Abstract
Background Plaque biofilm that adheres to tooth surfaces and gingiva is the main aetiology of periodontitis. Chlorhexidine (CHX) is considered as a gold standard anti-plaque and anti-gingivitis agent but it has side effects such as permanent staining of teeth and dysgeusia. Tea tree oil (TTO) is an essential oil extracted from the leaves of Melaleuca alternifolia. Many studies have reported that TTO exerts strong antibacterial, antifungal, antiviral and anti-inflammatory activities.
Primary study objective The review aims to answer the question of whether TTO (intervention) is a viable alternative to CHX (comparator) for the management of gingival and periodontal disease (outcomes) in adolescents and adults (population).
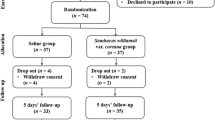
Methods/design The following search terms were used in PubMed, Scopus, Proquest, Web of Science, EBSCO (dentistry and open access), Cochrane database, Clinical.gov.org and ctri.nic.in to search for relevant articles: patients with periodontal disease; OR periodontitis; OR gingivitis; OR gingival inflammation; AND essential oil; OR tea tree oil; OR Melaleuca alternifolia; AND chlorhexidine; AND reduction in gingival index; OR reduction in plaque index; OR reduction in bleeding from gums. The initial check for the title and abstract screening followed by removal of duplicates in Mendeley Reference Manager (version 1.19.4) based on the inclusion and exclusion criteria were performed.
Primary outcome measures Parameters such as plaque index (PI), plaque surface score, gingival index (GI), bleeding index or bleeding as measured by % of sites with bleeding on probing (BOP) or bleeding scores, papillary bleeding index (PBI), were the primary outcomes considered.
Results TTO is found to be superior to CHX in reducing signs of gingival inflammation; however, CHX is superior to TTO in inhibiting plaque formation, probably due to its increased substantivity.
Conclusion TTO may be used as an alternative to CHX for reduction of gingival inflammation in conjunction with efficient plaque control measures.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Batchelor P. Is periodontal disease a public health problem? Br Dent J 2014; 217: 405-409.
Tonetti M S, Jepsen S, Jin L, Otomo-Corgel J. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. J Clin Periodontol 2017; 44: 456-462.
Könönen E, Gursoy M, Gursoy U K. Periodontitis: A Multifaceted Disease of Tooth-Supporting Tissues. J Clin Med 2019; 8: 1135.
Janakiram C, Basapathy R, Taha F, Venkitachalam R, Akalgud H, Kadanakuppe S. Equity in Oral Healthcare in India: A Review on Health System Analysis. Econ Polit Wkly 2017; 52: 82.
Andriankaja O, Trevisan M, Falkner K et al. Association between periodontal pathogens and risk of nonfatal myocardial infarction. Community Dent Oral Epidemiol 2011; 39: 177-185.
Nobre M D A, Maló P. Prevalence of periodontitis, dental caries, and peri-implant pathology and their relation with systemic status and smoking habits: Results of an open-cohort study with 22009 patients in a private rehabilitation centre. J Dent 2017; 67: 36-42.
Chandki R, Banthia P, Banthia R. Biofilms: A microbial home. J Indian Soc Periodontol 2011; 15: 111-114.
Torrungruang K, Jitpakdeebordin S, Charatkulangkun O, Gleebbua Y. Porphyromonas gingivalis, aggregatibacter actinomycetemcomitans, and Treponema denticola/Prevotella intermedia Co-Infection Are Associated with Severe Periodontitis in a Thai Population. PLoS One 2015; DOI: 10.1371/journal.pone.0136646.
Cekici A, Kantarci A, Hasturk H, Van Dyke T E. Inflammatory and immune pathways in the pathogenesis of periodontal disease. Periodontol 2000 2014; 64: 57-80.
Figuero E, Nóbrega D F, García-Gargallo M, Tenuta L M A, Herrera D, Carvalho J C. Mechanical and chemical plaque control in the simultaneous management of gingivitis and caries: a systematic review. J Clin Periodontol 2017; DOI: 10.1111/jcpe.12674.
Balagopal S, Arjunkumar R. Chlorhexidine: The Gold Standard Antiplaque Agent. J Pharm Sci Res 2013; 5: 270-274.
Palombo E A. Traditional Medicinal Plant Extracts and Natural Products with Activity against Oral Bacteria: Potential Application in the Prevention and Treatment of Oral Diseases. Evid Based Complement Altern Med 2011; DOI: 10.1093/ecam/nep067.
Eid Abdelmagyd H A, Ram Shetty D S, Musa Musleh Al-Ahmari D M. Herbal medicine as adjunct in periodontal therapies - A review of clinical trials in past decade. J Oral Biol Craniofacial Res 2019; 9: 212-217.
Soulissa A, Afifah J, Herryawan, Widyarman A. The effect of tea tree oil in inhibiting the adhesion of pathogenic periodontal biofilms in vitro. Sci Dent J 2020; 4: 88-92.
Elgendy E A, Abdel-Moula Ali S, Zineldeen D H. Effect of local application of tea tree (Melaleuca alternifolia) oil gel on long pentraxin level used as an adjunctive treatment of chronic periodontitis: A randomized controlled clinical study. J Indian Soc Periodontol 2013; 17: 444-448.
Armitage G C. Development of a classification system for periodontal diseases and conditions. Ann Periodontol 1999; 4: 1-6.
Löe H. The Gingival Index, the Plaque Index and the Retention Index Systems. J Periodontol 1967; 38: 610-616.
Engelberger T, Hefti A, Kallenberger A, Rateitschak K-H. Correlations among Papilla Bleeding Index, other clinical indices and historically determined inflammation of gingival papilla. J Clin Periodontol 1983; 10: 579-589.
Sterne J A, Hernán M A, Reeves B C et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016; DOI: 10.1136/bmj.i4919.
Viswanathan M, Patnode C D, Berkman N D et al. Recommendations for assessing the risk of bias in systematic reviews of health-care interventions. J Clin Epidemiol 2018; 97: 26-34.
Alshehri M, Alshail F, Aldosary K M, Alamri A A. Comparison of an essential -oil -based oral rinse and chlorhexidine as adjuncts to scaling and root planing in the treatment of periodontal inflammation. Interv Med Appl Sci 2015; 7: 78-84.
Charugundla B R, Anjum S, Mocherla M. Comparative effect of fluoride, essential oil and chlorhexidine mouth rinses on dental plaque and gingivitis in patients with and without dental caries: a randomized controlled trial. Int J Dent Hyg 2015; 13: 104-109.
Cortelli S C, Cortelli J R, Holzhausen M et al. Essential oils in one-stage full-mouth disinfection: double-blind, randomized clinical trial of long-term clinical, microbial and salivary effects. J Clin Periodontol 2009; 36: 333-342.
Kulkarni P, Singh D K, Jalaluddin M, Mandal A. Comparative Evaluation of Antiplaque Efficacy between Essential Oils with Alcohol-Based and Chlorhexidine with Nonalcohol-Based Mouthrinses. J Int Soc Prev Community Dent 2017; DOI: 10.4103/jispcd.JISPCD_131_17.
Tumer H, Berberoglu A, Caygur A, Yilmaz H G. Clinical Evaluation of Chlorhexidine and Essential Oils' Adjunctive Effects in Subgingival Ultrasonic Instrumentation on Periodontal Parameters and Halitosis. J Essent Oil-Bearing Plant 2019; 22: 169-175.
Yilmaz H G, Bayindir H. Clinical evaluation of chlorhexidine and essential oils for adjunctive effects in ultrasonic instrumentation of furcation involvements: a randomized controlled clinical trial. Int J Dent Hyg 2012; 10: 113-117.
Siddabasappa K G, Vandana L. Effect of Tea Tree Oil in Chronic Periodontitis Patients: A Clinical and Microbiological Study. CODS J Dent 2019; 11: 26-31.
Shetty S K, Sharath K, Shenoy S, Sreekumar C, Shetty R N, Biju T. Compare the efficacy of two commercially available mouthrinses in reducing viable bacterial count in dental aerosol produced during ultrasonic scaling when used as a preprocedural rinse. J Contemp Dent Pract 2013; 14: 848-851.
Elmehy G, Abo-Shady T. Comparison Between Tea Tree Oil and Chlorhexidine Mouth Rinse in Treatment of Gingivitis Induced by Orthodontic Treatment: A Randomized Control Clinical Study. Egypt Dent J 2018; 64: 249-256.
Ripari F, Cera A, Freda M, Zumbo G, Zara F, Vozza I. Tea Tree Oil versus Chlorhexidine Mouthwash in Treatment of Gingivitis: A Pilot Randomized, Double Blinded Clinical Trial. Eur J Dent 2020; 14: 55-62.
Soukoulis S, Hirsch R. The effects of a tea tree oil-containing gel on plaque and chronic gingivitis. Aust Dent J 2004; 49: 78-83.
Reddy V, Bennadi D, Satish G, Divya, Guruprasad, Reddy C V K. Effectiveness of tea tree oil and chlorhexidine as mouth rinse in the control of dental plaque and chronic gingivitis - A comparative study. Eur J Mol Clin Med 2020; 7: 1576-1582.
Brand C, Ferrante A, Prager R H et al. The water-soluble components of the essential oil of Melaleuca alternifolia (tea tree oil) suppress the production of superoxide by human monocytes, but not neutrophils, activated in vitro. Inflamm Res 2001; 50: 213-219.
Carson C F, Hammer K A, Riley T V. Melaleuca alternifolia (Tea Tree) oil: a review of antimicrobial and other medicinal properties. Clin Microbiol Rev 2006; 19: 50-62.
Supranoto S C, Slot D E, Addy M, Van der Weijden G A. The effect of chlorhexidine dentifrice or gel versus chlorhexidine mouthwash on plaque, gingivitis, bleeding and tooth discoloration: a systematic review. Int J Dent Hyg 2015; 13: 83-92.
Taalab M R, Mahmoud S A, Moslemany R M El, Abdelaziz D M. Intrapocket application of tea tree oil gel in the treatment of stage 2 periodontitis. BMC Oral Health 2021; DOI: 10.1186/s12903-021-01588-y.
Rahman B, Alkawas S, Al Zubaidi E A, Adel O I, Hawas N. Comparative antiplaque and antigingivitis effectiveness of tea tree oil mouthwash and a cetylpyridinium chloride mouthwash: A randomized controlled crossover study. Contemp Clin Dent 2014; 5: 466-470.
Author information
Authors and Affiliations
Contributions
Niharika Singh contributed to conception and design of the work, data collection, drafting the article, critical revision of the article and gave final approval of the version to be published. Lakshmi Puzhankara contributed to conception and design of the work, data collection, data analysis and interpretation, drafting the article, critical revision of the article and gave final approval of the version to be published. Madhurya N. Kedlaya contributed to drafting the article, designing images in the article, critical revision of the article and gave final approval of the version to be published. Venkitachalam Ramanarayanan contributed to data analysis and interpretation, drafting the article, critical revision of the article and gave final approval of the version to be published.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Singh, N., Puzhankara, L., Kedlaya, M. et al. Effectiveness of tea tree oil versus chlorhexidine in the treatment of periodontal diseases: a systematic review. Evid Based Dent (2022). https://doi.org/10.1038/s41432-022-0259-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41432-022-0259-6