Abstract
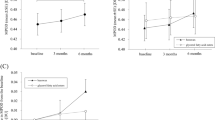
Carotenoids are lipophilic isoprenoid pigments with a common C40H56 core chemical structure that are naturally synthesized by many plants, algae, bacteria, and fungi. Humans and animals cannot synthesize carotenoids de novo and must obtain them solely through dietary sources. Among the more than 750 carotenoids in nature, only lutein, zeaxanthin, meso-zeaxanthin, and their oxidative metabolites selectively accumulate in the foveal region of the retina where they are collectively referred to as the macular pigment (MP) of the macula lutea. MP serves an ocular protective role through its ability to filter phototoxic blue light radiation and also via its antioxidant activity. These properties have led to the hypothesis that carotenoids may protect against the development of age-related macular degeneration (AMD), the most common cause of blindness in the aged population >60 years old. Epidemiological studies have supported this by showing that patients with lower concentrations of serum carotenoids and macular pigment optical density (MPOD) measurements are at a higher risk of developing AMD. Conversely, nutritional supplementation and diets rich in lutein and zeaxanthin readily impact MP concentrations and reduce the risk of progression to advanced AMD, and the AREDS2 supplement formulation containing 10 mg of lutein and 2 mg of zeaxanthin is the standard-of-care recommendation for individuals at risk for visual loss from advanced AMD. This article reviews the rich history of research on the MP dating back to the 1700s and outlines their potential for further therapeutic improvements for AMD in the future.
Similar content being viewed by others
Macular pigment background, history, and relationship to AMD
Structure and chemistry of the macular pigment (MP)
The unique structure of each carotenoid defines its physical, chemical, and biological properties. The macular carotenoids belong to the xanthophyll family with a molecular formula of C40H56O2. They have a conjugated double-bond backbone and cyclohexene end groups with hydroxyl group attached at the 3 and 3ʹ positions. The chemical structures of the macular carotenoids are shown in Fig. 1. Their rigid conjugated double-bond structure is responsible for carotenoid color and their ability to quench free radicals and reactive oxygen species. The macular xanthophyll carotenoids are relatively more polar compared to carotenes due to the presence of hydroxyl (O–H) groups which alter their polarity and solubility and also contribute to their antioxidant properties [1]. The hydroxyl functional group permits MP and its isomers to cross the blood-brain and blood-ocular barriers, and the position and chirality of the hydroxyl groups of MP contribute to their differences in absorption, transport, metabolism, tissue uptake, and potential orientation in bilayer membrane relative to each other and relative to other carotenoids [2]. The MP carotenoids also differ from each other by the location of one double-bond. The double-bond at the 4ʹ, 5ʹ position in lutein is shifted to 5ʹ, 6ʹ position in zeaxanthin and meso-zeaxanthin. Lutein exists in eight stereoisomeric forms as a result of three stereocenters at C-3, C-3ʹand C-6ʹ, but the lutein component of the MP consists of a single stereoisomer, (3R, 3ʹR, 6R)-β,ε-carotene-3,3ʹ-diol. Zeaxanthin has three stereoisomers which include RR-zeaxanthin [(3R, 3ʹR) - β, β -carotene-3, 3ʹdiol] (dietary zeaxanthin), SS-zeaxanthin [(3S, 3ʹS) β, β- carotene-3, 3ʹ-diol] (found only in trace amounts in nature), and meso-zeaxanthin [(3R, 3ʹS)- β, β -carotene-3,3ʹ diol] (rarely found in nature outside of the primate fovea). The position of the hydroxyl group at the 3ʹ carbon of lutein is classified as more allelic compared to zeaxanthin and meso-zeaxanthin [3].
MP distribution and orientation
Currently, 750 carotenoids have been identified in nature, but only about 40 carotenoids are found in major human foods. About 15 carotenoids have been identified in human blood and tissues, but only lutein, zeaxanthin, and their metabolites are detected in the human retina [4]. MP has a unique distribution in the retina with high concentrations in the fovea and inner plexiform layer of the retina (Fig. 2). The foveal Henle fiber layer has the highest concentration of MP at around 0.1 to 1 mM, and its concentration declines rapidly with increasing eccentricity. The ratio of lutein: zeaxanthin is 1:2.4 in the center (0–0.25 mm) to over 2:1 in the periphery (8.7–12.2 mm) of the human retina. There is a 100-fold drop in the macular pigment concentration in the peripheral retina compared to the fovea, although the MP levels vary widely between individuals. The variation in MP ratio with eccentricity has been linearly correlated with the corresponding rod and cone ratio [5]. Lutein and its isomers adopt perpendicular and parallel orientations to the plane of biological membranes, whereas the zeaxanthins adopt a perpendicular orientation to the plane of the membrane [6]. Transmembrane orientations of lutein and zeaxanthin have been shown to decrease the membrane’s susceptibility to lipid oxidation and enhance the rigidity of lipid bilayer and thus act as ‘molecular rivets’.
Biological function of MP against AMD
MP has its peak absorption at 460 nm (Fig. 3) where it can absorb 40–90 % of incident high-energy, short-wavelength visible light depending on its concentration [7]. A primary function of MP is the reduction of blue-light scattering in the central retina, and the deep yellow color and anatomical location of MP are thought to be ideal to protect the foveal region from photo-oxidative damage. While all MP molecules attenuate blue-light exposure, lutein filters blue light more efficiently than zeaxanthin and meso-zeaxanthin due to its orientation within the lipid bilayer [6], and primates fed with a xanthophyll-free diet from birth are more prone to blue-light induced damage [8]. Photoreceptor cells are more prone to oxidation than other cells in the retina and rely on the carotenoids for protection due to their greater oxidative stability. Chucair et al. demonstrated that rat retinal neurons treated with macular carotenoids have greater protection from oxidative stress than an untreated group [9]. The identification of lutein and zeaxanthin oxidative metabolites in the retina by Khachik et al. further supports the function of macular pigment in retinal oxidative protection [4].
Dietary sources of lutein and zeaxanthin
MP is not synthesized de novo in animals and must be obtained by dietary ingestion. Several studies have shown that increased dietary consumption of lutein and zeaxanthin results in a lower incidence of AMD [10,11,12]. Green leafy vegetables (spinach, parsley, kale, lettuce, broccoli, zucchini, etc.), orange-yellow fruits (orange, tangerine, papaya, and mango) are superior sources of macular carotenoids [13, 14]. Among cereals, durum wheat, corn, and their byproducts contain lutein and zeaxanthin [15, 16]. In animals, lutein and its isomers are mainly found in egg yolk, fish skin, carapace (shell) of crustaceans, and in the skin and integuments of birds. Among macular carotenoids, lutein is the most common carotenoid found in food sources. Zeaxanthin is found in smaller quantities, and meso-zeaxanthin rarely exists in the human diet. In 1986, Maoka et al. first reported the presence of meso-zeaxanthin in shrimp carapace, fish skin, and turtle fat [17]. In the past, due to difficulties in separating lutein from zeaxanthin, the carotenoid concentration in the foods was often termed as the sum of lutein and zeaxanthin (L+Z). As HPLC methods improved, lutein could be reliably separated from other MP carotenoids, but zeaxanthin and meso-zeaxanthin still co-eluted. It was not until the development of chiral chromatography that meso-zeaxanthin could be successfully separated from dietary zeaxanthin [18, 19]. Lutein and zeaxanthin supplementation is generally recognized as safe (GRAS) for human consumption, and the European Food Safety Authority (EFSA) recently accepted that consumption of 1 mg/kg of bodyweight of lutein with 80% total carotenoids content derived from marigold (Tagetes erecta) is safe. The no observed adverse effect level (NOAEL) for lutein and zeaxanthin is 400 mg/kg of bodyweight/day [20], and for meso-zeaxanthin it is 300 mg/kg of bodyweight/day [21]
Identification of the macular pigment
More than two centuries ago, the initial observation of yellow pigmentation in the central retina of humans was reported by Buzzi in 1782 [22]. Later, Soemmering discovered the foramine centrali limbo luteo (the central yellow-edged hole) in 1795 [23]. Home and Sommering made a detailed review on the macula lutea in 1798 [24]. They also reported that the yellow spot was not found in dissections of any animals other than humans and primates. This was the first evidence that macular pigment is exclusive to humans and primates. In 1866, the idea that MP may filter blue light and protect against harmful short wavelength radiation was first described by Max Schultze [25]. In 1945, Wald remarked that MP exhibited a characteristic carotenoid spectrum and concluded that the pigment belongs to the xanthophyll family of carotenoids [26]. Forty years later, Bone et al. (1985) first characterized the MP using high-performance liquid chromatography (HPLC) and reported that MP consists of two distinct dietary xanthophyll carotenoids, lutein and zeaxanthin [27], and this was later confirmed by Handelman et al. in 1988 [28]. The third and final component of MP, meso-zeaxanthin, was identified in retina by Bone et al. in 1993 [3]. The cross-sectional location of MP within the retina had not been clarified until Snodderly et al. localized the xanthophyll pigments to the Henle fiber layer [29]. Bernstein et al. in 2001 reported that carotenoids are not only located in the macula but are also present in the human lens and in virtually all the tissues of human eyes [30]. The origin of meso-zeaxanthin within the macula had not been elucidated until Johnson in 2005 reported that dietary lutein is the precursor for meso-zeaxanthin based on feeding studies of carotenoid-depleted monkeys [31]. Johnson’s finding was further confirmed by Bhosale et al., where they fed deuterium-labeled lutein and zeaxanthin supplements to quail and determined that dietary lutein is the precursor for meso-zeaxanthin and that dietary zeaxanthin is the precursor for 3ʹoxolutein, β-apo-2ʹ-carotenol, adonirubin, astaxanthin, galloxanthin, and ε,ε-carotene [18]. Recently, Shyam et al. identified RPE65 as the isomerase enzyme responsible for conversion of dietary lutein to meso-zeaxanthin in the retinal pigment epithelium of vertebrates [32].
Bioavailability of MP
Carotenoid bioavailability is one of the vital factors affecting its biological functionality and effectiveness. Bioavailability is termed as the ‘fraction of ingested nutrients that is available for normal physiological function or storage.’ The fraction of ingested carotenoids that becomes available for physiologic function is highly variable, and it depends on the source and amount of carotenoid consumed and the influence of other dietary factors [33]. Despite their various health benefits, macular carotenoids are poorly bioavailable due to their hydrophobicity. Carotenoid intestinal absorption involves several steps starting with the mechanical and enzymatic disruption of carotenoids from the food matrix, its release into the aqueous solution, followed by its incorporation into lipid droplets, and transfer to mixed micelles. Carotenoids in mixed micelles are absorbed by the intestinal cells via passive or facilitated absorption. Until the discovery of SR-B1 protein and CD36, researchers believed that carotenoid absorption took place by simple diffusion. The carotenoid cleavage enzymes, β-carotene-15,15′-oxygenase (BCO1) which cleaves carotenes symmetrically at the 15-15ʹ C = C results in formation of retinal from β-carotene, but BCO1 cannot cleave MP carotenoids due to lack of one non-substituted β-ionone ring, a requirement for BCO1’s cleavage activity. BCO2 cleaves xanthophyll carotenoids at the 9ʹ, 10ʹ C = C, resulting in formation of three possible cleavage products: 10ʹ- apo-β-carotenol (C27), β-ionone (C13), and a dialdehyde (C9). BCO2 is relatively inactive in humans, and as a result, lutein and zeaxanthin are stable in humans as opposed to mice where a very active BCO2 cleaves ingested xanthophylls [34]. Next, the uncleaved MP are packed into chylomicrons and transported into the lymphatic system to the liver and then transported to targeted tissues by the general circulation [35].
Each step of carotenoid absorption is influenced by various factors, making it difficult to assess the effects of each factor on overall carotenoid bioavailability [36, 37]. The key factors that affect carotenoid bioavailability are Species of carotenoid, molecular Linkage, Amount of carotenoids consumed, carotenoid Matrix, Effectors of absorption and bioconversion, Nutrient status of the host, Genetic and host-related factors, and mathematical Interactions (collectively known by the acronym SLAMENGI) [36]. There are several studies showing that addition of lipid improves the absorption of macular carotenoids [38, 39]. A complex food matrix also influences carotenoid bioavailability, as carotenoid uptake from oil-based supplements show better bioavailability than from whole vegetable sources [40]. Dietary fiber inhibits macular carotenoid absorption by entrapping them and also inhibiting lipase activity and micelle formation [38]. The presence of other carotenoids such as β-carotene leads to competition for incorporation into micelles and reduction of macular carotenoid absorption [41].
Rodents have been extensively used as animal models for carotenoid research. In one of the earlier reports, High and Day (1951) evaluated the effect of carotenoids on vitamin A storage and growth rate in rats [42]. Several studies have been reported on the bioavailability of xanthophylls in the rodent models [38, 43]. Due to species variations and other factors influencing carotenoid bioavailability, researchers are moving towards the genetically modified knockout mice models to obtain a better model for carotenoid metabolism. The genetically engineered ‘macular pigment mouse’ model with knockout of BCO2 was developed to study the protective effects of MP in genetic and environmental models of human ocular disease. In contrast to humans, wild-type mice have very active BCO2 xanthophyll cleaving enzymes, resulting in no detectable accumulation of macular carotenoids in their retinas. An unusual insertion of—GKAA—amino acids near the substrate binding tunnel appears to be unique to primate BCO2 and insertion of this sequence into the mouse enzyme leads to its inactivation; germ-line knockout of mouse BCO2 results in MP deposition in the mice retina [34, 44]. Non-human primates are considered even better models to study carotenoid metabolism, but their high cost of care, space requirements, and handling difficulties limit their use. Birds are also used for MP research, but they differ significantly from humans due to a broader diversity of carotenoids, many of which are esterified to long-chain fatty acids and deposited in oil droplets, making them difficult to extract and analyze without artifacts.
Macular carotenoid binding proteins and MP transport to retina
Lipoproteins such as low density lipoprotein (LDL), high density lipoprotein (HDL), very low density lipoprotein (VLDL) and chylomicrons and chylomicron remnants and their receptors CD36 and SRB1 are involved in macular carotenoid uptake [45]. In vitro studies using intestinal caco-2 cells suggested the possible role of receptor proteins during the process of carotenoid uptake [46]. Scavenger receptor class B member 1 (SR-BI), a cell surface glycoprotein and a non-specific lipid transporter, is involved in the competitive uptake of carotenoids in the gut prior to transport to the liver by chylomicrons. Recently, Lobo et al. reported the presence of ISX (intestine-specific homeobox), a transcription factor that governs carotenoid absorption via SR-B1 and BCO1 mRNA expression, which is regulated by a carotenoid metabolite, retinoic acid [47]. Several studies have revealed that SR-B1 and CD36 can function as carotenoid transporters into the retina [48, 49]. The role of the third SR-B family member, SR-B2, in carotenoid transport was not clear until Shyam et al. reported that all three human SR-B proteins (SR-B1, SR-B2, and CD36) were capable of binding all three macular carotenoids, and once delivered to the retina, they are stabilized by the presence of high levels of specific binding proteins in the macula [48].
While 15 unique carotenoids have been identified in human blood and tissues, the selective uptake and accumulation of lutein and zeaxanthin in the human retina had puzzled the scientific community until the discovery of their binding proteins. Tubulin, a water-soluble, low specificity carotenoid binding protein was identified by Bernstein et al. in 1997 [50]. Tubulin proteins are found abundantly in the photoreceptor axon layer of the fovea and may be involved in the high concentration and stabilization of MP in the retina, but they exhibit relatively weak and non-specific binding affinity for MP, so the search continued for more specific, higher affinity macular carotenoid binding proteins. Using human macular membrane preparations, glutathione S transferase P1 (GSTP1) was identified as a zeaxanthin-binding protein, and subsequent research revealed that GSTP1 protects the lipid membrane from oxidation [51]. Out of 15 known human steroidogenic acute regulatory domain proteins, steroidogenic acute regulatory domain protein 3 (StARD3) also known as metastatic lymph node 64 protein (MLN64) was identified as a lutein-binding protein [52]. The macular distributions of MP and its binding proteins are shown in Fig. 4. The macular carotenoids share retinoid transporters such as interphotoreceptor retinoid binding protein (IRBP) and retinol binding protein 4 (RBP4) in the process of transport of MP from serum to retina [53]. MP uptake is selective and the possible pathways for MP carotenoid uptake, transport, and accumulation in the human retina are shown in Fig. 5.
The retinal distribution of macular pigment binding proteins. a GSTP1 labeling of foveal cones in the macula of a 3-year-old monkey. This montage shows strongest labeling by antibody against GSTP1 (red) over the myoid and ellipsoid regions of cones identified by monoclonal antibody (7G6, green). b A low-magnification view of a near-foveal retina section in which N-62 StAR (red) identifies StARD3, an anti-cone arrestin monoclonal antibody (7G6, green) identifies monkey cones. Images courtesy of Dr. Jeanne M. Frederick
HDL, LDL, VLDL and albumin play an important role in transport of these carotenoids to their respective target sites. Carotenes such as β-carotene and lycopene are highly hydrophobic and are transported on LDL, whereas lutein and zeaxanthin are hydrophilic and are transported by HDL [54]. Chickens with a natural genetic defect of HDL (the Wisconsin hypoalpha mutant, WHAM) chicken fed with high levels of lutein in the diet has high levels of lutein in plasma, liver, heart, egg yolk but not in retina, suggesting that HDL is critical for delivery of lutein to the retina [55]. Genetic variations in CD36 and BCO1 can modulate plasma lutein and retinal concentrations [56].
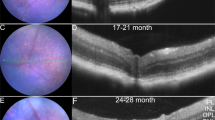
Age-related macular degeneration (AMD)
AMD is an acquired, degenerative disorder of the macula that is the leading cause of irreversible blindness and visual disability in people greater than 60 years of age. AMD accounts for 8.7 % of all legal blindness across the globe [57]. By the end of 2020, the patients with AMD in the United States alone will exceed 3 million [58]. AMD can be classified into two forms: non-exudative (dry) and exudative (wet), and fundus images of both the dry and the wet forms compared to a normal eye are shown in Fig. 6. The dry form is characterized by the accumulation of drusen under the macular retina caused by photo-oxidative damage of lipids and proteins along with depigmentation of the retinal pigment epithelium (RPE). The wet form is characterized by sub-RPE, sub-retinal, or intraretinal neovascularization from blood vessels originating in the choriocapillaris that have broken through Bruch’s membrane. This vascular abnormality leads to macular edema, sub-retinal fluid, hemorrhage, and eventual fibrosis, resulting in permanent loss of macular vision. AMD is a complex, multifactorial disease, and its pathogenesis is not yet clearly understood. AMD has a high cost to society and patient quality of life, hence prevention has important public health implications. Hereditary is one of the major risk factors, with risk loci on chromosome 1 in the complement factor H region [59] and on the chromosome 10 in the HTRA1/ARMS2 region [60]. Advanced age is an obvious risk for AMD, with a sharp increase in prevalence in those older than 75 years of age. Other unmodifiable risk factors of AMD are female gender, light complexion, and light-colored irides. Strategies to ameliorate AMD have been based on reduction of modifiable risk factors. Smoking is considered the most important environmental risk factor. Oxidative stress, excessive light exposure, poor nutritional status, hypercholesterolemia, and hypertension are also strongly correlated with AMD.
AREDS
Through the better understanding of antioxidant macular carotenoids, vitamins, and minerals gained over the previous decades, evaluation of epidemiological data suggested that patients with higher serum concentrations of antioxidants had a significantly lower risk of developing neovascular AMD. The Eye Disease Case–Control Study group compared over 350 patients with advanced AMD with 520 matched, control subjects from similar geographic areas without AMD to identify relationships between carotenoid dietary intake and risk for AMD. The study group determined that an increased dietary intake of carotenoids, particularly spinach and collard greens, was strongly associated with decreased risk for AMD a 42% decrease in risk between the highest and lowest quintile of carotenoid ingestion [12]. There was no significant benefit of vitamin A, C, or E intake; however, there was a trend in risk reduction with high vitamin C intake from food sources. Additional large epidemiologic prospective studies have associated increased lutein and zeaxanthin intake with a decreased long-term risk of advanced AMD [10].
There have been numerous small interventional studies looking at the role of carotenoids and other nutrients in the prevention of AMD that have been reviewed elsewhere [61], but clinicians generally rely on large, randomized, prospective trials to guide clinical practice, so we will concentrate on the AREDS and AREDS2 studies. The Age-Related Eye Disease Study (AREDS) [62] was commenced by the National Eye Institute in 1990 to study whether supplementation with antioxidants would alter the development and/or progression of AMD. This double-masked, randomized trial enrolled participants at 11 centers with extensive drusen of small, intermediate, or large size, geographic atrophy, or pigment abnormalities in one or both eyes. Additionally, patients with advanced AMD or vision loss from AMD in one eye were enrolled. The aim of the AREDS trial was to evaluate the effect of zinc and other antioxidant vitamins in doses 5 to 15 times greater than the recommended daily allowance in the progression of advanced AMD in older adults. The AREDS formulation was selected through the recommendations of an expert panel of nutritionists, biochemists, and ophthalmologists at National Eye Institute sponsored meetings. β-Carotene (15 mg (25,000 IU/day) was included in the formulation as it was commercially available at the time, unlike lutein and zeaxanthin. β-carotene was well-established in ophthalmic nutritional supplements, and its antioxidant properties were well-documented, although only trace amounts are actually found in the retina. The antioxidant vitamins C (500 mg/day) and E (400 IU/day) were also included. A randomized, placebo-controlled trial of zinc supplementation had reported a significant reduction (P < 0.05) in visual acuity loss in the group supplemented with zinc; therefore, zinc oxide (80 mg/day) was included in the mineral arm of the AREDS. Copper oxide (2 mg/day) was selected to prevent a copper-deficiency anemia caused by high serum zinc levels [63].
At the 5-year mark, the probability of progression to advanced AMD was 20% for those assigned to antioxidants plus zinc compared to 28% of study participants assigned to placebo, 23% in the antioxidants group, and 22% in the zinc group [62]. By the time these results were published in 2001, there had been a significant leap forward in the nutritional understanding of AMD since the study had commenced, thus highlighting the need for the AREDS2 clinical trial [63]. Also, there was new evidence during the course of AREDS trial that β-carotene supplementation was associated with an increased risk for lung cancer in smokers [64, 65]. This raised concerns about the inclusion of β-carotene in the AREDS formulation, as almost 50% of the US population at risk for AMD are former or current smokers [63].
Clinical research on macular pigment in the present
AREDS2
The AREDS2 supplement formulation was introduced into the market following the conclusion of the study in 2001. This formulation has since become the standard-of-care for those at risk for visual loss from AMD. AREDS2 was started in 2006 to evaluate the addition of lutein, zeaxanthin, and omega-3 long-chain polyunsaturated fatty acids into the AREDS formula. There was also a lower zinc content (25 mg) subgroup, as there was evidence that no greater amount could be absorbed and that high levels of zinc may result in genitourinary-related hospital admissions [66, 67]. Current and former smokers were enrolled into subgroups without β-carotene. Subgroup analysis of individuals in the entire study cohort that received lutein and zeaxanthin compared with individuals who did not receive lutein and zeaxanthin showed a statistically significant (P < 0.05) decrease in progression to advanced AMD [68]. Further analysis comparing groups receiving lutein and zeaxanthin without β-carotene and groups receiving β-carotene without lutein and zeaxanthin showed a significant (P < 0.05) reduction in progression to advanced AMD, particularly development of neovascular AMD [68]. However, the AREDS2 formulation was unable to meet the ambitious goal of an additional 25% reduction in progression to advanced AMD above the already effective AREDS formulation, but it was a safer and at least as efficacious option, specifically in former and current smokers [63]. In contrast to other published results [69], AREDS2 did not demonstrate any benefit or harm with omega-3 fatty acid supplementation in AMD.
No evaluation of MP in any fashion was performed in AREDS or AREDS2. In vivo, image-based instrumentation during the time period of these trials was not sufficiently standardized or widespread in the clinical domain [63], and psychophysical methods were considered too time-consuming to add to the already long study visits. Patients enrolled in an ancillary AREDS2 study from the Moran Eye Center, Salt Lake City, Utah, underwent MPOD and MP spatial distribution imaging and total skin carotenoid measurement by resonance Raman spectroscopy prior to the start of the AREDS2 trial [70]. They found that enrolled patients had higher than average baseline MPOD measurements than an age-matched control group, likely due to enrollment of patients taking eye supplements containing lutein and zeaxanthin for many years prior.
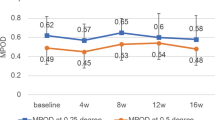
Modalities to clinically measure MP
From the findings of large epidemiological studies and AREDS2 that found a reduced risk of AMD progressing to advanced form with higher carotenoid consumption, groups became interested in attempting to quantify macular pigment concentrations to identify patients at risk of developing AMD [10, 62, 68]. Several measurement modalities have been proposed and have been compared elsewhere [71]. The use of high-performance liquid chromatography (HPLC) is the gold standard analytical method to measure MP within the eye, but it is tissue destructive, time-consuming, and provides little-to-no spatial distribution information [18]. Consequently, several less invasive techniques have been designed as biomarkers of MP concentrations, but unfortunately, no technique is perfect. There are two types of methods for measuring MP in living humans: psychophysical and physical. Heterochromatic flicker photometry (HFP) and other related psychophysical methods require test subjects to make iso-iluminance matches between flickering green and blue lights to measure MP at one or a few eccentricities; however, this technique requires significant patient training to produce meaningful results. HFP also provides little information on spatial distribution of MP [61]. Despite the technical expertise required and the relative lack of spatial information gleaned, the technique can be reliably used to detect changes in macular pigment optical density in patients taking oral supplementation [72]. Standardized protocols have been designed to ease the difficulty in both administering and performing the test, and pre-adolescent children can also reliably perform the test [73, 74]. However, due to the difficulty and expertise required in administering the test, researchers have subsequently tried to identify other image-based methods to measure MP objectively.
Imaging-based techniques such as reflectometry, autofluorescence attenuation, and resonance Raman spectroscopy have gained interest, as they are less technically demanding tests to administer and provide high-resolution, quantitative spatial distributions of MP. Raman spectroscopy uses the Raman Effect in which photon scattering by molecules results in a measurable shift in wavelength specific to the chemical structure. Fundus autofluorescence exploits the fluorescent properties of lipofuscin and the predictable attenuation of the fluorescence by MP. Reflectometry, or fundus reflectance, measures reflected light from the retina and choroid and then uses complex mathematical models to derive MP data. There has been concern that these methods maybe affected by visual axis opacities (e.g., cataract) and are quite expensive to manufacture [61]. Fortunately, most of these methods have been shown to correlate with other previously mentioned techniques including HFP [71, 75]. There has been notable measurement discordance between HFP and reflectometry-based techniques [75].
In regards to dual wavelength autofluorescence (Fig. 7), we have found that volumetric measurements appear to be superior to previously used optical densities in regards to their correlative power with other carotenoid measurement techniques [71]. Groups have argued that visual axis opacities such as cataracts may alter measurements; however, we did not find a significant ‘cataract effect’ on volume measurements [71, 76]. The technique is also highly reproducible even in the face of significant ocular pathology such as exudative AMD and diabetic macular edema [71]. Unfortunately, dual wavelength autofluorescence is not perfect either, as it requires pupillary dilation and expensive equipment to obtain the measurements.
Macular pigment readout from an unsupplemented normal control obtained by dual wavelength autofluorescence imaging on a Heidelberg Spectralis. a Macular pigment tracing at 0.5° (red line), 2° (blue line), and 9° (green line). b Autofluorescent image showing the fovea and the degrees (0.5°, red; 2°, blue; 9°, green) from the center of the macula lutea
Others have attempted to use systemic measurements of carotenoids as a surrogate for ocular concentrations. These methods include HPLC analysis of serum, dietary assessments, and skin resonance Raman spectroscopy. Unfortunately, HPLC requires time-consuming extractions and analyses, and prior attempts at using dietary assessments have shown that they are both tedious and fraught with recall errors and bias. While skin Raman spectroscopy can be easily performed, it cannot readily differentiate various carotenoids and requires specialized equipment; it correlates well with HPLC total serum, biopsied skin tissue, and volumetric concentrations obtained by dual wavelength autofluorescence [71]. While there are numerous techniques available to quantify MP both invasively and non-invasively, each technique is hindered by either its availability, cost of production, and/or expertise in implementation. As more individuals become interested in MP and how to measure it, the need for readily available equipment will become even more significant.
Visual performance improvement after carotenoid ingestion
Over the last decade, we have seen the development of psychophysical visual function research and the correlation of MP density with visual performance in AMD. While a majority of research on carotenoids has focused on identifying ways to quantify risks associated with AMD, emerging data from randomized, placebo-controlled, double-blinded studies have demonstrated a correlation between increases in MP optical density with improvement in visual function. This is hypothesized to also be due to the short wavelength filtering effects of MP, resulting in reduced glare, light scatter, and chromatic aberration, thereby enhancing contrast sensitivity [61]. Several randomized, controlled trials have corroborated this, with the most striking responses found in individuals with the lowest baseline MP concentrations [77]. Thus, there appears to be a beneficial role of MP supplementation in both diseased and healthy retinas; however, it is possible to develop a crystalline maculopathy from extreme supplementation [78]. While improvements in best corrected visual acuity (BCVA) are not commonly observed, gains in contrast sensitivity is significant bright light and low light contrast sensitivity, letter contrast sensitivity, glare disability, and mean reading speed showed significant association with MP after controlling for age, sex, and cataract changes [79]. Prior studies have shown that individuals who use computers or smartphones >6 h per day have benefited from carotenoid supplementation in not only increased visual performance measures, but also increased sleep quality, reduced headaches, less eye fatigue, and decreased photophobia [80, 81]. While no significant difference was measured in the National Eye Institute Visual Functioning Questionnaire 25 survey [79, 82], data exist to support contrast sensitivity as a better marker of real-world vision than BCVA [83, 84]. Consequently, macular pigment supplementation may be beneficial even to those without AMD.
The future of AMD and MP
Since the discovery of MP, there has been tremendous information and knowledge gathered about MP and its role in ocular health, particularly AMD. Researchers have identified the three distinct macular pigments, MP metabolism, and specific binding proteins of MP in the retina, but there are still many questions to be answered. Carotenoid physiology, metabolism, and molecular aspects of its antioxidant property have not yet been studied in sufficient detail. There are still knowledge gaps with regard to carotenoid absorption, transport, and distribution to the target tissues. The precise function of the metabolite meso-zeaxanthin and the interaction of carotenoids with BCO1 and BCO2 are unclear. The individual variations in MP peaks in the fovea and diverse responses to identical supplement interventions have not been solved at molecular levels.
The majority of the MP investigations in AMD over the last two decades were performed without the consideration of genetic predisposition to AMD or alterations in carotenoid metabolism. While many genetic risks factors for AMD have been identified, in 2018 it is still standard-of-care to assess genetic risk by obtaining only a family history. Twenty-four single nucleotide polymorphisms (SNPs) within five genes involved in the metabolism and transport of lutein and zeaxanthin have been identified in individuals with early or intermediate AMD [85], further supporting the protective role of macular carotenoids in the prevention of AMD. A large study of twins demonstrated that there was moderate heritability in the MPOD response to lutein and zeaxanthin supplementation [86]. These genetic variations seen in patients afflicted with AMD may offer an explanation on why some epidemiologic studies did not show a protective effect with lutein and zeaxanthin intake. There is a growing body of evidence supporting the variable response to carotenoid intake in increasing MP density [86, 87]. Variations in the genes complement factor H (CFH) and LOC387715/age-related maculopathy susceptibility 2 (ARMS2) have been associated with varying response to AREDS supplementation [88]. The question begs should we test all our patients with AMD prior to making supplement recommendations? Routine genetic testing for CFH and ARMS2 mutations to guide supplementation has been highly controversial and is likely to remain so. In this genomic era, there will certainly be greater numbers of identified genetic risks factors for AMD and more feasibility in testing for them in the clinical environment. However, further research will be needed to better understand the complex relationship between genetic risks, MP density, dietary intake, serum concentrations of macular carotenoids, and other lifestyle factors.
As the lifespan of individuals worldwide increases, AMD continues to be the number one cause of blindness in the elderly and is the third most common cause of blindness (8.7%) following cataracts and glaucoma [89, 90]. In order to effectively and efficiently screen individuals most at risk for AMD, there is a crucial need for the development of diagnostic equipment that is portable, cost-effective, accurate, and quick. In the future, prospective studies could be designed to elucidate whether skin and/or macular resonance Raman spectroscopy or heterochromatic flicker photometry (HFP) are sufficient tools to accurately identify persons at risk of developing AMD associated with low MP concentrations or anomalous distributions [91, 92], thus allowing for preventative interventions prior to the onset of visual impairment. Normative databases will need to be created much like optical coherence tomography and retinal nerve fiber layer thickness to better understand an individual’s carotenoid status. It is already clear that MP concentrations are readily impacted by oral supplementation through both diet and vitamins [93]. Carotenoid benchmarks could also be defined to aid in dosing concentrations of oral supplementation and monitoring compliance. Long-term studies could then be used to define at what point in an individual’s life supplementation should be started, maybe even before the clinical development of AMD.
Dietary supplements containing macular carotenoids are given to AMD patients in the form of capsules, powders or beadlets to ameliorate AMD. In the future, these supplements may be given in the form of nanoformulations such as nanocapsules, and functional foods with lutein supplementation are expected to reach the market soon. Patients often inquire about various herbal supplements and alternative medicines to treat AMD such as anthocyanins [94], goji berries [95], and saffron [96]. However, the safety, pharmacokinetics, and efficacy of these substances are largely unknown, and the potential for adverse interactions with other medications or supplements cannot be overlooked. While it is highly unlikely for more large studies on the scale of AREDS2 to be conducted, there would be benefit to discovering some information about these alternative agents that some of our patients are consuming [63].
While meso-zeaxanthin was identified as a macular carotenoid prior to the commencement of the AREDS2 trial, it was not commercially available at that time and was not included in the formulation. Meso-zeaxanthin is now available commercially as a supplement, although many questions remain on how it should be utilized. Meso-zeaxanthin is not normally a part of the human diet and is thought to be the result of lutein metabolism [97], yet its longitudinal effect on the progression of AMD as a dietary supplement is unknown. Supplementation of meso-zeaxanthin along with lutein and zeaxanthin has shown improvements in psychophysical testing compared to placebo, but its impact on the progression of AMD is unclear [77]. Carotenoid-binding proteins have been demonstrated to deposit meso-zeaxanthin into the macula, thus supporting the hypothesis that oral supplementation of meso-zeaxanthin will augment MP density [48]. It is now available commercially, and logically, it should be included in one treatment arm of any potential AREDS3 trial, if that study were to be conducted one day.
Clinicians and researchers in the future will have the benefit of improved, standardized methods of quantifying MP density and monitoring changes longitudinally. As the research in psychophysical visual function and MP matures, this information could facilitate the evaluation of a patient’s vision in a more comprehensive manner than the Snellen chart alone. Correlating MP changes with alterations in psychophysical testing may allow for optimization of dietary supplementation such as the lutein and zeaxanthin ratio or addition of meso-zeaxanthin to AREDS2 [98]. These novel techniques in conjunction with the better interpretation of the data will permit a more complete understanding and management of age-related macular degeneration.
References
Woodall AA, Britton G, Jackson MJ. Carotenoids and protection of phospholipids in solution or in liposomes against oxidation by peroxyl radicals: relationship between carotenoid structure and protective ability. Biochim Biophys Acta BBA-Gen Subj. 1997;1336:575–86.
Stahl W. Macular carotenoids: lutein and zeaxanthin. In: Nutrition and the Eye. Karger Publishers. 2005:70–88. https://doi.org/10.1159/000082768.
Bone RA, Landrum JT, Hime GW, Cains A, Zamor J. Stereochemistry of the human macular carotenoids. Invest Ophthalmol Vis Sci. 1993;34:2033–40.
Khachik F, Bernstein PS, Garland DL. Identification of lutein and zeaxanthin oxidation products in human and monkey retinas. Invest Ophthalmol Vis Sci. 1997;38:1802–11.
Bone RA, Landrum JT, Fernandez L, Tarsis SL. Analysis of the macular pigment by HPLC: retinal distribution and age study. Invest Ophthalmol Vis Sci. 1988;29:843–9.
Sujak A, Gabrielska J, Grudziński W, Borc R, Mazurek P, Gruszecki WI. Lutein and zeaxanthin as protectors of lipid membranes against oxidative damage: the structural aspects. Arch Biochem Biophys. 1999;371:301–7.
Landrum JT, Bone RA, Krinsky NI, Mayne ST, Sies H. Mechanistic evidence for eye diseases and carotenoids. Oxid STRESS Dis. 2004;13:445–72.
Barker FM, Neuringer M, Johnson EJ, Schalch W, Koepcke W, Snodderly DM. Dietary zeaxanthin or lutein improves foveal photo–protection from blue light in xanthopyhll–free monkeys. Invest Ophthalmol Vis Sci. 2005;46:1770–1770.
Chucair AJ, Rotstein NP, SanGiovanni JP, During A, Chew EY, Politi LE. Lutein and zeaxanthin protect photoreceptors from apoptosis induced by oxidative stress: relation with docosahexaenoic acid. Invest Ophthalmol Vis Sci. 2007;48:5168–77.
Wu J, Cho E, Willett WC, Sastry SM, Schaumberg DA. Intakes of lutein, zeaxanthin, and other carotenoids and age-related macular degeneration during 2 decades of prospective follow-up. JAMA Ophthalmol. 2015;133:1415–24.
Mares-Perlman JA, Fisher AI, Klein R, Palta M, Block G, Millen AE, et al. Lutein and zeaxanthin in the diet and serum and their relation to age-related maculopathy in the third national health and nutrition examination survey. Am J Epidemiol. 2001;153:424–32.
Seddon JM, Ajani UA, Sperduto RD, Hiller R, Blair N, Burton TC, et al. Dietary carotenoids, vitamins A, C, and E, and advanced age-related macular degeneration. Eye Disease Case-Control Study Group. JAMA . 1994;272:1413–20.
Sommerburg O, Keunen JE, Bird AC, van Kuijk FJ. Fruits and vegetables that are sources for lutein and zeaxanthin: the macular pigment in human eyes. Br J Ophthalmol. 1998;82:907–10.
Maiani G, Periago Castón MJ, Catasta G, Toti E, Cambrodón IG, Bysted A, et al. Carotenoids: actual knowledge on food sources, intakes, stability and bioavailability and their protective role in humans. Mol Nutr Food Res. 2009;53(S2):S194–218.
Perry A, Rasmussen H, Johnson EJ. Xanthophyll (lutein, zeaxanthin) content in fruits, vegetables and corn and egg products. J Food Compos Anal. 2009;22:9–15.
Abdel-Aal E-SM, Akhtar H, Zaheer K, Ali R. Dietary sources of lutein and zeaxanthin carotenoids and their role in eye health. Nutrients . 2013;5:1169–85.
Maoka T, Arai A, Shimizu M, Matsuno T. The first isolation of enantiomeric and meso-zeaxanthin in nature. Comp Biochem Physiol Part B Comp Biochem. 1986;83:121–4.
Bhosale P, Serban B, Zhao DY, Bernstein PS. Identification and metabolic transformations of carotenoids in ocular tissues of the Japanese quail Coturnix japonica. Biochem (Mosc). 2007;46:9050–7.
Khachik F, De Moura FF, Zhao D-Y, Aebischer C-P, Bernstein PS. Transformations of selected carotenoids in plasma, liver, and ocular tissues of humans and in nonprimate animal models. Invest Ophthalmol Vis Sci. 2002;43:3383–92.
Ravikrishnan R, Rusia S, Ilamurugan G, Salunkhe U, Deshpande J, Shankaranarayanan J, et al. Safety assessment of lutein and zeaxanthin (Lutemax 2020): subchronic toxicity and mutagenicity studies. Food Chem Toxicol Int J Publ Br Ind Biol Res Assoc. 2011;49:2841–8.
Thurnham DI, Howard AN. Studies on meso-zeaxanthin for potential toxicity and mutagenicity. Food Chem Toxicol. 2013;59:455–63.
Buzzi F Nuove sperienze fatte sull’occhio umano. 1782.
Soemmering S. De foramina centrali limbo luteo cincto retinae humanae. Comment Soc Reg Sci Goetting. 1799;13:3.
Soemmering P, Home E. An account of the orifice in the retina of the human eye, discovered by professor soemmering. to which are added, proofs of this appearance being extended to the eyes of other animals. Everard Home, Esq Frs Philos Trans R Soc Lond. 1798;88:332–45.
Schultze M. Zur anatomie und physiologie der retina. Arch Für Mikrosk Anat. 1866;2:175–286.
Wald G. Human vision and the spectrum. Science . 1945;101:653–8.
Bone RA, Landrum JT, Tarsis SL. Preliminary identification of the human macular pigment. Vision Res. 1985;25:1531–5.
Handelman GJ, Dratz EA, Reay CC, Kuijk JGvan. Carotenoids in the human macula and whole retina. Invest Ophthalmol Vis Sci. 1988;29:850–5.
Snodderly DM, Brown PK, Delori FC, Auran JD. The macular pigment. I. Absorbance spectra, localization, and discrimination from other yellow pigments in primate retinas. Invest Ophthalmol Vis Sci. 1984;25:660–73.
Bernstein PS, Khachik F, Carvalho LS, Muir GJ, Zhao D-Y, Katz NB. Identification and Quantitation of Carotenoids and their Metabolites in the Tissues of the Human Eye. Exp Eye Res. 2001;72:215–23.
Johnson EJ, Neuringer M, Russell RM, Schalch W, Snodderly DM. Nutritional manipulation of primate retinas, III: Effects of lutein or zeaxanthin supplementation on adipose tissue and retina of xanthophyll-free monkeys. Invest Ophthalmol Vis Sci. 2005;46:692–702.
Shyam R, Gorusupudi A, Nelson K, Horvath MP, Bernstein PS. RPE65 has an additional function as the lutein to meso-zeaxanthin isomerase in the vertebrate eye. Proc Natl Acad Sci USA. 2017;114:10882–7.
Yonekura L, Nagao A. Intestinal absorption of dietary carotenoids. Mol Nutr Food Res. 2007;51:107–15.
Li B, Vachali PP, Gorusupudi A, Shen Z, Sharifzadeh H, Besch BM, et al. Inactivity of human β,β-carotene-9’,10’-dioxygenase (BCO2) underlies retinal accumulation of the human macular carotenoid pigment. Proc Natl Acad Sci USA. 2014;111:10173–8.
Zaripheh S, Erdman JW. Factors that influence the bioavailablity of xanthophylls. J Nutr. 2002;132:531S–534S.
West CE, Castenmiller JJ. Quantification of the “SLAMENGHI” factors for carotenoid bioavailability and bioconversion. Int J Vitam Nutr Res. 1998;68:371–7.
Faulks RM, Southon S. Challenges to understanding and measuring carotenoid bioavailability. Biochim Biophys Acta. 2005;1740:95–100.
Mamatha BS, Baskaran V. Effect of micellar lipids, dietary fiber and β-carotene on lutein bioavailability in aged rats with lutein deficiency. Nutrition. 2011;27:960–6.
DiSilvestro RA, Thomas S, Harrison E, Epitropoulos A. A pilot comparison of phospolipidated lutein to conventional lutein for effects on plasma lutein concentrations in adult people. Nutr J. 2015;14:104.
Molldrem KL, Li J, Simon PW, Tanumihardjo SA. Lutein and β-carotene from lutein-containing yellow carrots are bioavailable in humans. Am J Clin Nutr. 2004;80:131–6.
Kostic D, White WS, Olson JA. Intestinal absorption, serum clearance, and interactions between lutein and beta-carotene when administered to human adults in separate or combined oral doses. Am J Clin Nutr. 1995;62:604–10.
High EG, Day HG. Effects of different amounts of lutein, squalene, phytol and related substances on the utilization of carotene and vitamin A for storage and growth in the rat. J Nutr. 1951;43:245–60.
Gorusupudi A, Baskaran V. Wheat germ oil: A potential facilitator to improve lutein bioavailability in mice. Nutrition . 2013;29:790–5.
Li B, Vachali PP, Shen Z, Gorusupudi A, Nelson K, Besch BM, et al. Retinal accumulation of zeaxanthin, lutein, and β-carotene in mice deficient in carotenoid cleavage enzymes. Exp Eye Res. 2017;159:123–31.
Li B, Vachali P, Bernstein SP. Human ocular carotenoid -binding proteins. Photochem Photobiol Sci. 2010;9:1418–25.
Reboul E, Abou L, Mikail C, Ghiringhelli O, André M, Portugal H, et al. Lutein transport by Caco-2 TC-7 cells occurs partly by a facilitated process involving the scavenger receptor class B type I (SR-BI). Biochem J. 2005;387(Pt 2):455–61.
Lobo GP, Hessel S, Eichinger A, Noy N, Moise AR, Wyss A, et al. ISX is a retinoic acid-sensitive gatekeeper that controls intestinal beta,beta-carotene absorption and vitamin A production. FASEB J Publ Fed Am Soc Exp Biol. 2010;24:1656–66.
Shyam R, Vachali P, Gorusupudi A, Nelson K, Bernstein PS. All three human scavenger receptor class B proteins can bind and transport all three macular xanthophyll carotenoids. Arch Biochem Biophys. 2017;634:21–28.
During A, Dawson HD, Harrison EH. Carotenoid transport is decreased and expression of the lipid transporters SR-BI, NPC1L1, and ABCA1 is downregulated in Caco-2 cells treated with ezetimibe. J Nutr. 2005;135:2305–12.
Bernstein PS, Balashov NA, Tsong ED, Rando RR. Retinal tubulin binds macular carotenoids. Invest Ophthalmol Vis Sci. 1997;38:167–75.
Bhosale P, Larson AJ, Frederick JM, Southwick K, Thulin CD, Bernstein PS. Identification and Characterization of a Pi Isoform of Glutathione S-Transferase (GSTP1) as a Zeaxanthin-binding Protein in the Macula of the Human Eye. J Biol Chem. 2004;279:49447–54.
Li B, Vachali P, Frederick JM, Bernstein PS. Identification of StARD3 as a lutein-binding protein in the macula of the primate retina. Biochem (Mosc). 2011;50:2541–9.
Vachali P, Besch BM, Gonzalez-Fernandez F, Bernstein PS. Carotenoids as Possible Interphotoreceptor Retinoid-binding Protein (IRBP) Ligands: A Surface Plasmon Resonance (SPR) Based Study. Arch Biochem Biophys [Internet]. 2013;539:181–6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3818380/ [accessed on 15 Januray 2018]
Thomas SE, Harrison EH. Mechanisms of selective delivery of xanthophylls to retinal pigment epithelial cells by human lipoproteins. J Lipid Res. 2016;57:1865–78.
Connor WE, Duell PB, Kean R, Wang Y. The prime role of HDL to transport lutein into the retina: evidence from HDL-deficient WHAM chicks having a mutant ABCA1 transporter. Invest Ophthalmol Vis Sci. 2007;48:4226–31.
Borel P, de Edelenyi FS, Vincent-Baudry S, Malezet-Desmoulin C, Margotat A, Lyan B, et al. Genetic variants in BCMO1 and CD36 are associated with plasma lutein concentrations and macular pigment optical density in humans. Ann Med. 2011;43:47–59.
Wong TY, Loon S-C, Saw S-M. The epidemiology of age related eye diseases in Asia. Br J Ophthalmol. 2006;90:506–11.
Congdon N, O’Colmain B, Klaver CC, Klein R, Muñoz B, Friedman DS, et al. Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol Chic Ill 1960. 2004;122:477–85.
Hageman GS, Anderson DH, Johnson LV, Hancox LS, Taiber AJ, Hardisty LI, et al. A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration. Proc Natl Acad Sci USA. 2005;102:7227–32.
Yang Z, Camp NJ, Sun H, Tong Z, Gibbs D, Cameron DJ, et al. A variant of the HTRA1 gene increases susceptibility to age-related macular degeneration. Science . 2006;314:992–3.
Bernstein PS, Li B, Vachali PP, Gorusupudi A, Shyam R, Henriksen BS, et al. Lutein, zeaxanthin, and meso-zeaxanthin: The basic and clinical science underlying carotenoid-based nutritional interventions against ocular disease. Prog Retin Eye Res. 2016;50:34–66.
Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol Chic Ill 1960. 2001;119:1417–36.
Gorusupudi A, Nelson K, Bernstein PS. The age-related eye disease 2 study: micronutrients in the treatment of macular degeneration. Adv Nutr Bethesda Md. 2017;8:40–53.
Albanes D, Heinonen OP, Taylor PR, Virtamo J, Edwards BK, Rautalahti M, et al. Alpha-Tocopherol and beta-carotene supplements and lung cancer incidence in the alpha-tocopherol, beta-carotene cancer prevention study: effects of base-line characteristics and study compliance. J Natl Cancer Inst. 1996;88:1560–70.
Alpha-Tocopherol, Beta Carotene Cancer Prevention Study Group. The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers. N Engl J Med. 1994;330:1029–35.
Hambidge M. Underwood Memorial Lecture: human zinc homeostasis: good but not perfect. J Nutr. 2003;133(5Suppl 1):1438S–42S.
Johnson AR, Munoz A, Gottlieb JL, Jarrard DF. High dose zinc increases hospital admissions due to genitourinary complications. J Urol. 2007;177:639–43.
Age-Related Eye Disease Study 2 (AREDS2) Research Group, Chew EY, Clemons TE, Sangiovanni JP, Danis RP, Ferris FL, et al. Secondary analyses of the effects of lutein/zeaxanthin on age-related macular degeneration progression: AREDS2 report No. 3. JAMA Ophthalmol. 2014;132:142–9.
Souied EH, Delcourt C, Querques G, Bassols A, Merle B, Zourdani A, et al. Oral docosahexaenoic acid in the prevention of exudative age-related macular degeneration: the Nutritional AMD Treatment 2 study. Ophthalmology . 2013;120:1619–31.
Bernstein PS, Ahmed F, Liu A, Allman S, Sheng X, Sharifzadeh M, et al. Macular pigment imaging in AREDS2 participants: an ancillary study of AREDS2 subjects enrolled at the Moran Eye Center. Invest Ophthalmol Vis Sci. 2012;53:6178–86.
Conrady CD, Bell JP, Besch BM, Gorusupudi A, Farnsworth K, Ermakov I, et al. Correlations between macular, skin, and serum carotenoids. Invest Ophthalmol Vis Sci. 2017;58:3616–27.
Sabour-Pickett S, Beatty S, Connolly E, Loughman J, Stack J, Howard A, et al. Supplementation with three different macular carotenoid formulations in patients with early age-related macular degeneration. Retin Phila Pa. 2014;34:1757–66.
Snodderly DM, Mares JA, Wooten BR, Oxton L, Gruber M, Ficek T, et al. Macular pigment measurement by heterochromatic flicker photometry in older subjects: the carotenoids and age-related eye disease study. Invest Ophthalmol Vis Sci. 2004;45:531–8.
McCorkle SM, Raine LB, Hammond BR, Renzi-Hammond L, Hillman CH, Khan NA. Reliability of heterochromatic flicker photometry in measuring macular pigment optical density among preadolescent children. Foods Basel Switz. 2015;4:594–604.
Dennison JL, Stack J, Beatty S, Nolan JM. Concordance of macular pigment measurements obtained using customized heterochromatic flicker photometry, dual-wavelength autofluorescence, and single-wavelength reflectance. Exp Eye Res. 2013;116:190–8.
Komar B, Rauscher FG, Wiedemann R, Dawczynski J. Macular pigment optical density measurements by one-wavelength reflection photometry--influence of cataract surgery on the measurement results. Graefes Arch Clin Exp Ophthalmol Albrecht Von Graefes Arch Klin Exp Ophthalmol. 2014;252:1717–27.
Nolan JM, Power R, Stringham J, Dennison J, Stack J, Kelly D, et al. Enrichment of macular pigment enhances contrast sensitivity in subjects free of retinal disease: Central Retinal Enrichment Supplementation Trials - Report 1. Invest Ophthalmol Vis Sci. 2016;57:3429–39.
Choi RY, Chortkoff SC, Gorusupudi A, Bernstein PS. Crystalline maculopathy associated with high-dose lutein supplementation. JAMA Ophthalmol. 2016;134:1445–8.
Akuffo KO, Nolan JM, Peto T, Stack J, Leung I, Corcoran L, et al. Relationship between macular pigment and visual function in subjects with early age-related macular degeneration. Br J Ophthalmol. 2017;101:190–7.
Stringham JM, Stringham NT, O’Brien KJ. Macular carotenoid supplementation improves visual performance, sleep quality, and adverse physical symptoms in those with high screen time exposure. Foods Basel Switz. 2017;6:47–60.
Wenzel AJ, Fuld K, Stringham JM, Curran-Celentano J. Macular pigment optical density and photophobia light threshold. Vision Res. 2006;46:4615–22.
Akuffo KO, Beatty S, Peto T, Stack J, Stringham J, Kelly D, et al. The impact of supplemental antioxidants on visual function in nonadvanced age-related macular degeneration: a Head-to-Head Randomized Clinical Trial. Invest Ophthalmol Vis Sci. 2017;58:5347–60.
Wood JM, Owens DA. Standard measures of visual acuity do not predict drivers’ recognition performance under day or night conditions. Optom Vis Sci Publ Am Acad Optom. 2005;82:698–705.
Owsley C, Sloane ME. Contrast sensitivity, acuity, and the perception of “real-world” targets. Br J Ophthalmol. 1987;71:791–6.
Meyers KJ, Mares JA, Igo RP, Truitt B, Liu Z, Millen AE, et al. Genetic evidence for role of carotenoids in age-related macular degeneration in the Carotenoids in Age-Related Eye Disease Study (CAREDS). Invest Ophthalmol Vis Sci. 2014;55:587–99.
Hammond CJ, Liew SHM, Van Kuijk FJ, Beatty S, Nolan JM, Spector TD, et al. The heritability of macular response to supplemental lutein and zeaxanthin: a classic twin study. Invest Ophthalmol Vis Sci. 2012;53:4963–8.
Mares JA, LaRowe TL, Snodderly DM, Moeller SM, Gruber MJ, Klein ML, et al. Predictors of optical density of lutein and zeaxanthin in retinas of older women in the Carotenoids in Age-Related Eye Disease Study, an ancillary study of the Women’s Health Initiative. Am J Clin Nutr. 2006;84:1107–22.
Klein ML, Francis PJ, Rosner B, Reynolds R, Hamon SC, Schultz DW, et al. CFH and LOC387715/ARMS2 genotypes and treatment with antioxidants and zinc for age-related macular degeneration. Ophthalmology . 2008;115:1019–25.
Gehrs KM, Anderson DH, Johnson LV, Hageman GS. Age-related macular degeneration--emerging pathogenetic and therapeutic concepts. Ann Med. 2006;38:450–71.
World Health Organization—Global data on visual impairments 2010. Available at http://www.who.int/blindness/GLOBALDATAFINALforweb.pdf?ua=1.
Mayne ST, Cartmel B, Scarmo S, Jahns L, Ermakov IV, Gellermann W. Resonance Raman spectroscopic evaluation of skin carotenoids as a biomarker of carotenoid status for human studies. Arch Biochem Biophys. 2013;539:163–70.
Bernstein PS, Zhao D-Y, Wintch SW, Ermakov IV, McClane RW, Gellermann W. Resonance Raman measurement of macular carotenoids in normal subjects and in age-related macular degeneration patients. Ophthalmology . 2002;109:1780–7.
Obana A, Tanito M, Gohto Y, Okazaki S, Gellermann W, Bernstein PS. Changes in macular pigment optical density and serum lutein concentration in Japanese subjects taking two different lutein supplements. PLoS One. 2015;10:e0139257.
Liu Y, Song X, Zhang D, Zhou F, Wang D, Wei Y, et al. Blueberry anthocyanins: protection against ageing and light-induced damage in retinal pigment epithelial cells. Br J Nutr. 2012;108:16–27.
Cheng CY, Chung WY, Szeto YT, Benzie IFF. Fasting plasma zeaxanthin response to Fructus barbarum L. (wolfberry; Kei Tze) in a food-based human supplementation trial. Br J Nutr. 2005;93:123–30.
Piccardi M, Marangoni D, Minnella AM, Savastano MC, Valentini P, Ambrosio L, et al. A longitudinal follow-up study of saffron supplementation in early age-related macular degeneration: sustained benefits to central retinal function. Evid-Based Complement Altern Med ECAM. 2012;2012:429124.
Nolan JM, Meagher K, Kashani S, Beatty S. What is meso-zeaxanthin, and where does it come from? Eye (Lond). 2013;27:899–905.
Bernstein PS, Delori FC, Richer S, van Kuijk FJM, Wenzel AJ. The value of measurement of macular carotenoid pigment optical densities and distributions in age-related macular degeneration and other retinal disorders. Vision Res. 2010;50:716–28.
Acknowledgements
This work was supported in part by NIH grants EY11600 and EY14800 and by an unrestricted departmental grant from Research to Prevent Blindness.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
P.S.B. and the University of Utah hold a patent on the use of resonance Raman spectroscopy to measure carotenoid levels in the eye, skin, and other tissues. The remaining authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Arunkumar, R., Calvo, C.M., Conrady, C.D. et al. What do we know about the macular pigment in AMD: the past, the present, and the future. Eye 32, 992–1004 (2018). https://doi.org/10.1038/s41433-018-0044-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-018-0044-0
This article is cited by
-
Generation and physiological characterization of genome-edited Nicotiana benthamiana plants containing zeaxanthin as the only leaf xanthophyll
Planta (2023)
-
Distribution of macular pigments in macular telangiectasia type 2 and correlation with optical coherence tomography characteristics and visual acuity
BMC Ophthalmology (2022)
-
The Lutein and Zeaxanthin in Pregnancy (L-ZIP) study—carotenoid supplementation during pregnancy: ocular and systemic effects—study protocol for a randomized controlled trial
Trials (2021)
-
Stability and ocular biodistribution of topically administered PLGA nanoparticles
Scientific Reports (2021)
-
Macular pigment optical density change analysis in primary open-angle glaucoma and pseudoexfoliation glaucoma
International Ophthalmology (2021)