Abstract
Data sources Forty-four adult patients (32 female : 12 males) with irreversible pulpitis with periapical periodontitis on a mandibular posterior tooth, who were undergoing a two-visit endodontic treatment protocol, were randomly divided into two groups. The intervention group (n = 22) had occlusal surface reduced on the treated tooth and a control group (n = 22) did not.
Data The primary outcome was pain intensity after endodontic treament, which was measured on a visual-analogue-scale (VAS). This was measured 6, 12, 24 and 48 hours after the first visit, and 6, then 12 hours after the second visit.
The study also investigated the proportion of patients who took post-operative analgesic tablets.
Results Pain intensity 12 hours after the first and second visits were statistically significantly lower in the intervention group compared to the control group. The proportion of patients who recorded taking analgesics was not significantly different between the two groups.
Conclusions Occlusal reduction seems to reduce levels of post root- treatment pain in posterior mandibular teeth 12 hours postopertively, but otherwise makes little difference.
Similar content being viewed by others
A commentary on
Emara R S, Abou El Nasr H M, El Boghdadi R M.
Evaluation of postoperative pain intensity following occlusal reduction in teeth associated with symptomatic irreversible pulpitis and symptomatic apical periodontitis: a randomized clinical study. Int Endod J 2019; 52: 288-296. DOI: 10.1111/iej.13012.G

GRADE rating
Commentary
An all too common sequelae of nonsurgical endodontic treatment is self-limiting post-op pain that can linger for about a week1,2 The literature describes many ways of managing this pain.3,4,5,6,7,8,9 One technique which can be used, which goes back to the early days of endodontic care, is taking the treated tooth completely out of occlusion post-operatively.10 This study by Emara et al. supports this practice for lower molar teeth presenting with symptomatic apical periodontitis.
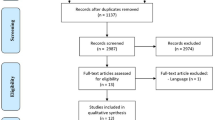
It would be premature to consider the results of any single clinical study as being conclusive without verifying it with other sources of evidence; in particular, by critically appraising the evidence relative to the current body of knowledge which addresses the same clinical question. A quick search of PubMed, Google Scholar and EMBASE identified eight other such studies dating back to 1984.11,12,13,14,15,16,17,18 The majority of them found no difference in patient-reported, post-treatment pain between those who had the endodontically treated tooth taken out of occlusion or not.11,12,14,16,17,18
The fundamental problem with synthesising any body of knowledge is how to account for the heterogeneity between the included studies. This body of knowledge is not short of significant inter-study variability: in the diagnostic definition, treatment protocol, outcome measure and sample size to name some of the sources of heterogeneity. For example, in some studies calcium hydroxide dressing was used as an inter-operative medicament before canal obturation was finalised while in others the canafs were left empty. Also, this study by Emara et al. measured post-op pain perception on a 10 mm visual analogue scale (VAS). Most of the other studies used broad categories (for example, none, mild, moderate, severe pain) to report patient experience. Data from continuous scales are more likely to find a statistical difference between groups than data from a broad categorical scale,but how clinically significant those differences are, remain open to question.
The first studies on this topic were published in 1984 and found no differences when teeth were, or were not, taken out of occlusion.11,12 However, Rosenberg et al. (1998) performed a quasi-subgroup analysis, suggesting that teeth presenting with symptomatic apical periodontitis are more likely to benefit from occlusal reduction than those that are asymptomatic.13 Except for two studies, including this one, most subsequent studies have not confirmed this hypothesis.
However, this study by Emara et al. only found a significant, but small difference in patient reported pain levels between the experimental group and the control group after 12 hours. At all other time intervals, no statistical differences were found, which suggested that this study is largely consistent with the majority of studies which found occlusal reduction did not make a difference to patients' reported post-op pain experience.
Evidence-based decision making involves the systematic approach of translating scientific knowledge to individual patient care. The GRADE (Grading of Recommendations, Assessment, Development and Evaluations) approach offers such a process of making clinical recommendation as being either strong or limited by assessing the quality of evidence on five domains - risk of bias, imprecision, inconsistency, indirectness, and publication bias.19
Although eight of the nine studies were RCTs, it can be concluded that the quality of evidence is low because of moderate to high bias in each study, imprecision of the reported outcome and inconsistency between studies. Occlusal reduction on all endodontically treated teeth to prevent post-op pain cannot be recommended yet. However, in those cases where a crown is indicated and the patient is willing to follow through with such treatment afterwards occlusal reduction should be performed.
References
Pak J G, White S N. Pain prevalence and severity before, during, and after root canal treatment: a systematic review J Endod 2011; 37: 429-438.
Sipavičiūtė E, Manelienė R. Pain and flare-up after endodontic treatment procedures Stomatologija 2014; 16: 25-30.
Iranmanesh F, Parirokh M, Haghdoost A A, Abbott P V. Effect of corticosteroids on pain relief following root canal treatment: a systematic review. Iran Endod J 2017; 12: 123-130.
Smith E A, Marshall J G, Selph S S, Barker D R, Sedgley C M. Nonsteroidal anti-inflammatory drugs for managing postoperative endodontic pain in patients who present with preoperative pain: a systematic review and meta-analysis. J Endod 2017; 43: 7-15.
Parirokh M, Yosefi M H, Nakhaee N, Manochehrifar H, Abbott P V, Reza Forghani F. Effect of bupivacaine on postoperative pain for inferior alveolar nerve block anaesthesia after single-visit root canal treatment in teeth with irreversible pulpitis. J Endod 2012; 38: 1035-1039. DOI: 10.1016/j.joen.2012.04.012.
Hou X M, Su Z, Hou B X. Post endodontic pain following single-visit root canal preparation with rotary vs reciprocating instruments: a meta-analysis of randomized clinical trials. BMC Oral Health 2017; 17: 86.
Farzaneh S, Parirokh M, Nakhaee N, Abbott P V. Effect of two different concentrations of sodium hypochlorite on postoperative pain following single-visit root canal treatment: a triple-blind randomized clinical trial. Int Endod J 2018; 51 Suppl 1: e2-e11.
Gambarini G, Testarelli L, De Luca M et al. The influence of three different instrumentation techniques on the incidence of postoperative pain after endodontic treatment. Ann Stomatol (Roma) 2013; 4: 152-155.
Singh RD1, Khatter R, Bal R K, Bal C S, Intracanal medications versus placebo in reducing postoperative endodontic pain-a double-blind randomized clinical trial. Braz Dent J 2013; 24: 25-29.
Cohen, S. Endodontic emergenicies. In Cohen S, Burns R C Pathways of the pulp. 2nd ed. p. 31. St Louis: C.V Mosby Co, 1980.
Jostes J L, Holland G R. The effect of occlusal reduction after canal preparation on patient comfort. J Endod 1984; 10: 34-7.
Creech J L 3rd, Walton R E, Kaltenbach R. Effect of occlusal relief on endodontic pain. J Am Dent Assoc 1984; 109: 64-67.
Rosenberg P A, Babick P J, Schertzer L, Leung A. The effect of occlusal reduction on pain after endodontic instrumentation. J Endod 1998; 24: 492-496.
Parirokh M, Rekabi A R, Ashouri R, Nakhaee N, Abbott P V, Gorjestani H. Effect of occlusal reduction on postoperative pain in teeth with irreversible pulpitis and mild tenderness to percussion. J Endod 2013; 39: 1-5.
Ashgar S, Fatima F, Ali A. Occlusal reduction reduces postopertative pain after endodontic instrumentation. Pakistan Oral Dent J 2014; 34: 539-542.
Sheikh H, Ahmed M A, Jouhar R Choudhry Z. Comparioson of psot instrumentation pain in teeth during root canal treatment with or without occlusal reduction. Pakistan Oral Dent J 2015; 35: 699-701.
Zeidan B M. Evaluation the effect of occlusal reduction on postoperative pain in teeth with irreversible pulpitis and mild tenderness to percussion. Journal of Al Rafidain University College 2016; 38: 128-140.
Arslan H, Seckin F, Kurklu D, Karatas E, Yanikoglu N, Capar I D. The effect of various occlusal reduction levels on postoperative pain in teeth with symptomatic apical periodontitis using computerized analysis: a prospective, randomized, double-blind study. Clin Oral Investig 2017; 21: 857-863.
What is GRADE? BMJ Best Practice Tools. Available online at https://bestpractice.bmj.com/info/toolkit/learn-ebm/what-is-grade/ (accessed 24 August 2018).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Balevi, B. Managing post endodontic treatment pain by eliminating occlusal contacts. Evid Based Dent 20, 109–110 (2019). https://doi.org/10.1038/s41432-019-0055-0
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41432-019-0055-0