution image detailing different retinal layers [3]. In this case series, our aim was to describe the characteristics of combined hamartomas on MultiColorTM imaging and to evaluate its role in their diagnosis and management.
Materials and methods
This retrospective, observational case series, conducted in compliance with the World Medical Association Declaration of Helsinki [4], comprised three patients with combined hamartoma in the left eye, attending Southampton University Hospital, UK. A complete ophthalmic examination, including best corrected visual acuity (BCVA), was performed. MultiColorTM, including green reflectance (GR) and near infra-red reflectance (NIRR), OCT and autofluorescence (AF) imaging, was obtained with the Spectralis combined scanning laser ophthalmoscopy and enhanced depth imaging OCT (Heidelberg Engineering, Germany). In one case Spectralis OCT was unavailable, so Topcon OCT (Topcon Europe) was used.
Case Reports
Case 1: a 55-year-old female, referred for an incidental finding of a left fundus lesion. She had bilateral sensorineural hearing loss, but was otherwise well. BCVA was OU 0.12 and OS 1.16 LogMAR. Examination of the right eye was unremarkable. Acoustic neuroma was excluded.
Case 2: a 44-year-old, otherwise well male, initially referred for a possible central retinal vein occlusion affecting the left eye. BCVA was OU 0.12 and OS 0.42 LogMAR. Examination of the right eye revealed a small RPE detachment, consistent with previous central serous chorioretinopathy.
Case 3: a 35-year-old male presenting with distorted vision in the left eye, which was reported to be amblyopic. He was otherwise well. BCVA was OU −0.08 and OS 0.86 LogMAR. Horizontal nystagmus was present. Examination of the right eye was unremarkable.
Results
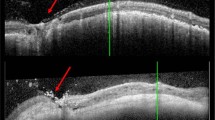
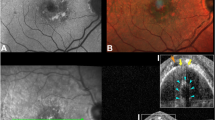
All patients had an elevated, partially pigmented, and juxtapapillary tumour. Mean presenting BCVA was 0.81 LogMAR. OCT (Figs. 1e, 2f, 3e) showed thickening and disorganisation of all retinal layers, with intra-retinal fluid in two cases. In Case 1, the retinal pigment epithelium (RPE) showed sectoral atrophy with corresponding photoreceptor loss (Fig. 1e), whilst in Case 2 (Fig. 2f), the RPE was thickened, at the lesion and the fovea, where pigment migration was noted. An epiretinal membrane (ERM) was evident in all cases, associated with ‘mini peaks’ of the inner retina, and in Case 3 (Fig. 3e) with retinoschisis resulting from vitreous traction. On AF (Figs. 1d, 2d–e, 3c), the lesions were hypo-autofluorescent. On MultiColorTM (Figs. 1a, 2a, 3a), they displayed ‘red shifting’, confirming their partial pigmentation. GR (Figs. 1c, 2b, 3b) highlighted the extent of epiretinal gliosis, with clear delineation of retinal striations and dragging. On NIRR (Figs. 1b, 2c, 3d), the tumours were hypo-reflectant with hyper-reflectance at their edges, enabling their boundaries to be clearly defined.
Case 1. a–e (clockwise from top left): a MultiColorTM shows red-shifting at the temporal optic disc and infero-temporal border of the lesion (←), indicating pigmentation. b On NIRR, a corresponding area of hypo-reflectance (←), confirms the pigmentation and better defines the edges of the lesion. c On GR, the extent of epiretinal gliosis and retinal dragging can be seen; superficial striae are clearly delineated (↑), departing from the optic disc and encompassing the fovea. d On AF, the lesion displays hypo-autofluorescence, obscuring the normal blood vessel hypo-autofluorescence. e OCT over the lesion reveals disorganisation and thickening of all retinal layers, disrupted by intra-retinal cysts (↑). There is sectoral RPE atrophy with loss of photoreceptors (↑↑) and telangectatic vessels (*) at a deeply excavated optic disc. There is an obvious ERM (↓). The posterior hyaloid is attached at the optic disc (↓) and vitreous traction is present. f OCT over the macula demonstrates a posterior hyaloid detachment (↑) with an underlying ERM (↓)
Case 2. (a–f) (clockwise from top left): a MultiColorTM shows areas of ‘red-shifting’, indicating partial pigmentation of the lesion. b GR better defines the overlying epiretinal gliosis, dragging of the retina and retinal striations. c On NIRR, the edges of the lesion display hyper-reflectance (←), helping to define its boundaries more clearly. d,e On AF the lesion corresponds to an area of hypo-autofluorescence that becomes patchier distant from the optic disc. f OCT over the lesion shows a thickened and disorganised retina. An overlying ERM (↓) is causing 'mini-peaks' of the inner retina (*) and distorting its profile. g OCT over the macula shows a thickened and disorganised ellipsoid zone (↓). The RPE is also thickened, at the level of the lesion and at the fovea, where there is minimal pigment migration (←) that does not reach the neuroretina. Note that macular anatomy is mostly preserved, which is also associated with relatively better visual acuity in this patient
Case 3. (a–e) (clockwise from top left): a On MultiColorTM the lesion displays 'red shifting', indicating partial pigmentation. b On NIRR the lesion is defined more clearly as an area of hypo-reflectance with hyper-reflectance (←) at its edges. c On AF, the lesion corresponds to an ill-defined area of hyporeflectance; its boundaries are obscured by epiretinal gliosis. d GR most clearly shows the epiretinal gliosis overlying the lesion and retinal striae (←) extending radially. e OCT over the lesion shows prominent disorganisation of retinal architecture, with thickening of inner retinal layers (*) and intra-retinal fluid (**). There is an obvious ERM (↓) associated with “mini-peaks” of the inner retina (←). Vitreous traction overlying the lesion is causing tractional retinoschisis. f OCT over the macula shows that there is no foveal pit but there is a pseudohole (↓) and intra-retinal cysts (*). As this is a retrospective case series a Spectralis OCT was not available, thus a TopCon OCT is provided
Discussion
Combined hamartoma was described by Gass as a hamartomatous malformation involving the RPE, retina, retinal vasculature and overlying vitreous [5]. OCT has enabled the structure of these tumours to be explored in great detail [6,7,8] but accurately determining their location on the retina can be difficult, given that it focuses in so closely on a particular section.
As well as altering the inner retinal surface, combined hamartomas may also affect the deeper retinal layers and the RPE. Establishing the size and extent of a tumour is particularly important when it encroaches on the macula, as the degree of macular involvement is highly related to its visual impact [9]. In our patients, the whole tumour and surrounding retina could be included in the MultiColorTM image, enabling its location to be precisely mapped out. Using three different wavelengths, details within the lesion itself could also be captured simultaneously. Clinically, the boundaries of combined hamartomas can be hard to distinguish [6]. In the present series, however, NIRR proved to be very helpful in better delineating both edges of the tumour and the extent of macular involvement. If surgical intervention is being considered, such as an ERM peel, taking these factors into account is essential. Even if conservative measures are preferred, this added information can be used to enable more accurate prognostication. MultiColorTM imaging used in combination with OCT may thus be invaluable for optimising clinical management. ERMs are a prominent feature of combined hamartomas [7], associated with ‘mini-peaks’ of the inner retina and ‘maxi-peaks’ involving the full retinal thickness [8]. Surgical removal remains controversial; although visual improvement has been reported in younger patients [10, 11], in two older patients it was not reported [12]. A possible reason is that irreversible visual loss had occurred in the presumably longer-standing tumours, indicating that the degree of retinal distortion already present may be an important determinant of visual outcome. In this series of patients, GR was useful for characterising epiretinal gliosis, by illustrating dragging of the retina and defining the extent of inner retinal distortion. GR could therefore be considered a useful adjunct to OCT for establishing the morphological features of the vitreoretinal interface and the inner retina and thus in influencing surgical management decisions. From this perspective, none of the cases in this series were considered as suitable for surgical management.
Although combined hamartomas are benign, accurate diagnosis remains critical, because unnecessary enucleations for presumed melanomas have been reported [1, 2]. While MultiColorTM imaging alone cannot differentiate between the two conditions and thus cannot replace traditional imaging techniques, it may be considered a valuable modality in better illustrating important characteristics regarded as suspicious for malignancy, such as lipofuscin clumps and subretinal fluid (Fig. 4). A detailed description of the differential diagnosis of combined hamartomas however, is beyond the purpose of the present case series.
In conclusion, MultiColorTM imaging contributes valuable information regarding the anatomical characteristics of combined hamartomas and may be useful in establishing their diagnosis, aiding management and informing prognosis.
Summary
What was known before
-
Combined hamartoma is a benign ocular lesion but visual prognosis can be poor and accurate diagnosis is critical to distinguish it from malignant tumours.
-
MultiColorTM imaging is a novel technique that can be used to highlight different layers within the retina simultaneously.
What this study adds
-
MultiColorTM and NIRR are helpful in defining tumour boundaries and the extent of macular involvement, which may be useful for assessing visual impact.
-
GR highlights epiretinal gliosis and the degree of inner retinal distortion, which may aid surgical management decisions.
-
MultiColorTM imaging contributes further information regarding the anatomical characteristics of combined hamartomas and may thus be valuable in establishing their diagnosis, aiding management decisions and informing prognosis.
References
Vogel MH, Zimmerman LE, Gass JD. Proliferation of the juxtapapillary retinal pigment epithelium simulating malignant melanoma. Doc Ophthalmol. 1969;26:461–81.
Theobald GD, Floyd G, Kirk HQ. Hyperplasia of the retinal pigment epithelium simulating a neoplasm: report of two cases. Am J Ophthalmol. 1958;45:235–40.
Querques G, Srour M, Massamba N, Puche N, Souuied EH. Reticular pseudodrusen. Ophthalmology. 2013;120:872–2.
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4.
Gass JD. An unusual hamartoma of the pigment epithelium and retina simulating choroidal melanoma and retinoblastoma. Trans Am Ophthalmol Soc. 1973;71:171–83.
Ting TD, McCuen BW 2nd, Fekrat S. Combined hamartoma of the retina and retinal pigment epithelium: optical coherence tomography. Retina. 2002;22:98–101.
Shields CL, Mashayekhi A, Dai VV, Materin MA, Shields JA. Optical coherence tomographic findings of combined hamartoma of the retina and retinal pigment epithelium in 11 patients. Arch Ophthalmol. 2005;123:1746–50.
Arepalli S, Pellegrini M, Ferenczy SR, Shields CL. Combined hamartoma of the retina and retinal pigment epithelium: findings on enhanced depth imaging optical coherence tomography in eight eyes. Retina. 2014;34:2202–7.
Shields CL, Thangappan A, Hartzell K, Valente P, Pirondini C, Shields JA. Combined hamartoma of the retina and retinal pigment epithelium in 77 consecutive patients visual outcome based on macular versus extramacular tumor location. Ophthalmology. 2008;115:2246–52.
Stallman JB. Visual improvement after pars plana vitrectomy and membrane peeling for vitreoretinal traction associated with combined hamartoma of the retina and retinal pigment epithelium. Retina. 2002;22:101–4.
Mason JO 3rd, Kleiner R. Combined hamartoma of the retina and retinal pigment epithelium associated with epiretinal membrane and macular hole. Retina. 1997;17:160–2.
McDonald HR, Abrams GW, Burke JM, Neuwirth J. Clinicopathological results of vitreous surgery for epiretinal membranes in patients with combined retinal and retinal pigment epithelial hamartomas. Am J Ophthalmol. 1985;100:806–13.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kaprinis, K., Bobat, H. & De Salvo, G. MultiColorTM imaging in combined hamartoma of the retina and retinal pigment epithelium. Eye 32, 1478–1482 (2018). https://doi.org/10.1038/s41433-018-0123-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-018-0123-2