Abstract
Purpose
This study was designed to assess the efficacy, reliability and repeatability of SPARCS (Spaeth Richman Contrast Sensitivity Test) as compared to the conventional Pelli Robson Chart Test for the assessment of contrast sensitivity in patients with glaucoma.
Materials and Methods
We evaluated 135 eyes of 135 patients who were age and sex matched into three groups (controls, disc suspects and glaucoma) of 45 patients each. The glaucoma subgroup was further divided into subgroups of mild, moderate and severe based on the visual field damage.
Results
There was a strong positive correlation between Pelli Robson scores and SPARCS scores (S = 0.807, P < 0.001). Intraclass correlation coefficient (ICC) for Pelli Robson Test was 0.952 and 0.988 for SPARCS. The coefficient of repeatability (COR) for mean SPARCS was 5.65%, while COR of Pelli Robson Test was 12.44%. SPARCS was found to have better repeatability than Pelli Robson Test based on COR values. Pelli Robson score had a sensitivity of 80% and a specificity of 65.6% for detecting glaucoma patients as compared to 84.4% and 70%, respectively, for SPARCS scores.
Conclusion
SPARCS is a better alternative to conventional Pelli Robson Chart Test for assessment of contrast sensitivity in patients with glaucoma. Being independent of the effects of literacy and educational status, it offers a universal way to measure contrast sensitivity. It can also be reliably used in patients with varying severity of glaucoma.
Similar content being viewed by others
Introduction
Glaucoma is the leading cause of irreversible blindness worldwide and a major public health concern [1]. Currently, perimetric (visual field) losses are used to define and document progression in glaucoma; however, alone they are not enough to detect the earliest pathological changes. It has been shown that around 30% of the optic nerve axons are lost before defects become apparent in the visual field [2, 3]. The inadequacy of visual fields to detect early glaucomatous damage has led to attempts to measure this damage with contrast sensitivity.
Earlier studies have employed assessment of central contrast sensitivity as an aid to diagnose glaucoma before the emergence of visual field defects using the conventional Pelli Robson chart, gratings, oscilloscopes and computer-based contrast sensitivity tests like McArden colour contrast sensitivity test that involved only foveal viewing of the display/chart [4]. These studies had a sensitivity and specificity around 50% and thus these methods of assessment of contrast sensitivity could not be used as a screening test for diagnosing or detecting early glaucoma. The tests were inadequately evaluated, required special equipment, were costly and had low test–retest reliability [5].
Since classical glaucomatous visual field loss is usually detected first in the periphery, often as an arcuate scotoma occurring in the superior or inferior hemifield within 20° of the fovea, attempts were subsequently made to correlate the peripheral visual field loss with contrast sensitivity measurements [6]. Richman et al. [7] found that contrast sensitivity loss correlated more closely and strongly to glaucomatous damage than binocular visual field loss in patients with glaucoma. Contrast sensitivity testing thus may be more sensitive to subtle changes in visual function when compared to other commonly used tests such as visual field and visual acuity evaluating retinal function and thus may also be able to detect glaucomatous changes even prior to visual field and structural changes [8]. This belief led to the development of Spaeth Richman Contrast Sensitivity Test (SPARCS) for detecting contrast sensitivity for patients with glaucoma. SPARCS measures contrast sensitivity in both central and peripheral field which makes it a better tool to assess glaucomatous damage as compared to the tests available earlier which were measuring only central contrast sensitivity[4]. SPARCS has been used to identify patients with glaucoma with high test–retest reliability and correlates well with the most commonly used optotype-based Pelli Robson contrast sensitivity chart [6]. In addition to its role in glaucoma assessment, SPARCS has also been shown to be a reliable method to assess contrast sensitivity in cases of refractive errors and cataract patients [9, 10].
The present study aims to assess contrast sensitivity measurement by SPARCS and compare it with the conventional optotype-based, Pelli Robson chart in glaucoma suspects, established patients of glaucoma with varying severity and age-matched controls. Previous studies with SPARCS do not address the relationship between contrast sensitivity changes and severity of glaucoma, so we address this issue by incorporating visual field-based severity grading of glaucoma in our study.
No previous study in the Indian population has been carried out using SPARCS as a tool for assessing contrast sensitivity in glaucoma patients. The Indian population is different due to its heterogeneous and multilingual nature. A contrast sensitivity tool independent of literacy and language barriers can be easily used in this population, which forms a major chunk of world glaucoma burden. SPARCS is easy and patient friendly, therefore it may decrease the potential patient frustration, loss of valuable time and resources that are currently employed in glaucoma evaluation.
Material and methods
Study design
This prospective observational study enroled consecutive patients who presented to the Glaucoma Clinic of our hospital. The study was approved by the institutional ethics committee and a written, informed consent was taken prior to enrolment. All patients underwent a detailed ocular examination. Patients were evaluated for both eyes, but monocular contrast sensitivity testing was done using an eye patch. The better eye was included in the study based on the Pelli Robson and SPARCS scoring. The study was registered with Clinical Trials Registry of India (CTRI) available online at https://www.ctri.nic.in. The trial registration number is CTRI/2017/05/008488.
Glaucoma was considered present if the patient had evidence of optic nerve damage from either one, or both, of the following: [11]
-
Optic disc or retinal nerve fibre layer (RNFL) structural abnormalities.
-
Reliable and reproducible visual field abnormality.
The fundus examination and visual field and RNFL assessment was done by a trained glaucoma specialist. The glaucoma suspects and the glaucoma patients were classified using parameters that have been described earlier [11, 12]. In order to avoid multiple aetiologies of decreased contrast sensitivity and other factors that could preclude the patient from providing reliable and valid data, patients having pre-existing visually significant cataract and history of incisional surgery in past 3 months were excluded from the study. Patients with neurological disease, diabetic retinopathy and other diseases that could affect contrast sensitivity were also excluded from the study. To ensure that patients with a full range of glaucomatous damage are included, selection was based partially on the amount of optic disc damage. The Disc Damage Likelihood Scale (DDLS) was used to evaluate the extent of optic disc damage caused by glaucoma [13]. The DDLS generates a score from 1 to 10 based on the rim/disc ratio (rather than cup/disc ratio) and the size of the optic nerve. Glaucoma was also graded based on the visual field-based HAP (Hodapp, Anderson and Parrish) grading system using the Humphrey visual field analyser (Carl. Zeiss Meditec Inc., Dublin, CA, USA) and SITA Fast protocol [14]. The intraocular pressure was measured using Goldmann Applanation Tonometer.
Contrast sensitivity assessment
Pelli Robson Test
The Pelli Robson Test is a wall-mounted contrast sensitivity chart and the patients are tested at 1 m. The chart has large Sloan letters that occupy approximately one cycle per degree of vision. The letters are arranged in triplets, which decrease in contrast by 0.15 log units for each triplet. The contrast tested ranges from 100% to 0.56% (log contrast sensitivity 0.00–2.25) [15]. Patients were given credit for a contrast level if they answer two of the three letters in a triplet correctly. Pelli Robson scoring sheets were used to determine the contrast sensitivity. The “letter-by-letter” scoring system was used, whereby each letter correctly identified was scored as 0.05 log units (except for the first triplet, where contrast is 100%). Testing ended when the patient missed two of three letters in a triplet.
Spaeth Richman Contrast Sensitivity Test
SPARCS is performed on a standard computer with internet access [13]. It is designed to be used on a monitor set to 1024 × 768 resolution, 256 grey levels and a size of at least 22 cm width and 26.5 cm height. SPARCS can be accessed via https://www.sparcscontrastcenter.com, where each patient gets a unique identification number. The website provides instructions on how to take the test (Fig. 1a). The patient is seated 50 cm from the computer monitor. At this testing distance, the test occupies 30° of vision horizontally and 23.5° of vision vertically. The central test area subtends 5° horizontally and 3.5° vertically (Fig. 1b). The patient was then instructed to fixate on the central area of the testing screen and identify which of the areas appears different. When the patient was ready, they clicked on the central area.
Vertical square wave gratings with a spatial frequency of 0.4 cycles per degree appear for 0.3 s in one of the five tested areas (Fig. 1c). Patients then temporarily break fixation to select the area that showed the grating. Subsequently, patients fixate again on the central area and click it to activate the programme to show the next image. The area with the gratings appears at random. Correct and incorrect responses are recorded by SPARCS until the software determines the contrast threshold in each area. This typically takes 5–10 min per patient per eye.
The contrast threshold is determined using a staircase strategy with reversals. Initial correct responses advance four levels until an incorrect response was made. After the incorrect response, the contrast level presented is two levels easier. Thereafter, the algorithm advances or regresses one level at a time until two incorrect responses are made at a specific level, which established the threshold. If a patient stops trying to guess the correct area and simply clicks the same location again and again, the test terminates and explains to the patient to attempt to choose the location where the gratings appear. The range of contrast tested is from 100% to 0.45% (log contrast sensitivity 0.00 to 2.35) and decreased by approximately 0.15 log units between levels. The contrast value is calculated by Weber contrast. The central area and four peripheral areas each receive separate scores (Fig. 1d). A total SPARCS score is summated from each of the five areas, making 100 the perfect summed score from all five areas.
To test the reliability of the two tests, monocular testing was performed on each eye twice on the same day. The order of testing was randomised to SPARCS 1, Pelli Robson 1, Pelli Robson 2, SPARCS 2; or Pelli Robson 1, SPARCS 1, SPARCS 2, Pelli Robson 2. The principal investigator explained the test to every patient in his/her vernacular language and administered each test. LED light: 22 W, colour temperature: 6500 K and lumens: 1900Lm was used in the room without daylight to minimise glare.
Statistical analysis
IBM SPSS version 22 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis [16]. Kruskal–Wallis H test with pairwise comparisons was used to assess statistical significance. Association between quantitative explanatory and outcome variables was assessed by calculating Spearman’s rank correlation coefficient. Reliability of different readings of Pelli Robson score and SPARCS score was assessed by calculating intraclass correlation coefficient (ICC) along with its 95% confidence interval and P value. All the ICC values were computed for the entire study group and also for individual subgroup population, that is, normal, disc suspects and glaucoma patients. An ICC value closer to 1 indicates better test–retest reliability. The coefficient of repeatability (COR) values for Pelli Robson Test and SPARCS were also calculated. First described by Bland and Altman, COR is calculated as 1.96 multiplied by the standard deviation of the difference between test and retest scores [17]. A COR value closer to 0 indicates better test–retest repeatability. P value <0.05 was considered statistically significant.
Results and observations
Basic demographics
The study included 135 eyes of 135 patients who were divided into age-matched and sex-matched groups (controls, glaucoma suspects and glaucoma patients) of 45 patients each. The glaucoma group was further subdivided into groups of 15 patients each in the mild, moderate and severe subgroups. The mean age of our study group was 56.93 years. In controls, the mean age was 57.44 ± 11.70 years, in disc suspects 54.22 ± 12.73 years and in glaucoma patients 59.11 ± 12.22 years. There were 78 males and 57 females in the study who were distributed equally in the three study groups and there were 26 males and 19 females in each group.
History
Patients in the glaucoma group had a significant family history of glaucoma (χ2 = 10.352, P = 0.01.) There was no significant difference between the glaucoma severity subgroup subjects on the basis of previous ocular history.
Drugs
There was no statistically significant difference in antiglaucoma drug number between the different severity groups, χ2 = 3.808, P = 0.149.
Best-corrected visual acuity
The distribution of best-corrected visual acuity (BCVA) (LogMAR) was not similar across the study groups, χ2 = 24.651, P < 0.001. In pairwise analysis, BCVA was statistically higher in controls (0.05 ± 0.96) as compared to glaucoma suspects (0.16 ± 0.17, P = 0.004) and glaucoma patients (0.19 ± 0.14, P < 0.001). The distribution of BCVA was also not similar across the glaucoma severity subgroups, χ2 = 7.020, P = 0.03. In pairwise analysis, BCVA was statistically higher when the moderate group (0.13 ± 0.13, P = 0.008) was compared to the severe group (0.27 ± 0.15).
Intraocular pressure
The mean intraocular pressure (IOP) in controls was 15.02 ± 3.201 (10–24) mm Hg, in disc suspects 13.84 ± 3.133 (8–20) mm Hg and in glaucoma patients 13.11 ± 3.099 (6–22) mm Hg. The distribution of IOP was not similar across the study groups, χ2 = 7.020, P = 0.03. In pairwise analysis, the IOP was statistically higher in the control group as compared to the glaucoma group (P = 0.012). The mean IOP for glaucoma subgroup analysis in the mild group was 13.93 ± 2.890 (8–19) mm Hg, in the moderate group 11.67 ± 2.664 (6–15) mm Hg and in the severe group 13.73 ± 3.369 (8–22) mm Hg and there was no statistically significant difference in IOP distribution between the different study groups, χ2 = 4.604, P = 0.100.
Disc Damage Likelihood Scale
The mean DDLS score in controls was 3.22 ± 1.412 (1–4), in suspects 4.93 ± 1.195 (2–6) and in glaucoma patients 7.71 ± 0.991 (7–10). In pairwise analysis, the DDLS was significantly higher in the glaucoma group as compared to the suspects or control group. (P < 0.001 for both, respectively). The mean DDLS score for glaucoma subgroup analysis in the mild group was 7.33 ± 0.976 (6–10), in the moderate group 7.60 ± 0.910 (6–9) and in the severe group 8.20 ± 0.941 (6–9). In pairwise analysis, the DDLS was significantly higher in the severe group as compared to the mild group (P = 0.016).
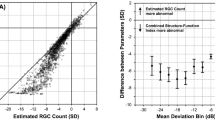
The mean Pelli Robson and SPARCS scores were compared across the subgroups (Table 1). The mean scores in glaucoma patients were comparatively less than those in controls and disc suspects. Similarly, the mean scores in the severe glaucoma patients were less than those in mild and moderate groups. Box and Whisker plots were plotted for the mean scores across the study group and glaucoma severity subgroups (Fig. 2). There is overlap among the groups in the Pelli Robson scores, while SPARCS scores show negligible overlap among the groups. However, in the glaucoma severity subgroup there is considerable overlap in the mean scores for both Pelli Robson and SPARCS scores for mild and moderate glaucoma groups, while mean scores for severe glaucoma are considerably less than mild and moderate groups.
The Spearman’s rank coefficient shows high degree of correlation between Pelli Robson scores (S = 0.905, P < 0.001) and mean SPARCS score (S = 0.975, P < 0.001). There was strong positive correlation between Pelli Robson scores and SPARCS score (S = 0.786 & 0.800, P < 0.001). Moderate degree of correlation was shown between Pelli Robson and SPARCS central component (S = 0.575 and S = 0.623, P < 0.001, respectively).
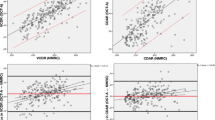
ICC for Pelli Robson was 0.952 and 0.988 for SPARCS. The tests demonstrated excellent repeatability and reliability across all study subject groups (Table 2). SPARCS IN had the best ICC out of the SPARCS component scores in our study group (ICC = 0.966, P < 0.001) and SPARCS ST had the best ICC for the glaucoma severity subgroup (ICC = 0.980, P < 0.001). The COR for mean SPARCS was 5.65%, while COR of Pelli Robson was 12.44%. SPARCS was found to have better repeatability than Pelli Robson based on COR values.
Discussion
Demographics
Our study included 135 eyes of 135 patients with 45 patients in each group; our sample size was comparable to samples used by Gupta et al. [10] (162 eyes of 84 subjects) and Sun et al. [18] (182 eyes of 93 subjects); however, less than the 261 eyes of 157 patients described by Richman et al. [6] in their study. Our sample size was more as compared to the sample size studied by Faria et al. [19] (120 eyes).
The average age of our study group was 56.93 years, which is equivalent to the average age of patients in the Richman et al. [6] study (57.5 years). The average age is also relatively younger to the subjects in the Gupta et al. [10] study and the Faria et al. [19] study. Our patients were age and sex matched into the three groups of controls, disc suspects and glaucoma patients and there was no statistically significant difference between the three groups based on age or sex of the patient.
In our study, we had 58% males and 42% females who were equally distributed in the study groups. All the patients in our study were Asian Indians and thus no racial difference was there in our study.
Previous ocular history
It was however interesting to note that higher SPARCS scores (P = 0.025 and P = 0.045) were associated with phakic eyes than pseudophakic eyes. It is possible that additional factors like the IOL optic material, lens centration or residual refractive error after cataract surgery may account for lower scores in the pseudophakic group [20]. However, the distribution of Pelli Robson scores was found to be equal between phakic and pseudophakic patients (P = 0.068 and P = 0.170) and thus it can be concluded that additional sensitivity of SPARCS for peripheral contrast sensitivity may be the reason for this statistical difference between SPARCS scores for phakic and pseudophakic eyes.
Disc Damage Likelihood Scale
Richman et al. [6] in their study had a mean DDLS score in controls of 2.00 ± 1.0 (1–4), in suspects 3.0 ± 1.5 (1–5) and in glaucoma patients 5.7 ± 2.2 (2–10). The mean DDLS scores in our study controls were 3.22 ± 1.412 (1–4), in disc suspects 4.93 ± 1.195 (2–6) and in glaucoma patients 7.71 ± 0.991 (7–10). The mean DDLS scores for glaucoma severity subgroup analysis in mild group were 7.33 ± .976 (6–10), in moderate group 7.60 ± 0.910 (6–9) and in severe group 8.20 ± 0.941 (6–9). DDLS was significantly higher in the severe group as compared to the mild group (P = 0.016).
Pelli Robson and SPARCS scores
The mean Pelli Robson scores in our study controls were 1.93 ± 0.24, in disc suspects 1.73 ± 0.36 and in glaucoma patients 1.46 ± 0.45, which are similar to those reported by Richman et al. [6]. The mean SPARCS scores in our study were 76.022 ± 6.471, in disc suspects 68.505 ± 7.909 and in glaucoma patients 54.18 ± 12.75, which are also similar to those reported by Richman et al. [6]. For our subgroup analysis, the mean Pelli Robson scores were 1.605 ± 0.331 in the mild group, 1.715 ± 0.139 in the moderate group and 1.106 ± 0.562 in the severe group. The mean SPARCS scores were 58.73 ± 8.680 in the mild group, 62.566 ± 7.949 in the moderate group and 41.27 ± 9.82 in the severe group.
There was strong positive correlation between Pelli Robson scores and SPARCS score (S = 0.786 and 0.800, P < 0.001). Moderate degree of correlation was shown between Pelli Robson and SPARCS central component (S = 0.575 and S = 0.623, P < 0.001, respectively). Our results are similar to those obtained by Faria et al. [19], who reported a Spearman's rank coefficient of 0.80, P < 0.01 for the mean Pelli Robson vs. SPARCS scores. Sun et al. [18] also demonstrated significant correlations between SPARCS and Pelli Robson scores using Pearson's analysis (r = 0.443, P < 0.001).
We also plotted the ROC curves for the two tests (Fig. 3a, b). In our study, a Pelli Robson score <1.80 had a sensitivity of 80% and a specificity of 65.6% for detecting glaucoma patients and SPARCS score <67 had a sensitivity of 84.4% and a specificity of 70% for detecting glaucoma patients. Our results are comparable to those obtained by Richman et al. [6]. They reported that a Pelli Robson score of 1.35 or less provided 80.5% sensitivity and 76.0% specificity for glaucoma and a SPARCS score of <70 had 79.7% sensitivity and 92.8% specificity for glaucoma.
We summarise the findings of previous studies using Pelli Robson Test and SPARCS in Table 3.
The findings of our study confirm that contrast sensitivity measurement obtained by SPARCS and Pelli Robson Test have good agreement and may be used interchangeably. SPARCS also appears to be more sensitive to glaucomatous damage as compared to Pelli Robson Test and seems to have better test–retest repeatability based on COR and ICC values.
Conclusion
Our study thus confirms the reliability and repeatability of SPARCS in the heterogeneous multilingual Indian population. SPARCS and Pelli Robson Test demonstrate high degree of correlation and thus can be used interchangeably for assessment of contrast sensitivity. Pelli Robson Test being an optotype chart-based test has its fallacies like inadequate and unequal illumination, reflections from chart surface, chart fading, need of literate patients and above all significant cost of installation and maintenance. SPARCS on the other hand is based on gratings and hence is independent of the effects of literacy and intelligence. It measures both central and peripheral contrast sensitivity and thus appears to be more sensitive for diseases like glaucoma where peripheral loss of retinal function occurs. SPARCS being a computer-based test offers more accessibility and thus is a better alternative for contrast sensitivity assessment.
There are however certain fallacies in our study like small sample size, presence of alternate factors such as topical antiglaucoma drug use and lower BCVA in the glaucoma group. The lack of monitoring of luminance of the Pelli Robson chart and SPARCS computer screen also can be accounted for in future studies by using a gamma function assessment that can further standardise low levels of contrast in non-standardised testing environment.
Further studies are needed to analyse the effects of additional factors like intraocular pressure, systemic diseases, topical antiglaucoma drugs and intraocular lens type on contrast sensitivity scores before SPARCS can replace Pelli Robson Test as the gold standard for contrast sensitivity testing.
Summary
What was known before
-
SPARCS can be used in glaucoma patients as an alternative to Pelli Robson Test for assessment of contrast sensitivity.
-
The test is reliable and repeatable in the Caucasian and African population.
What this study adds
-
SPARCS can be used in patients with varying severity of glaucoma.
-
SPARCS maintains its reliability in the Asian Indian population.
-
The study add data to the fact that the current gold standard for contrast sensitivity needs to be replaced with newer and more accurate/reliable tests such as SPARCS.
References
Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–7.
Quigley HA, Addicks EM, Green WR. Optic nerve damage in human glaucoma. III. Quantitative correlation of nerve fiber loss and visual field defect in glaucoma, ischemic neuropathy, papilledema, and toxic neuropathy. Arch Ophthalmol. 1982;100:135–46.
Broadway DC. Visual field testing for glaucoma—a practical guide. Community Eye Health. 2012;25:66–70.
Richman J, Spaeth GL, Wirostko B. Contrast sensitivity basics and a critique of currently available tests. J Cataract Refract Surg. 2013;39:1100–6.
George L, Spaeth. Validation and reproducibility of Spaeth/Richman Contrast Sensitivity Test 2014 [updated 29 January 2015; cited 10 October 2015]. https://www.clinicaltrials.gov/ct2/show/study/NCT01300949.
Richman J, Zangalli C, Lu L, Wizov SS, Spaeth E, Spaeth GL. The Spaeth/Richman contrast sensitivity test (SPARCS): design, reproducibility and ability to identify patients with glaucoma. Br J Ophthalmol. 2015;99:16–20.
Richman J, Lorenzana LL, Lankaranian D, Dugar J, Mayer JR, Wizov SS, et al. Relationships in glaucoma patients between standard vision tests, quality of life, and ability to perform daily activities. Ophthalmic Epidemiol. 2010;17:144–51.
Shoshani YZ, Harris A, Rusia D, Spaeth GL, Siesky B, Pollack A, et al. Contrast sensitivity, ocular blood flow and their potential role in assessing ischaemic retinal disease. Acta Ophthalmol. 2011;89:e382–95.
Sun Y, Erdem E, Lyu A, Zangalli C, Wizov SS, Lo D, et al. SPARCS: a novel assessment of contrast sensitivity and its validity in patients with refractive error. Invest Ophthalmol Vis Sci. 2014;55:2711.
Gupta L, Cvintal V, Delvadia R, Sun Y, Erdem E, Zangalli C, et al. SPARCS and Pelli–Robson contrast sensitivity testing in normal controls and patients with cataract. Eye. 2017;31:753–761.
Prum BE Jr, Rosenberg LF, Gedde SJ, Mansberger SL, Stein JD, Moroi SE, et al. Primary Open-Angle Glaucoma Preferred Practice Pattern((R)) Guidelines. Ophthalmology. 2016;123:P41–P111.
Prum BE Jr., Lim MC, Mansberger SL, Stein JD, Moroi SE, Gedde SJ, et al. Primary Open-Angle Glaucoma Suspect Preferred Practice Pattern((R)) Guidelines. Ophthalmology. 2016;123:P112–51.
Henderer JD. Disc damage likelihood scale. Br J Ophthalmol. 2006;90:395–6.
Anderson D, Patella V. Automated static perimetry. 2 ed. St Louis: Mosby; 1999.
Pelli DG, Robson JG, Wilkins AJ. The design of a new letter chart for measuring contrast sensitivity. Clin Vision Sci. 1988;2:187–99.
Machines IB. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp; 2013.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
Sun Y, Erdem E, Lyu A, Zangalli C, Wizov SS, Lo D, et al. The SPARCS: a novel assessment of contrast sensitivity and its reliability in patients with corrected refractive error. Br J Ophthalmol. 2016;100:1421–6.
Faria BM, Duman F, Zheng CX, Waisbourd M, Gupta L, Ali M, et al. Evaluating Contrast sensitivity in age-related macular degeneration using a novel computer-based test, the Spaeth/Richman Contrast Sensitivity Test. Retina. 2015;35:1465–73.
Ohtani S, Miyata K, Samejima T, Honbou M, Oshika T. Intraindividual comparison of aspherical and spherical intraocular lenses of same material and platform. Ophthalmology. 2009;116:896–901.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Thakur, S., Ichhpujani, P., Kumar, S. et al. Assessment of contrast sensitivity by Spaeth Richman Contrast Sensitivity Test and Pelli Robson Chart Test in patients with varying severity of glaucoma. Eye 32, 1392–1400 (2018). https://doi.org/10.1038/s41433-018-0099-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-018-0099-y
This article is cited by
-
Correlation of contrast sensitivity with ganglion cell/inner plexiform layer thickness and damage location in glaucoma with varying severity
Eye (2023)
-
Analysing the change in contrast sensitivity post-travoprost treatment in primary open-angle glaucoma patients using Spaeth Richman contrast sensitivity test
International Ophthalmology (2022)
-
Association of ocular blood flow and contrast sensitivity in normal tension glaucoma
Graefe's Archive for Clinical and Experimental Ophthalmology (2021)